Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, thousands of people around the world have brain tumor removal surgery. Craniotomy surgery is a common method. It involves temporarily removing a part of the skull to reach the brain. This lets surgeons take out tumors that could harm a patient’s life and health.Learn what happens when a brain tumor is removed via craniotomy surgery. Understand the procedure and what to expect during recovery clearly.
Dealing with brain cancer treatment can be scary. But, thanks to neurosurgery progress, more people are living longer. We aim to give you all the details about craniotomy surgery. We want to help you through this tough time.
Key Takeaways
- Craniotomy surgery is a complex procedure for removing brain tumors.
- Advances in neurosurgery have improved patient outcomes.
- Understanding the process can help alleviate concerns.
- Brain tumor removal is a life-saving procedure.
- Comprehensive support is available for patients undergoing brain cancer treatment.
Understanding Brain Tumors

It’s important for patients to understand brain tumors. They can be either benign or malignant. Knowing the difference helps in planning treatment.
Types of Brain Tumors: Benign vs. Malignant
Benign tumors are not cancerous and don’t spread. They can cause problems if they grow too big. Malignant tumors are cancerous and spread, making treatment harder.
Brain tumors are classified by their cell type and behavior. Common types include gliomas, meningiomas, and acoustic neuromas. Gliomas can be low-grade or high-grade, with glioblastoma being the most aggressive.
| Tumor Type | Benign/Malignant | Common Symptoms |
| Gliomas | Both | Headaches, seizures, cognitive changes |
| Meningiomas | Usually Benign | Headaches, vision changes, hearing loss |
| Acoustic Neuromas | Benign | Hearing loss, tinnitus, balance issues |
Common Symptoms and Warning Signs
Symptoms of brain tumors vary. They include headaches, seizures, and memory loss. Weakness or numbness in parts of the body is also common.
These symptoms can also have other causes. If you’re experiencing them, see a doctor to find out why.
How Brain Tumors Are Detected
Imaging studies are used to find brain tumors. MRI and CT scans are the main tools. MRI gives detailed brain images, while CT scans are quicker and used in emergencies.
After finding a tumor, more tests may be needed. These tests help figure out the tumor’s type and grade. This info is key for treatment planning.
The Path to Diagnosis

Finding a brain tumor needs a mix of doctor checks and high-tech scans. This process is key to picking the right treatment.
Initial Symptoms That Prompt Medical Attention
The first step to finding a brain tumor is noticing symptoms. These can be headaches, seizures, or changes in how you think or move. Spotting these early is very important for good treatment.
A medical expert says,
“The symptoms can tell us a lot about the tumor.”
Seeing these signs early means doctors can act fast.
Neurological Examination Process
A detailed check of the nervous system is a big part of finding a brain tumor. This check looks at how well you move, feel things, and think. It finds any signs of a tumor.
Doctors use special tests during this check. They might check your vision, hearing, balance, and how well you move. These tests give clues about where the tumor is and how it might affect you.
Imaging Studies: MRI and CT Scans for Brain Tumors
Imaging tests are key to confirming a brain tumor. MRI and CT scans are the main tools used.
MRI scans show the brain’s soft parts in detail. They help find the tumor’s size and where it is. CT scans give quick, clear images, which are great in emergencies.
These tests help doctors understand the tumor well. This guides the treatment plan.
Meeting With a Neurosurgeon
Meeting a neurosurgeon is a key step in dealing with a brain tumor. This meeting is vital for understanding your diagnosis and treatment options.
Why Patients Are Referred to Neurosurgeons After MRI
After an MRI shows a brain tumor, patients see a neurosurgeon. The MRI gives detailed images. These images help neurosurgeons see the tumor’s size, where it is, and how it might affect the brain.
The role of the neurosurgeon is to look at these images and decide the best treatment. They might talk about surgery or other options. They also answer any questions or worries the patient has.
What to Expect During Your First Consultation
In the first meeting, the neurosurgeon will go over your medical history and symptoms. They will explain your diagnosis. This is a chance for you to understand your condition and the treatment plan.
It’s a good idea to come prepared with questions and concerns. This way, you make sure all important topics are covered. You’ll have a clear idea of what’s happening with your health.
Questions to Ask Your Neurosurgeon
It’s important to have questions ready for your neurosurgeon. Some important ones are:
- What type of brain tumor do I have, and what are its characteristics?
- What are the available treatment options, and which one is recommended for my case?
