Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 30% of patients who have craniotomy surgeries need help with pain and other symptoms after. We know that having a craniotomy is scary. The right anesthesia and post-operative care are key for a good outcome.Learn the essential craniotomy medications used for pain, swelling, and seizure prevention after the procedure clearly.
During a craniotomy, doctors use different anesthesia for craniotomy to keep patients comfortable. After the surgery, post-craniotomy medication helps with pain and prevents problems. We’ll talk about the craniotomy pain relief and other medicines used before and after the surgery.
It’s important for patients to know about the craniotomy drugs they might get. We aim to give full care and support every step of the way.
Key Takeaways
- Various medications are used before, during, and after craniotomy to manage symptoms and improve patient comfort.
- Anesthesia is very important in craniotomy surgeries.
- Medication after craniotomy is key for pain management and avoiding complications.
- Knowing about craniotomy pain relief is crucial for good care after surgery.
- We offer full support to patients going through craniotomy.
The Craniotomy Procedure: An Overview
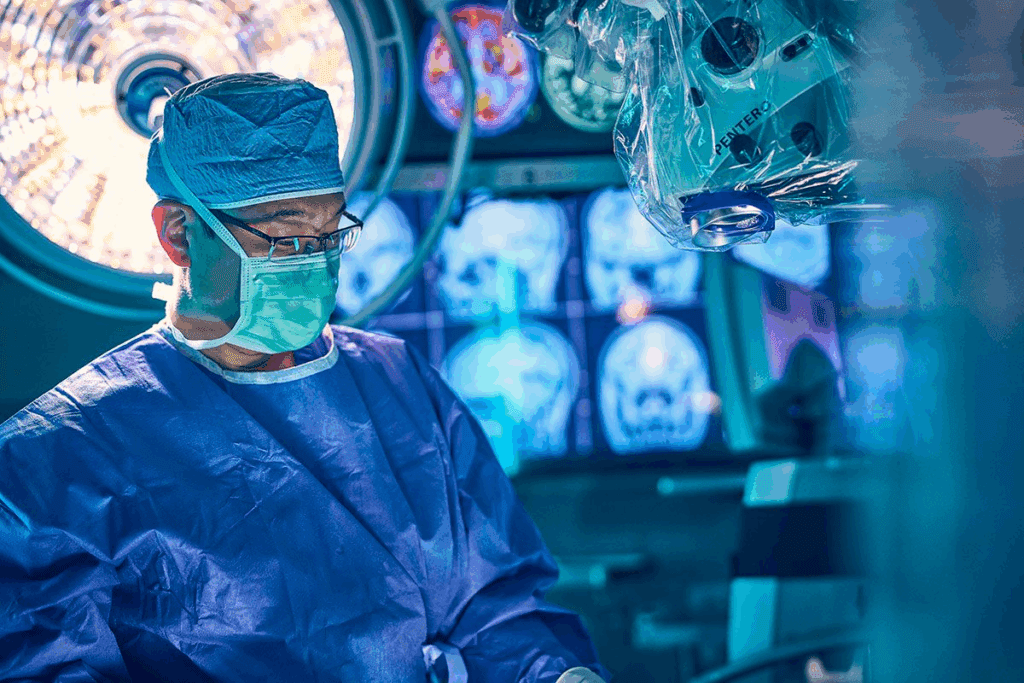
For many, a craniotomy can seem scary. But knowing what to expect can ease worries. A craniotomy is a surgery where part of the skull is taken off to reach the brain. It’s done for many reasons, like removing tumors or easing brain pressure.
Definition and Common Reasons for Craniotomy
A craniotomy is a surgery where a part of the skull is removed. This lets surgeons get to the brain. It’s done for many reasons, like:
- Removing brain tumors or cysts
- Relieving pressure on the brain caused by trauma or swelling
- Repairing aneurysms or arteriovenous malformations (AVMs)
- Draining abscesses or other infected areas
Surgical Preparation Including Head Shaving
Getting ready for a craniotomy involves several steps. Sometimes, head shaving is needed to keep the area clean. The amount of shaving depends on the surgery and the doctor’s choice. Patients also get instructions on what to do before surgery, like stopping certain medicines and using special soap.
Types of Craniotomy Procedures
There are different types of craniotomy surgeries, each for a specific reason:
- Standard Craniotomy: The traditional method where a section of the skull is removed.
- Keyhole Craniotomy: A minimally invasive technique where smaller incisions are made.
