Last Updated on December 1, 2025 by Bilal Hasdemir

Nearly 250,000 people have brain surgery every year in the United States. Many of them need to stay in the Intensive Care Unit (ICU) after surgery craniotomy.
The time spent in the ICU after brain surgery can vary a lot. This depends on how complex the craniotomy for brain tumor surgery is. It also depends on the patient’s health.
Knowing how long someone might stay in the ICU can help. It helps patients and their families get ready for what comes after surgery.
Key Takeaways
- The length of ICU stay after brain surgery varies based on the complexity of the procedure.
- Factors such as the patient’s overall health and age influence ICU stay duration.
- Post-surgery care involves close monitoring and management of possible complications.
- Understanding the typical ICU stay can help patients and families prepare.
- The complexity of neurosurgery plays a significant role in determining ICU stay.
Understanding Brain Surgery and Craniotomy
Brain surgery is a complex medical procedure. It involves different techniques, with craniotomy being a key one. It’s important to understand brain surgery, and craniotomy in particular.
What Is a Craniotomy?
A craniotomy is a surgery where part of the skull is removed. This lets neurosurgeons do various brain operations. These include brain tumor removal and cerebral tumor surgery.
Common Reasons for Brain Surgery
Brain surgery is done for many important reasons. These include:
- Removing brain tumors
- Relieving pressure on the brain
- Fixing aneurysms or AVMs
- Treating epilepsy
- Removing blood clots or foreign objects
Types of Brain Surgical Procedures
There are many types of brain surgeries. Each has its own reasons and methods:
- Craniotomy: This involves temporarily removing a part of the skull.
- Biopsy: It’s about taking a sample of brain tissue for tests.
- Aneurysm Clipping: This treats aneurysms by clipping the neck of the aneurysm.
- Deep Brain Stimulation: It involves putting electrodes in the brain to treat movement disorders.
Knowing about brain surgery and craniotomy helps patients and families. It makes understanding neurosurgical procedures easier.
The Typical ICU Stay After Brain Surgery
Staying in the ICU after brain surgery is a key part of getting better. How long you stay depends on your needs and the surgery type. The ICU is where doctors watch you closely and fix any problems fast.
Average Duration in Intensive Care
How long you stay in the ICU can vary. It can be a few days or more than a week. Things that affect this time include how complex the surgery was, your health before surgery, and how well you’re recovering. Some people might leave sooner if they get better fast, while others need more time.
Why ICU Monitoring Is Necessary
Monitoring in the ICU is vital after brain surgery. It helps doctors catch and fix problems early. Watching your vital signs and brain function closely is key to keeping you safe and helping you heal well.
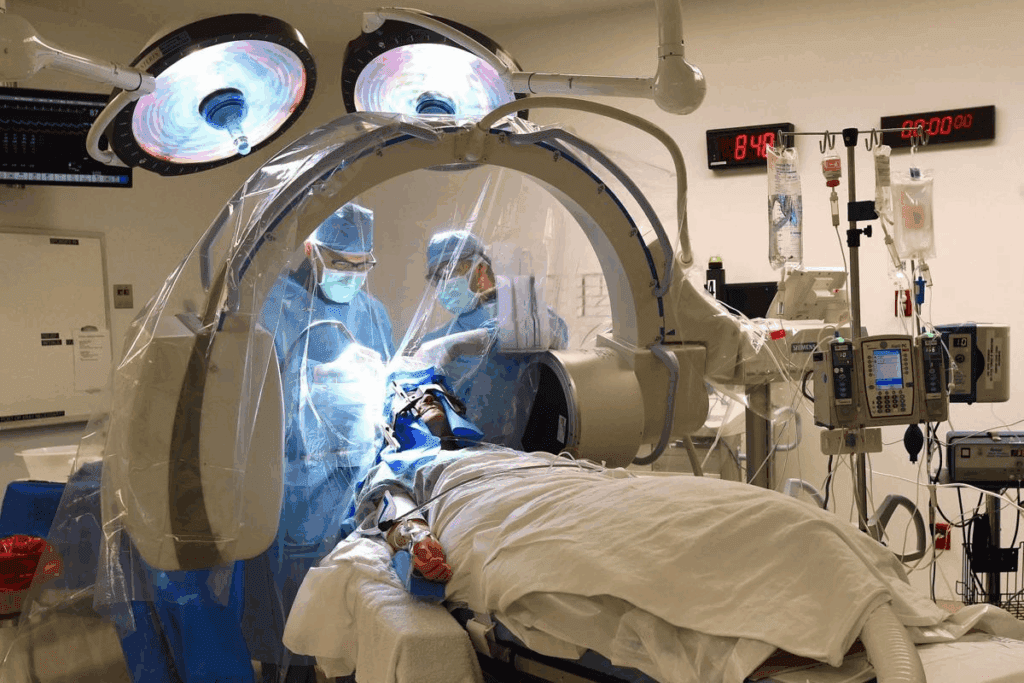
Transition from Operating Room to ICU
Going from the operating room to the ICU is a big step. After surgery, you move to the ICU where a special team takes care of you. This team knows how to handle neurosurgery patients and is ready for any challenges.