- What are the possible risks and benefits of the suggested treatment?
- How will the treatment affect my daily life and long-term health?
By asking the right questions, you can make informed decisions about your care.
“The consultation with a neurosurgeon is a critical step in the treatment process. It’s a time for patients to gain a deeper understanding of their condition and the available treatment options.”
Treatment Options for Brain Tumors
Understanding the treatment options for brain tumors is key for patients. The choice depends on the tumor’s type, size, and location. It also depends on the patient’s overall health.
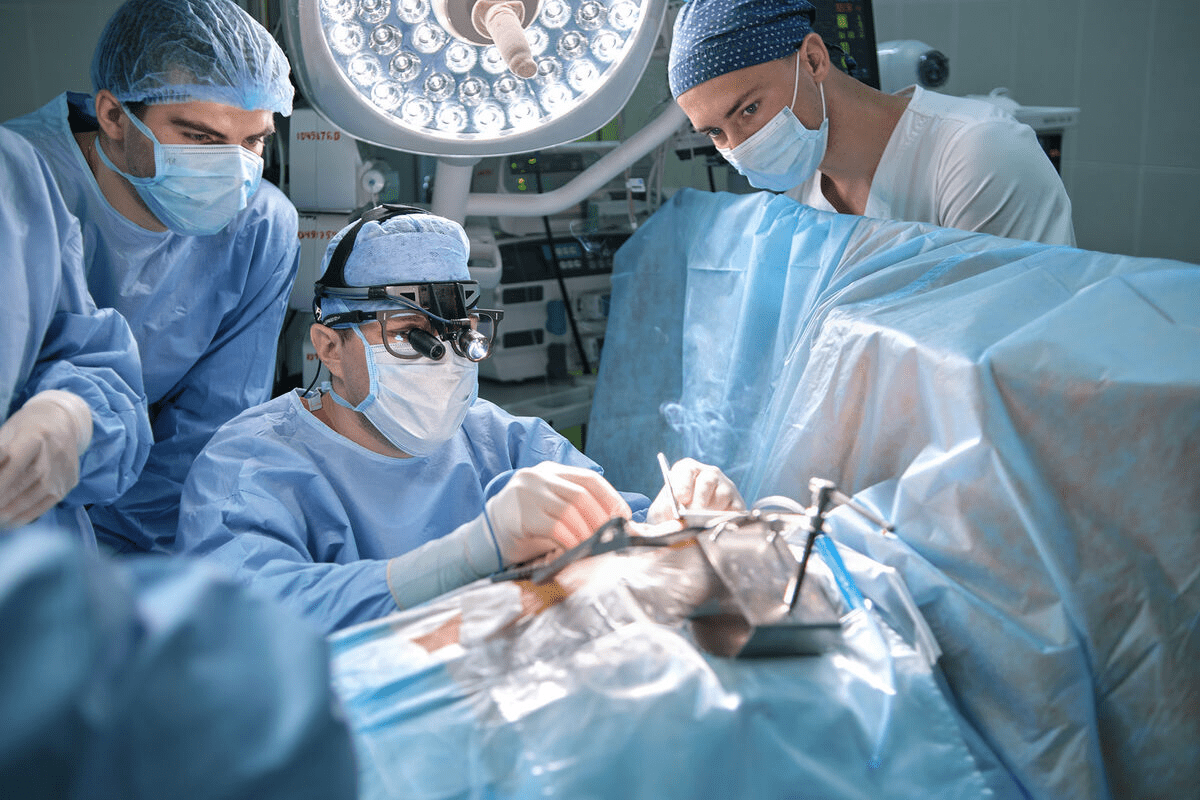
Surgical Approaches
Surgery is often the first step in treating brain tumors. It aims to remove as much of the tumor as possible. Craniotomy, a procedure where part of the skull is removed, is common. The decision to use surgery depends on the tumor’s location and how easy it is to reach.
Non-Surgical Alternatives
Not all brain tumors can be treated with surgery. In these cases, non-surgical alternatives like radiation therapy and chemotherapy are used. Radiation therapy kills tumor cells with high-energy beams. Chemotherapy uses drugs to target and destroy cancer cells.
Factors That Determine Treatment Selection
The choice of treatment is very personal. It considers the tumor’s characteristics, the patient’s health, and the treatment’s side effects. A team of healthcare professionals works together to find the best treatment plan.
The goal of treatment is to remove or control the tumor. It also aims to keep the patient’s quality of life good. Advances in medical technology and treatment strategies are helping improve outcomes for brain tumor patients.