- Awake Craniotomy: Performed while the patient is awake to monitor brain functions.
Knowing about these types of surgeries helps patients feel more prepared. It can reduce anxiety and lead to better results.
Pre-Operative Medication Protocol
The pre-operative medication protocol is key in getting patients ready for craniotomy surgery. It aims to lower risks, make patients comfortable, and improve surgery results.
Medications for Pre-Surgical Preparation
Before a craniotomy, patients take certain meds to get ready. These meds are picked based on the patient’s health, the surgery type, and other important details.
Pre-surgical preparation medications include drugs to calm anxiety, stop infections, and manage health issues that might affect the surgery.
Anti-Anxiety Medications Before Surgery
Anti-anxiety meds are given before craniotomy surgery to help patients relax. These meds make the patient’s experience better and keep them calm before surgery.
Common anti-anxiety medications are benzodiazepines, like midazolam, which calm the patient down.
Pre-Operative Antibiotics
Pre-operative antibiotics are vital for craniotomy surgery. They prevent infections at the surgical site, which could be a big problem.
The choice of pre-operative antibiotics depends on the surgery type and patient allergies. Broad-spectrum antibiotics like cefazolin are often used.
| Medication Type | Purpose | Examples |
| Anti-Anxiety Medications | Reduce anxiety and stress before surgery | Midazolam, Lorazepam |
| Pre-Operative Antibiotics | Prevent surgical site infections | Cefazolin, Vancomycin |
| Other Pre-Surgical Medications | Manage other health conditions and prepare for surgery | Varies based on patient condition |
Knowing the pre-operative medication protocol helps patients prepare for craniotomy surgery. It ensures their safety and comfort.
Anesthesia Options for Craniotomy
It’s important for patients to know about anesthesia options for craniotomy surgery. Anesthesia is key to keeping patients comfortable and safe during these complex surgeries.
General Anesthesia Medications
General anesthesia is often used for craniotomy surgeries. It makes the patient unconscious and pain-free during surgery. Propofol and sevoflurane are common medications used. They are chosen based on the patient’s health and the surgery’s needs.
General anesthesia helps the surgical team control the patient’s vital signs. It also keeps the patient still during the surgery.
Local Anesthesia for Awake Craniotomy
In some cases, an awake craniotomy is done. The patient stays awake and can talk to the surgical team. Local anesthesia numbs the scalp and surgery area, keeping the patient comfortable.
This method is good for surgeries near brain areas that control important functions. It lets the team watch the patient’s responses in real-time.
Sedatives Used During the Procedure
Sedatives are used with local anesthesia in awake craniotomies to relax the patient. Midazolam and dexmedetomidine are examples. The sedation level is adjusted to keep the patient comfortable and able to respond.
The choice of sedation is made with care to avoid risks and keep the patient safe.
Intraoperative Medication Management
During a craniotomy, the right medications are key to keeping patients safe and improving surgical results. It’s important to manage medications well to protect the brain and keep vital signs stable. This helps avoid complications.
Brain-Protective Medications
These medications lower the risk of brain injury during surgery. They help keep the brain well-oxygenated and perfused. Thiopental and propofol are often used for their brain-protective effects.
These drugs work by reducing the brain’s need for oxygen. This is crucial during times of possible brain injury or when there’s a risk of ischemia.
Blood Pressure Control Medications
Keeping blood pressure in check is vital during surgery. It ensures the brain gets enough blood and prevents sudden spikes in blood pressure that could cause bleeding. Vasoactive medications like labetalol and nicardipine are used to control blood pressure.
It’s important to keep blood pressure stable to avoid problems like too little or too much blood to the brain. The right medication is chosen based on the patient’s needs and the surgery.
Anti-Seizure Prophylaxis During Surgery
Preventing seizures is a big part of care during craniotomy, especially with brain tumors or vascular issues. Anticonvulsants like levetiracetam (Keppra) are given to stop seizures.
Whether to use seizure prevention depends on the patient’s risk, the surgery type, and the neurosurgeon’s choice. It’s also important to watch for any side effects of these drugs.
| Medication Category | Examples | Purpose |
| Brain-Protective | Thiopental, Propofol | Reduce cerebral metabolic rate, provide neuroprotection |
| Blood Pressure Control | Labetalol, Nicardipine | Maintain stable blood pressure, prevent hypertensive surges |
| Anti-Seizure Prophylaxis | Levetiracetam (Keppra) | Prevent seizures during and after surgery |
Craniotomy Medications for Different Conditions
Craniotomy procedures need specific medications based on the condition being treated. The right medications can greatly affect the surgery’s success and the patient’s recovery. We’ll look at the medications for various conditions that require craniotomy.