Good communication between the surgery team and ICU staff is important. It makes sure you get the best care all the way through your recovery. Knowing about ICU stays after brain surgery helps you and your family get ready for the next steps in your healing.
Factors That Influence ICU Length of Stay
The time a patient stays in the ICU after brain surgery can change a lot. Knowing what affects this time is key for patients and their families. It helps them understand what to expect during their recovery.
Complexity of the Surgical Procedure
The type and complexity of brain surgery matter a lot. More complex surgeries or those with higher risks need longer watch times. For example, brain tumor removal or aneurysm clipping can vary in complexity, affecting how long a patient stays in the ICU.
Pre-existing Health Conditions
What health issues a patient has before surgery can really affect their recovery. Problems like diabetes, heart disease, or COPD can make recovery harder. It’s important to manage these conditions well to help the patient recover faster.
Age and Overall Health Status
A patient’s age and health also play big roles. Older patients or those in poor health might need more time to get better. The medical team looks at these factors to make a care plan that fits the patient’s needs.
Surgical Complications
Surgical complications, like intracranial hemorrhage or cerebral edema, can happen during or after surgery. They often mean a longer stay in the ICU for careful watching and treatment. Quick action to treat these issues is key to avoiding more problems.
Any of these factors can make recovery harder. This shows why care in the ICU needs to be tailored to each patient’s needs.
The First 24 Hours in ICU After Craniotomy
The first day in the ICU after brain surgery is very important. It’s a time of close monitoring and care. This helps prevent and manage any problems that might arise.
Immediate Post-operative Monitoring
When patients arrive in the ICU, they are hooked up to many devices. These track their heart rate, blood pressure, and oxygen levels. Continuous monitoring lets doctors spot any issues quickly and act fast.
Neurological Assessments
Doctors do neurological assessments often. They check how awake the patient is, their thinking, and their brain function. These checks help find problems early, like swelling in the brain or bleeding.
Pain Management Protocols
Managing pain well is key after surgery. The ICU team uses different methods, like medicines and other treatments. They aim to keep the patient comfortable and avoid any extra problems.
Ventilation and Respiratory Support
Many patients need ventilation and respiratory support after a craniotomy. This helps them breathe properly until they can do it on their own. It keeps their oxygen and carbon dioxide levels just right.
The care given in the first 24 hours in the ICU is vital for recovery. By watching the patient closely and fixing any problems right away, doctors can help them get better faster.
Medical Monitoring in the Neurosurgical ICU
Medical monitoring in the neurosurgical ICU is key for patients after brain surgery. The ICU has advanced tech and a team ready for neurosurgical patients’ complex needs.
Intracranial Pressure Monitoring
Monitoring intracranial pressure (ICP) is vital in the ICU. It checks the skull’s pressure, which can rise due to swelling or bleeding. High ICP can cause more brain damage if not treated fast. show how important ICP monitoring is for making treatment plans.
Vital Signs and Neurological Checks
Keeping an eye on vital signs like blood pressure and heart rate is essential. Neurological checks also happen often. They look at consciousness, pupil size, and limb strength. These help spot any neurological problems early.
Brain Oxygen and Blood Flow Monitoring
It’s important to watch brain oxygen and blood flow. This ensures the brain gets enough oxygen and nutrients. Tools like jugular venous oximetry and cerebral blood flow monitoring help understand the brain’s health.