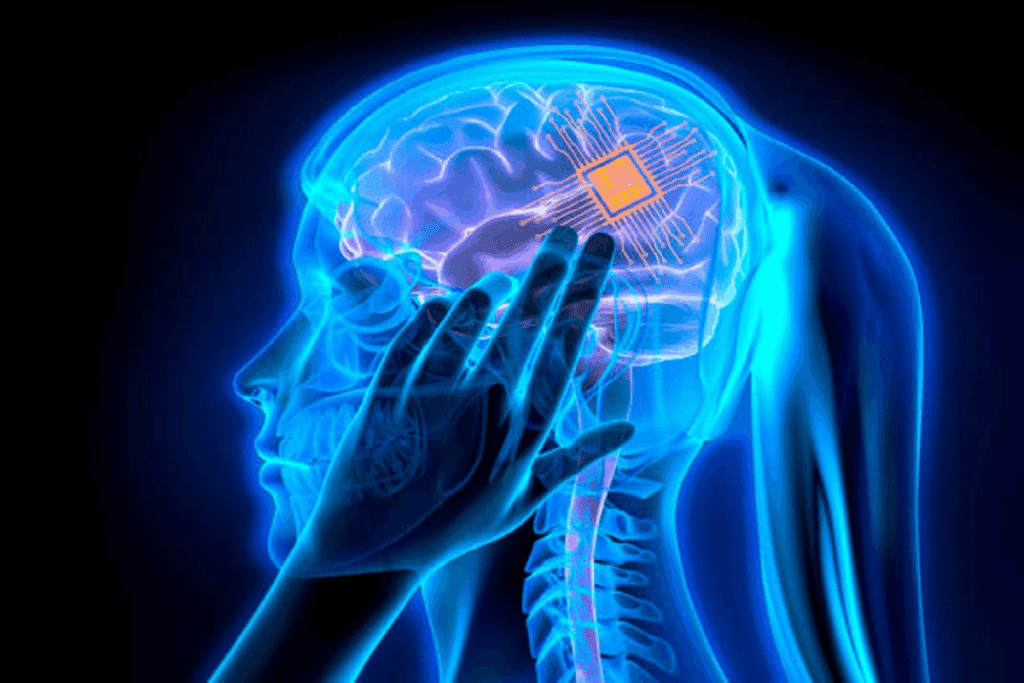
What is Craniotomy Surgery?
Craniotomy surgery is a complex procedure. It involves temporarily removing a part of the skull to access the brain. This is done to treat brain-related conditions like tumors, aneurysms, and traumatic brain injuries.
Definition and Purpose
A craniotomy is a surgery where a part of the skull is removed to expose the brain. The main goal is to let neurosurgeons operate on the brain when other methods won’t work.
The skull portion is removed to access the brain. This allows surgeons to remove tumors, repair blood vessels, or relieve pressure from swelling or bleeding.
When Craniotomy is Recommended
Craniotomy is suggested for several brain conditions. These include:
- Brain tumors that need to be removed or biopsied
- Aneurysms or arteriovenous malformations (AVMs) that require surgical clipping or removal
- Traumatic brain injuries with hematomas or skull fractures that need to be addressed
- Seizure disorders that are resistant to medication and require surgical intervention
The decision to do a craniotomy comes after a thorough evaluation and diagnosis. This often involves imaging studies like MRI or CT scans.
Types of Craniotomy Procedures
There are several types of craniotomy procedures. Each is tailored to the patient’s needs and the condition being treated.
Some common types include:
- Traditional Craniotomy: This involves removing a significant portion of the skull to access the brain.
- Keyhole Craniotomy: A minimally invasive approach where a small hole is made in the skull, often used for procedures like aneurysm clipping.
- Awake Craniotomy: Performed while the patient is awake, this type is used for surgeries near critical brain areas, allowing for real-time monitoring of the patient’s neurological functions.
Each type of craniotomy has its own indications and benefits. The choice of procedure depends on the patient’s condition, the location of the pathology, and the neurosurgeon’s expertise.
Types of Craniotomy Based on Location
The location of a brain tumor is key in choosing the right surgery. Different brain spots need special methods for safe and effective tumor removal.
Frontal Craniotomy
A frontal craniotomy accesses the frontal lobe. This area handles important tasks like decision-making and motor control. It’s used for tumors in this area.