Medications for Tumor-Related Craniotomies
Tumor-related craniotomies remove brain tumors, which can be benign or malignant. Medications are key for managing swelling, preventing seizures, and keeping the patient comfortable.
Corticosteroids, like dexamethasone, help reduce peritumoral edema and ease symptoms from tumor pressure. Anti-seizure medications such as levetiracetam prevent seizures, a common issue with brain tumors.
Medications for Trauma-Related Craniotomies
Trauma-related craniotomies treat injuries like epidural or subdural hematomas. The focus is on managing pressure, preventing infection, and supporting neurological health.
Osmotic diuretics like mannitol lower intracranial pressure by reducing brain fluid. Antibiotics prevent infection, a big risk in trauma cases. Sedatives help keep the patient calm and comfortable after surgery.
Medications for Vascular Abnormality Procedures
Vascular abnormalities, such as aneurysms or arteriovenous malformations (AVMs), need careful medication management during craniotomy. The aim is to keep blood pressure stable, prevent vasospasm, and ensure proper blood flow to the brain.
Nimodipine helps prevent vasospasm in patients with aneurysmal subarachnoid hemorrhage. Antihypertensive medications control blood pressure and lower the risk of bleeding or re-bleeding. We monitor the patient’s blood pressure closely to adjust medications as needed.
Immediate Post-Operative Pain Management
After a craniotomy, managing pain is key. It’s not just about comfort. It also helps prevent problems and aids in recovery.
Experts suggest using a mix of pain treatments. This includes both opioid and non-opioid drugs. It helps control pain well and lowers risks.
Opioid Analgesics
Opioids are often used for pain after a craniotomy. They work well for strong pain. But, we must watch for side effects like breathing problems and addiction.
“Opioids are still important for acute pain after neurosurgery,” says recent advice. We aim to use the least amount needed for the shortest time.
Non-Opioid Pain Relief Options
Non-opioid drugs are also important. They include things like acetaminophen and NSAIDs. They’re good for less severe pain.
Using these drugs can lessen opioid side effects. But, we must consider each patient’s situation and health history.
Local Anesthetic Infiltration
Local anesthetic infiltration is another method. It involves injecting drugs directly into the surgery site. This helps with pain.
This method is very effective right after surgery. It’s often used with other treatments to work better.
In summary, managing pain after a craniotomy needs a variety of approaches. This includes opioids, non-opioid drugs, and local anesthetics. Knowing these options helps doctors create the best pain plans for each patient.
Anti-Seizure Medications After Craniotomy
After a craniotomy, doctors often give anti-seizure meds to prevent seizures. Seizures can happen after this surgery. So, these meds are key in caring for patients after surgery.
Common Anti-Epileptic Drugs
Many anti-epileptic drugs (AEDs) are used after a craniotomy. Levetiracetam (Keppra), phenytoin (Dilantin), and valproate (Depakote) are some examples. The right AED depends on the patient’s health, the surgery type, and the doctor’s choice.
Levetiracetam is popular because it has fewer side effects and doesn’t interact with many drugs. Phenytoin has been used for years but needs blood level checks to work right and avoid harm.
Duration of Anti-Seizure Therapy
How long you take anti-seizure meds depends on your risk. People with seizure history or surgery for tumors or malformations might need them longer.
Usually, these meds are taken for weeks to months after surgery. The exact time depends on your health and risk of seizures coming back.
Managing Side Effects of Anti-Seizure Medications
It’s important to manage side effects of these meds to keep patients happy and healthy. Common side effects are feeling tired, dizzy, or having trouble thinking.
To lessen these side effects, doctors might change the dose or switch to another med. Regular check-ups with your doctor are key to handling side effects and adjusting treatment as needed.
Knowing about anti-seizure meds after a craniotomy helps patients understand their care better. It also helps avoid more problems.
Corticosteroids and Anti-Inflammatory Drugs
Corticosteroids and anti-inflammatory drugs are key in post-craniotomy care. They help manage brain swelling, a common issue after surgery.
Role in Reducing Brain Swelling
Corticosteroids, like dexamethasone, are used to reduce brain swelling after craniotomy. They decrease inflammation and improve symptoms. Medical studies support their effectiveness in managing swelling.