Seizure Monitoring and Management
Seizures can happen after brain surgery. It’s important to catch and manage them quickly. EEG monitoring catches seizures, and medicines are given as needed.
The detailed monitoring in the ICU is critical for patients after brain surgery. It lets doctors act fast if the patient’s condition changes. This helps improve patient outcomes.
Common Complications That May Extend ICU Stay
Patients who have had brain surgery in the ICU face many risks. These can affect their recovery. The ICU team watches closely for any issues that might make their stay longer.
Cerebral Edema (Brain Swelling)
Brain swelling, or cerebral edema, is a common issue after brain surgery. It happens when fluid builds up in the brain, causing pressure. Managing brain swelling includes using medicines like corticosteroids. Sometimes, surgery is needed to relieve pressure.
- Monitoring intracranial pressure
- Administration of osmotic diuretics
- Maintaining optimal head elevation
Intracranial Hemorrhage
Intracranial hemorrhage, or bleeding in the skull, is a serious problem after brain surgery. It needs quick medical help. The management of bleeding in the brain might include surgery to remove the blood or other treatments to stop bleeding.
Infection Risks and Management
Infections are a big risk after brain surgery, even more so in the ICU. Infection risks include meningitis, ventriculitis, and infections at the surgery site. To manage these, doctors use antibiotics and follow strict infection control. They also watch for signs of infection.
| Infection Type | Prevention Measures | Treatment Options |
| Meningitis | Vaccination, Sterile technique | Antibiotics |
| Surgical Site Infections | Preoperative antibiotics, Wound care | Antibiotics, Surgical debridement |
Seizures and Neurological Deficits
Seizures and neurological problems can happen after brain surgery. To manage seizures, doctors use special drugs. Neurological issues might need rehabilitation. Monitoring for changes in the brain is key in the ICU to catch and treat problems early.
The ICU team works hard to prevent these complications. They do this by closely watching patients and acting quickly. Knowing about these risks and how to manage them helps patients and their families during recovery.
ICU Care for Specific Types of Brain Surgery
Different brain surgeries need special ICU care. This care depends on the surgery type, the patient’s health, and possible complications after surgery.
Tumor Resection Recovery
Patients after tumor removal surgery are closely watched in the ICU. They are checked for any signs of brain problems or swelling. They also get regular checks on their brain pressure and watch for infections or bleeding.
Aneurysm Clipping or Coiling
Patients with aneurysm clipping or coiling need special ICU care. They are watched closely for signs of bleeding or blood vessel problems. It’s important to keep an eye on their brain and body signs. The team also works to control blood pressure and prevent blood vessel narrowing.
Traumatic Brain Injury Surgery
Patients with TBI face complex ICU care. They might have other injuries and are at risk for brain damage. The ICU team checks their brain pressure, manages pain and agitation, and makes sure their brain gets enough blood. They also take care of other injuries and support the patient’s recovery.
Epilepsy Surgery
Epilepsy surgery patients are watched for seizures and possible complications. The ICU team works with neurologists and neurosurgeons to manage their medication and adjust treatment plans. They might use EEG to watch for seizures.
In summary, ICU care for brain surgery patients is very specific. It depends on the surgery and the patient’s health. Understanding these needs helps healthcare providers give better care and improve patient outcomes.
The Role of the Neurocritical Care Team
The success of brain surgery depends a lot on the neurocritical care team. This team is key in managing patients after surgery. They make sure patients get the best care for a good recovery.
Neurosurgeons and Neurointensivists
Neurosurgeons and neurointensivists are vital to the team. Neurosurgeons do the surgery and watch over the patient’s surgical care. Neurointensivists focus on the intensive care of very sick neurological patients. They work together to keep an eye on the patient, handle any problems, and decide on the best care.
Working together, neurosurgeons and neurointensivists meet the complex needs of patients after brain surgery. Their knowledge ensures patients get care that fits their needs perfectly.
Specialized ICU Nursing Care
ICU nursing care is also critical. ICU nurses are trained to care for very sick patients, like those after brain surgery. They watch the patient’s vital signs, manage pain, and follow the care plans made by the team.