Key Considerations: The surgical team must plan the incision and bone flap removal carefully. This is to avoid harming critical brain functions.
Temporal Craniotomy
Temporal craniotomy targets tumors in the temporal lobe. This area is vital for hearing, memory, and language. The surgery needs precise technique to protect nearby structures.
Benefits: This method can remove hard-to-reach tumors. It may improve outcomes for patients with these tumors.
Other Location-Specific Approaches
Other specialized craniotomy techniques are used based on the tumor’s location. These include:
- Occipital Craniotomy: For tumors in the occipital lobe, which handles visual information.
- Parietal Craniotomy: Used for tumors in the parietal lobe, affecting sensory processing and spatial awareness.
- Suboccipital Craniotomy: Often used for tumors at the brain’s base or in the posterior fossa.
Each approach needs careful planning and skill from a neurosurgical team. This ensures the best results for patients.
Preparing for Brain Tumor Surgery
Brain tumor surgery needs careful planning. This includes medical checks and getting ready emotionally. We’ll help you prepare well for surgery to get the best results.
Medical Evaluations and Tests
Before surgery, many tests are done. They check your health and the tumor’s details. These tests might include:
- Blood tests to find infections or health issues
- Imaging like MRI or CT scans to find the tumor’s exact spot
- Heart checks if you have heart problems
- Neurological tests to see how your brain is working
| Test/Evaluation | Purpose |
| Blood Tests | Check for infections or health conditions |
| Imaging Studies (MRI/CT) | Locate the tumor and plan surgery |
| Cardiac Evaluations | Assess heart health |
| Neurological Examinations | Evaluate neurological status |
Medication Adjustments
Talk to your doctor about your medicines before surgery. Some might need to be changed or stopped to avoid risks.
Medications to Discuss with Your Doctor:
- Blood thinners
- Diabetes medications
- Medications for high blood pressure
- Any supplements or herbal remedies
Mental and Emotional Preparation
Getting ready emotionally is as important as the medical side. Here’s how to prepare:
- Get support from loved ones or support groups
- Try stress-reducing activities like meditation or yoga
- Learn about the surgery and what to expect
By doing these things, you can handle surgery and recovery better. This can lead to a better outcome.
The Craniotomy Procedure Step by Step
Surgical teams take a careful approach during craniotomy procedures. They aim for patient safety and the best results. The steps of the craniotomy procedure are detailed below.
Anesthesia Administration
The first step is giving anesthesia. This makes sure patients are comfortable and pain-free. Our skilled anesthesiologists manage the anesthesia.
Surgical Access to the Brain
With anesthesia in place, we access the brain. We make a precise scalp incision and create a temporary skull opening. This is called a bone flap.
Tumor Removal Techniques
The main goal is to remove the brain tumor. We use advanced techniques and tools. This includes neuronavigation systems for precise tumor removal, with minimal damage to the brain.
- Advanced imaging guides the surgery.
- Microsurgical instruments help remove the tumor precisely.
- Intraoperative monitoring keeps neurological function safe.
Closing the Surgical Site
After removing the tumor, we close the site. We replace the bone flap and secure it with plates or sutures. Then, we close the scalp incision. We focus on a cosmetically pleasing closure.
Our detailed approach in the craniotomy procedure leads to the best outcomes for our patients.
Awake Craniotomy: A Special Approach
Awake craniotomy is a unique neurosurgery method. It’s used for certain cases where the patient is awake during parts of the surgery. This allows doctors to watch the brain’s function in real-time.
Necessity of Awake Craniotomy
Awake craniotomy is needed when a brain tumor is in a key area. This area controls important functions like speech and movement. The surgery is done with great care to avoid harming the brain.
Patient Experience During the Procedure
Patients start with sedation to relax during the awake craniotomy. As the surgery goes on, they wake up. Their brain activity is checked through tests like speech and movement checks.
Patients can talk to the team during the surgery. This feedback helps the doctors guide the operation.
The awake craniotomy procedure requires a high degree of coordination between the neurosurgeon, anesthesiologist, and the patient. It’s a complex process, but one that can offer significant benefits for appropriately selected patients.
Benefits and Challenges of Awake Craniotomy
The awake craniotomy has many benefits. It allows for precise tumor removal and reduces the risk of brain damage. It can also lead to faster recovery times.