Dosage and Duration of Steroid Therapy
The dosage and duration of corticosteroid therapy vary based on the patient’s condition and surgery type. A high dose is given first, then the dose is gradually reduced. This approach aims to minimize side effects while managing swelling.
| Condition | Initial Dose | Tapering Duration |
| Brain Tumor | 16 mg/day | 7-10 days |
| Trauma | 20 mg/day | 5-7 days |
| Vascular Abnormality | 12 mg/day | 10-14 days |
Tapering Protocols for Steroids
Tapering corticosteroids is important to avoid withdrawal and let the body produce cortisol naturally again. The tapering process involves gradually reducing the dose over several days or weeks. This depends on the initial dose and therapy duration.
We keep a close eye on patients during tapering to prevent swelling from coming back. We adjust the tapering schedule as needed.
Comprehensive Guide to Craniotomy Medications
Managing craniotomy patients well means knowing about different medicines. Choosing the right medicine is key before, during, and after surgery. This ensures the best results for the patient.
First-Line Medications After Surgery
Right after a craniotomy, the main goal is to control pain, stop infections, and avoid seizures. First-line medications are the first ones used to achieve these goals. For pain, opioids are often chosen because they work well. But, doctors watch their use because of possible side effects.
- Opioid analgesics like morphine and fentanyl are frequently used for pain control.
- Antibiotics such as cefazolin are administered to prevent surgical site infections.
- Anti-seizure medications like levetiracetam are used to prevent post-operative seizures.
Second-Line Treatment Options
If first-line treatments don’t work or aren’t right, second-line treatment options are looked at. These might include other ways to manage pain or different seizure medicines.
- For patients who can’t take opioids, non-opioid pain relievers like acetaminophen might be used.
- If the first seizure medicines don’t work, other options like phenytoin or valproate could be tried.
Medication Protocols Based on Patient Factors
Medicine plans are made just for each patient, based on things like age, health history, and why the craniotomy was needed. For example, someone with a history of seizures might need a special medicine plan.
- Elderly patients might need smaller doses because their kidneys work less well.
- Patients with a history of substance abuse need close watch on opioid use.
- Those having surgery for tumors might get corticosteroids to shrink swelling.
By making medicine plans that fit each patient, doctors can get better results and reduce problems.
Antibiotics for Infection Prevention
To lower the chance of infections after surgery, doctors give craniotomy patients antibiotics before the operation. These medicines are key to keeping patients safe as they heal.
Prophylactic Antibiotic Regimens
Antibiotics are given to stop infections from happening. They are broad-spectrum, meaning they fight many kinds of germs.
Doctors pick different antibiotics for each patient. This depends on the patient’s health, any allergies, and the surgery type.
| Antibiotic Type | Dose | Frequency |
| Cefazolin | 2g | Every 8 hours |
| Vancomycin | 1g | Every 12 hours |
| Metronidazole | 500mg | Every 8 hours |
Duration of Antibiotic Treatment
How long antibiotics are used depends on the patient and the surgery. Usually, they are given for 24 to 48 hours after surgery.
Monitoring how well the antibiotics work is very important. We change the treatment if needed to keep infections away.
Managing Antibiotic-Related Side Effects
Antibiotics are vital but can cause side effects. These include stomach problems, allergic reactions, and Clostridioides difficile infection.
We watch for these side effects closely. If needed, we change the antibiotics to reduce risks.
Medications for Specific Post-Craniotomy Complications
Managing complications after a craniotomy is key to better patient outcomes and faster recovery. Patients may face several issues that need immediate medical care. We’ll talk about the medications for these complications, helping patients understand what to expect and how these problems are tackled.
Drugs for Cerebral Edema Management
Cerebral edema, or brain swelling, is a common issue after a craniotomy. To tackle this, we often use corticosteroids, like dexamethasone. These drugs help by reducing brain swelling through inflammation reduction.
The amount and length of steroid treatment vary based on the swelling’s severity and the patient’s response. We start with a high dose and gradually reduce it as the swelling goes down. It’s important to watch for any side effects during this treatment.
Medications for Cerebrospinal Fluid Leaks
CSF leaks are another complication that can occur after a craniotomy. To handle these leaks, we might use drugs that lower CSF production, such as acetazolamide. This helps by reducing CSF pressure and aiding in the leak’s healing.
We also use antibiotics to prevent infections, which are a big risk with CSF leaks. The type of antibiotic and how long to use it depend on the patient’s condition and the leak’s severity.