ICU nurses play a huge role in the team. They are often the first to care for patients in the ICU, providing constant support and monitoring.
Multidisciplinary Approach to Recovery
For patients to recover well after brain surgery, a team effort is needed. The team includes neurosurgeons, neurointensivists, ICU nurses, physical therapists, and more. They work together to create a care plan that covers all aspects of the patient’s needs.
| Team Member | Role |
| Neurosurgeons | Perform surgery and oversee surgical care |
| Neurointensivists | Provide intensive care to critically ill neurological patients |
| ICU Nurses | Provide high-level care, monitor vital signs, and manage pain |
| Physical Therapists | Assist with physical rehabilitation and mobility |
The multidisciplinary approach makes sure all parts of recovery are covered. This leads to better results and a smoother move from the ICU to other care settings.
Transitioning from ICU to Regular Hospital Care
When a patient moves from the ICU to regular hospital care, it’s a big step in their recovery. This change shows the patient is stable enough to leave the ICU. But, they need to keep getting monitored and cared for.
Criteria for ICU Discharge
There are key factors that decide when a patient can leave the ICU. These include:
- Stable vital signs and neurological status
- Minimal need for life-supporting therapies
- Adequate pain management
- Ability to breathe without mechanical ventilation
When these conditions are met, the healthcare team thinks the patient is ready for a less intense care setting.
Step-Down Units and Intermediate Care
Before moving to a regular hospital floor, many patients go to step-down units or intermediate care. These places offer less intense care than the ICU but keep a close eye on the patient.
Benefits of Step-Down Units:
- Continued close monitoring of vital signs and neurological status
- Intervention capabilities for any complications
- Support for patients not yet ready for regular floor care
Continued Monitoring on Regular Floors
On a regular hospital floor, patients keep getting medical care and monitoring, but at a less intense level. Nurses and healthcare professionals watch their vital signs, manage pain, and look for any complications.
The table below shows the typical care progression after brain surgery:
| Care Setting | Level of Care | Typical Duration |
| ICU | Intensive care, close monitoring | 1-3 days |
| Step-Down/Intermediate Care | Less intensive, continued monitoring | 2-5 days |
| Regular Hospital Floor | Standard care, ongoing monitoring | Variable, typically several days |
Family Experience During the ICU Stay
It’s important for families to know what the ICU is like after brain surgery. The ICU is a place where patients get very close care. It can be tough for families to get used to, but knowing what to expect helps a lot.
Visitation Policies in Neurosurgical ICU
Every hospital has its own rules for visiting in the neurosurgical ICU. Most try to let families visit while keeping the area calm and clean for the patient. Visiting hours are usually set, and only a few people can be with the patient at a time. Families should ask about these rules when they arrive.
Some hospitals let families visit more freely, but even then, the ICU staff might limit visits during certain times or when the patient needs quiet. It’s good to check with the hospital about this.
Communication with the Medical Team
Talking well with the medical team is key for families. They should get regular updates on the patient’s health and treatment plans. This helps families feel less worried and unsure.
Having a family meeting is also important. The medical team talks about the patient’s health, what might happen, and how they will be cared for. This meeting helps families understand the situation better and make decisions together.
Supporting a Loved One in Neuro ICU
Helping a loved one in the neuro ICU means giving emotional support and practical help. Families can help a lot by being there, reassuring the patient, and helping with simple things when they can.
| Support Strategies | Description |
| Emotional Support | Being present, holding hands, and talking to the patient can provide comfort and reassurance. |
| Practical Assistance | Helping with daily needs, such as feeding or personal care, under the guidance of ICU staff. |
| Advocacy | Communicating with the healthcare team on behalf of the patient to ensure their needs are met. |
By knowing the visitation rules, talking well with the medical team, and supporting their loved one, families can make the ICU stay better. They can help a lot in the patient’s recovery.
Early Rehabilitation Efforts in the ICU
The intensive care unit (ICU) is more than just critical care. It’s where early rehabilitation for brain surgery patients starts. Early rehab is key to recovery, helping patients regain strength, function, and independence.