But, there are challenges too. Patient anxiety is a big one. The surgery also needs a very skilled team.
| Benefits | Challenges |
| Precise tumor removal | Patient anxiety |
| Reduced neurological damage | Complex surgical process |
| Faster recovery times | Need for skilled surgical team |
Knowing about awake craniotomy’s benefits and challenges helps patients and families. It makes understanding brain tumor surgery easier.
Advanced Technologies in Brain Tumor Surgery
Brain tumor surgery has become more advanced with new technologies. These changes have made surgeries more precise and safe. Now, we use neuronavigation systems, intraoperative imaging, and laser ablation to improve our surgeries.
Neuronavigation Systems
Neuronavigation systems are key in modern brain tumor surgery. They use MRI and CT scans to map the brain. This helps surgeons find the tumor and plan the best surgery.
During surgery, these systems track instruments in real-time. This ensures we avoid important brain areas.
Key Benefits of Neuronavigation Systems:
- Enhanced precision in tumor localization
- Improved safety by avoiding critical brain areas
- Better planning and execution of the surgical approach
Intraoperative Imaging
Intraoperative imaging lets us see how the surgery is going. With MRI, we can see the tumor and brain tissue in real-time. This helps us adjust the surgery to remove the tumor safely.
| Intraoperative Imaging Technique | Benefits |
| Intraoperative MRI | Real-time visualization of tumor and brain tissue |
| Intraoperative CT | Quick assessment of surgical progress |
| Intraoperative Ultrasound | Portable and flexible imaging during surgery |
Laser Ablation Techniques
Laser ablation uses laser energy to kill tumor cells. It’s good for tumors that are hard to reach or in sensitive areas. Laser ablation can be guided by MRI for precise treatment.
The advantages of laser ablation include:
- Minimally invasive, reducing recovery time
- Precise targeting of tumor cells
- Potential for treating tumors in eloquent brain areas
By using these advanced technologies, we offer our patients the best treatments. As technology gets better, we expect even better results for our patients.
Immediate Post-Operative Care
Patients who have had craniotomy surgery need careful care right after surgery. This time is key to make sure they do well. It involves many steps to meet the patient’s needs.
Recovery in the Intensive Care Unit
Patients go to the Intensive Care Unit (ICU) after surgery. There, experts in neurocritical care watch them closely. They check the patient’s brain function, vital signs, and more.
The main goals are:
- Keeping vital signs stable
- Watching brain function
- Handling pain and discomfort
- Stopping complications
Monitoring for Complications
Spotting problems early is a big part of care. Issues can include:
- Infection
- Bleeding or hematoma
- Cerebral edema
- Seizures
Doctors do regular checks and scans, like CT scans, to find problems fast. Quick action helps lessen the effects of these issues.
Pain Management and Initial Mobility
Managing pain well is key for comfort and moving early. Our team uses different ways to control pain, like medicine and other methods.
Moving a bit early helps avoid problems like DVT and helps recovery. This might include:
- Slowly getting up
- Physical therapy
- Respiratory exercises
These steps are adjusted based on the patient’s situation and needs.
The Craniotomy Recovery Timeline
Knowing what to expect after a craniotomy surgery is key. It helps patients and their families get ready for the road ahead. Recovery includes a hospital stay, weeks at home, and ongoing therapy.
Hospital Stay Duration
The time spent in the hospital after surgery varies. It depends on the patient’s health and the surgery’s complexity. Usually, patients stay for 3 to 7 days.
During this time, doctors keep a close eye on the patient. They manage pain and watch for any complications.
First Weeks at Home
After leaving the hospital, patients recover at home for several weeks. It’s important to follow the doctor’s advice on medication, rest, and activity levels. Avoid heavy lifting and strenuous activities to prevent increased pressure in the brain.
Long-Term Recovery Milestones
Recovery from a craniotomy can take several months. Patients often see big improvements in 6 to 8 weeks. But, full recovery can take longer.
Regular check-ups with the neurosurgeon are vital. They help track progress and address any issues.
Physical and Occupational Therapy
Physical and occupational therapy are key to recovery. They help patients regain strength and learn daily tasks again. The therapy plan is based on the patient’s needs and surgery extent.
Following the recommended care and therapy helps patients heal better. It allows them to return to their lives as much as possible.
Physical Appearance After Surgery
Knowing what to expect about your looks after a craniotomy surgery is key. This surgery is needed to treat brain tumors but can change how you look. It’s important to be ready for these changes.
Craniotomy Scars and Healing Process
Scars from a craniotomy surgery are a big worry for many. How visible the scars are can depend on the surgery type and how well you heal. Doctors try to hide scars in your hairline or make them less noticeable.