Treatments for Post-Operative Nausea and Vomiting
Post-operative nausea and vomiting (PONV) are common after a craniotomy, affecting comfort and recovery. To manage PONV, we use ondansetron and metoclopramide. These drugs block the brain signals that cause nausea and vomiting.
A study found that ondansetron has greatly reduced PONV in post-craniotomy patients. We often use these medications with other methods, like staying hydrated and resting, to effectively manage PONV and improve patient outcomes.
Long-Term Medication Management
Managing medications long-term is key after a craniotomy. As patients move from the hospital to home, it’s vital to handle their meds well. This helps avoid problems and makes recovery smoother.
Transitioning from Hospital to Home Medications
Patients need to know their meds when they go home. Discharge instructions list all meds, how much, and when to take them. It’s important to follow this plan and talk to the doctor if you have questions.
Keeping a medication diary is a good idea. Write down when you take your meds and any side effects. This can help spot problems early and make needed changes.
Medication Adjustments During Recovery
Medication changes are common during recovery. Regular follow-up appointments with doctors are key. They help check how you’re doing and adjust your meds if needed.
Talking openly with your healthcare team is crucial. Share any changes in symptoms or side effects. This helps doctors adjust your meds to support your recovery.
Potential Lifelong Medication Requirements
Some patients may need meds for life after a craniotomy. This could include anti-seizure medications or other treatments. Knowing this is important for planning and sticking to your medication plan.
We help patients understand the importance of taking their meds as prescribed. We talk about possible side effects and how to deal with them. This prepares patients for their long-term care needs.
Conclusion
Knowing about the medicines used before, during, and after a craniotomy is key. We’ve looked at the different types of drugs used. These include those for getting ready for surgery, anesthesia, and care after surgery.
Recovering from a craniotomy means managing medicines well. This helps the healing process go smoothly. Medicines are used to control pain, prevent seizures, and lower swelling. This knowledge helps patients and their families during recovery.
Good care after a craniotomy means more than just medicine. It also includes regular check-ups and making lifestyle changes. It’s important to follow the doctor’s advice and go to all follow-up visits. This ensures the best recovery.
We aim to give top-notch care and support to our patients. Our goal is to help them get the best results from their surgery. We focus on personalized care for international patients getting advanced medical treatments.
FAQ
What medications are typically used before a craniotomy?
Before a craniotomy, patients often get antibiotics to prevent infection. They also get anti-anxiety meds to relax. These steps help prepare the patient and lower the risk of problems.
What types of anesthesia are used during a craniotomy?
Anesthesia types vary for craniotomies. General anesthesia is common, but local anesthesia is used for awake surgeries. Sedatives help the patient relax during surgery.
Why are brain-protective medications used during craniotomy?
These meds protect the brain from damage during surgery. They help reduce complications and improve outcomes.
How is pain managed after a craniotomy?
Pain management includes opioids, non-opioids, and local anesthetics. The choice depends on the patient’s needs and history.
Why are anti-seizure medications used after craniotomy?
These meds prevent seizures, a possible complication. The type used varies, but common drugs are prescribed.
What is the role of corticosteroids in managing brain swelling after craniotomy?
Corticosteroids reduce brain swelling. They decrease inflammation and relieve pressure, improving outcomes.
How are antibiotics used to prevent infection after craniotomy?
Antibiotics are given to prevent infection. The type and duration depend on the patient’s situation.
What medications are used to manage post-craniotomy complications?
Medications for complications include drugs for swelling, leaks, and nausea. They help manage post-surgery issues.
How are medications managed in the long term after craniotomy?
Long-term care involves transitioning to home meds and adjusting as needed. Sometimes, lifelong medication is required.
Do I need to shave my head before a craniotomy?
Shaving may be needed, depending on the surgery and surgeon. It ensures a clean site.
What is tonsuring or head shaving for medical procedures?
Tonsuring prepares the scalp for surgery. It reduces infection risk and clears the site.
Are there any specific medications used for craniotomy patients with tumors or vascular abnormalities?
Yes, specific meds are used for conditions like tumors or vascular issues. They manage these conditions during and after surgery.
Can I expect to be on pain relief medication after craniotomy?
Yes, pain meds are used to manage post-op pain. The type and duration vary based on individual needs.
How long will I need to take anti-seizure medications after craniotomy?
Anti-seizure treatment duration varies by patient. Your doctor will decide based on your risk factors and history.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5516779/