Physical Therapy Interventions
Physical therapy in the ICU helps patients recover from brain surgery. Early mobilization is a big part, getting patients moving safely. This includes:
- Range of motion exercises to keep flexibility
- Progressive mobilization to boost strength and balance
- Gait training to help patients walk again
Occupational Therapy Assessments
Occupational therapists check if patients can do daily tasks. They work on getting these skills back. Occupational therapy interventions are made for each patient. They might include:
- Cognitive rehab to enhance memory and problem-solving
- Adaptive equipment training for daily tasks
- Strategies to improve fine motor skills
Speech and Swallowing Evaluations
Speech-language pathologists are vital for speech and swallowing issues. Swallowing evaluations are key to ensure safe eating and drinking. These might include:
- Bedside swallowing assessments
- Instrumental assessments like videofluoroscopic swallow studies
- Speech therapy to enhance communication skills
Early rehab in the ICU is a team effort that greatly affects recovery. By tackling physical, occupational, and speech therapy early, patients have a better shot at full recovery.
Preparing for Hospital Discharge After Brain Surgery
Patients recovering from brain surgery look forward to going home. This time brings both excitement and worries about what’s next. The path to leaving the hospital includes several important steps, like how long they stay, planning for discharge, and choosing care after they go home.
Typical Hospital Length of Stay
The time a patient stays in the hospital after brain surgery varies. It depends on the surgery’s complexity, the patient’s health, and any complications. Usually, patients stay for a few days to a week or more.
Several things affect how long a patient stays in the hospital:
- The type and complexity of the brain surgery
- Any health issues the patient had before surgery
- The patient’s age and health
- Any problems that come up during or after surgery
Discharge Planning Process
Discharge planning starts soon after a patient is admitted. It’s about figuring out what care they’ll need after leaving the hospital. This might include:
- Checking the patient’s physical and mental health
- Deciding if they need ongoing medical care or therapy
- Finding the best place for them to go after the hospital
A good discharge plan helps patients move smoothly from the hospital to their next care setting. This reduces the chance of them having to go back to the hospital.
Home Care vs. Rehabilitation Facility
Choosing between home care and a rehabilitation facility is a big part of discharge planning. The decision depends on the patient’s needs and situation.
| Care Setting | Characteristics | Suitability |
| Home Care | Care in the patient’s home, which might include nursing, physical therapy, and help with daily tasks. | Good for patients with a supportive home and simpler needs. |
| Rehabilitation Facility | Specialized care and therapy in a place focused on helping patients get back to normal. | Best for patients needing a lot of therapy or have more complex health issues. |
Choosing the right place for care after the hospital is key for a successful recovery. It ensures the patient gets the right level of care.
Long-term Recovery Timeline After Brain Surgery
Recovering from brain surgery is a long journey. It goes beyond just the time spent in the hospital. Understanding the recovery timeline helps manage expectations and improves outcomes. The recovery time varies for each person, based on the surgery type, health, and any complications.
First Weeks After Discharge
The first weeks after leaving the hospital are key. Patients need to follow a strict plan that includes taking medicine, attending follow-up visits, and slowly getting back to activities. Rest and avoiding hard activities are very important during this time. As one neurosurgeon says,
“The first few weeks are about healing and adjusting to any changes brought about by the surgery.”
During this time, patients might feel tired, have headaches, or notice changes in thinking. It’s important to watch these symptoms and talk to their healthcare provider about any worries.
One to Three Months Post-Surgery
As patients move into the one to three months after surgery, they often see big improvements. Rehabilitation efforts become more focused. Physical, occupational, and speech therapy help regain lost functions and adapt to changes. A study in a medical journal says,
“Most patients show notable recovery within the first three months, with continued improvement thereafter.”
Six Months to One Year Recovery
By six months to one year after surgery, many patients have made big strides. This time is marked by continued neurological recovery and adaptation. Patients can usually do most of their daily activities, but some may have lasting effects from the surgery or their condition.
It’s important to keep up with follow-up appointments with the neurosurgical team during this phase. They help monitor progress and address any ongoing concerns.
Long-term Outcomes and Follow-up
The long-term results after brain surgery depend on many factors. These include the surgery type, the patient’s health, and any complications after surgery. Long-term care is key to managing late effects and watching for any return of the condition that led to surgery.
- Regular check-ups with the neurosurgeon
- Imaging studies as recommended
- Management of any ongoing symptoms or side effects
“Long-term follow-up is critical for the best outcomes and ensuring patients get the care they need throughout their recovery.”
Special Considerations for Different Patient Populations
Caring for patients in the neuro ICU needs a deep understanding of different groups. Each age and health condition requires a special care plan. This ensures the best results for everyone.
Pediatric Patients in Neuro ICU
Pediatric patients need special care because their brains and bodies are growing. A study in shows that their care must consider their development.
The team in the neuro ICU must handle the unique challenges of kids. This includes pain management and neurological monitoring. Experts say, “Caring for critically ill kids needs a team effort, focusing on their special needs.”
“The management of pediatric patients in the ICU is a complex task that requires a deep understanding of pediatric physiology and pathology.”
| Consideration | Pediatric Patients |
| Neurological Monitoring | Requires specialized equipment and expertise |
| Pain Management | Must be tailored to the patient’s age and weight |
| Family Support | Crucial for the patient’s emotional well-being |
Elderly Patients and Extended Recovery
Elderly patients face extra challenges after brain surgery. These include health problems and less ability to recover. The neuro ICU team must understand these factors.
Comprehensive geriatric assessment is key for elderly patients. It looks at their physical health, mental state, and social support.
- Careful monitoring of vital signs and neurological status
- Management of comorbid conditions
- Early mobilization and rehabilitation
Patients with Pre-existing Conditions
Patients with health issues like diabetes or high blood pressure need careful management in the neuro ICU. These conditions can affect their recovery and must be watched closely.
Having pre-existing conditions can make recovery harder. The neuro ICU team must tailor care to manage these conditions well. This helps improve patient outcomes.
Conclusion
Knowing how long you’ll stay in the ICU after brain surgery is key. Recovery after a craniotomy or other neurosurgery can be complex. It changes a lot from one person to another.
Things like the surgery type, your health before surgery, and any complications can affect your stay. The team of neurosurgeons and neurointensivists work together. They provide the care and watch you closely during this time.
Understanding what affects your ICU stay and recovery time helps you prepare. Talking well with your medical team and having support are key to a good recovery. They help a lot in getting better after brain surgery.
Getting good results from neurosurgery needs skilled care, careful monitoring, and a solid recovery plan. These are all important for the best outcome after brain surgery and craniotomy.
FAQ
What is a craniotomy?
A craniotomy is a surgery where a part of the skull is removed. This lets doctors access the brain.
How long do patients typically stay in the ICU after brain surgery?
The ICU stay varies. It depends on the surgery type, its complexity, and the patient’s health.
Why is ICU monitoring necessary after brain surgery?
Monitoring is key to watch the patient’s brain health. It helps manage pain and spot any issues early.
What are the common complications that can prolong ICU stay?
Complications like swelling, bleeding, infections, and seizures can extend the stay.
How is intracranial pressure monitored in the ICU?
Pressure is checked with special devices. This lets doctors act fast if there’s a change.
What is the role of the neurocritical care team in managing patients after brain surgery?
The team, including neurosurgeons and ICU nurses, provides care. They manage complications together.
When can patients be discharged from the ICU after brain surgery?
Patients leave the ICU when they’re stable. They no longer need constant care.
What is the typical hospital length of stay after brain surgery?
Stay varies. Most patients are in the hospital for days to weeks, based on their needs.
What are the options for care after hospital discharge?
Patients might go home or to a rehab facility. It depends on their health and the doctor’s advice.
How long does it take to recover from brain surgery?
Recovery time varies. Most patients take weeks to months to fully heal.
Are there special considerations for different patient populations after brain surgery?
Yes, kids, older adults, and those with health issues need special care.
What is the long-term recovery timeline after brain surgery?
Recovery can take a year or more. Most patients see big progress in the first year.
How much does brain surgery cost?
Costs vary. It depends on the surgery, location, and insurance.
Are you awake during brain surgery?
Some surgeries, like awake craniotomy, require being awake. Others use general anesthesia.
What is the success rate of brain tumor surgery?
Success rates vary. It depends on the tumor type, location, and the patient’s health.
Can brain surgery cause long-term effects?
Surgery can lead to long-term effects. This includes cognitive or neurological issues, depending on the surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11729059/