Scars from a craniotomy go through stages. First, they might look red and swollen. But as time goes on, they will get flatter and less noticeable. Everyone heals at their own pace.
Hair Regrowth and Cosmetic Considerations
Many worry about hair loss after a craniotomy. The surgery might mean shaving part of your head. But, hair usually grows back, though it might take time.
Looking good after surgery is also important. Talk to your doctor about your concerns. There are ways to help with scars and hair growth.
Timeline for Visible Recovery
How long it takes to see changes after a craniotomy surgery varies. The first few weeks are the most noticeable. But, it can take months for scars to fade and hair to grow back fully.
| Recovery Stage | Timeline | Notable Changes |
| Initial Healing | 0-6 weeks | Swelling reduction, initial scar formation |
| Intermediate Recovery | 6 weeks-3 months | Scar maturation, hair regrowth begins |
| Long-term Recovery | 3-12 months | Scars become less noticeable, hair regrowth continues |
Knowing about these stages helps you prepare and focus on getting better.
Potential Complications and Side Effects
It’s important for patients and their families to know about the risks of craniotomy surgery. This surgery, like any major operation, has its own set of risks. These can affect how well a person recovers and their overall health.
Common Surgical Complications
Craniotomy surgery can lead to problems like infection, bleeding, and reactions to anesthesia. Infection is a big worry because it can cause serious issues if not treated right away. We take many steps to avoid these problems, like using antibiotics and keeping the surgery area clean.
| Complication | Description | Prevention/Management |
| Infection | Bacterial or viral infection at the surgical site | Prophylactic antibiotics, sterile technique |
| Bleeding | Hemorrhage during or after surgery | Careful hemostasis during surgery, monitoring post-op |
| Anesthesia Reaction | Adverse reaction to anesthesia | Pre-anesthetic evaluation, careful anesthesia management |
Neurological Side Effects
Neurological side effects can happen because of the surgery’s impact on brain tissue. These might include weakness, numbness, or trouble with speech and language. How severe these effects are can vary a lot, depending on the tumor’s location and size.
Possible neurological side effects include:
- Weakness or paralysis of limbs
- Numbness or sensory disturbances
- Speech and language difficulties
- Cognitive changes
Long-Term Effects on Cognitive Function
Craniotomy surgery can affect cognitive function in different ways, depending on the brain area involved. Some people might see changes in memory, attention, or how they make decisions. We work closely with patients and their families to watch for and help with any cognitive changes.
Brain Surgery Mortality Rates
Mortality rates for craniotomy surgery have gone down thanks to better surgical techniques and care before and after surgery. While death is a risk, it’s usually low for people having surgery for tumor removal on purpose.
Knowing about these possible complications and side effects is key to making good choices about craniotomy surgery. Our team is dedicated to giving full care and support during the surgery process.
Financial Aspects of Brain Tumor Surgery
It’s important for patients to know about the financial side of craniotomy surgery. The cost can be high, and understanding it helps with planning and managing expenses.
Average Costs of Craniotomy Surgery
The cost of craniotomy surgery changes based on several factors. These include the location, the hospital, the surgeon’s fees, and how complex the surgery is. On average, it can cost between $80,000 and over $200,000.
| Cost Component | Average Cost |
| Surgical Fees | $30,000 – $60,000 |
| Hospital Stay | $20,000 – $50,000 |
| Anesthesia | $1,000 – $3,000 |
| Imaging and Tests | $5,000 – $10,000 |
Insurance Coverage Considerations
Insurance is key in handling the financial side of craniotomy surgery. Most plans cover a big part of the costs. But, how much they cover can differ a lot.
It’s essential for patients to:
- Check their insurance before surgery
- Know what they’ll have to pay out of pocket
- Look into financial help if they need it
“Knowing your insurance benefits can really help with financial stress during tough times.” – Healthcare Financial Counselor
Financial Resources and Support
For those struggling with the cost of surgery, there are resources. Non-profits, government programs, and hospital help can offer support.
Patients can look into these options to manage their expenses. Also, many hospitals have social workers and financial counselors to help with the financial side of care.
Conclusion
Craniotomy surgery is a complex procedure that needs careful thought and detailed care. Understanding the whole process, from diagnosis to recovery, is key for patients and their families.
Brain tumor treatment goes beyond surgery. It includes supportive care during the recovery. We’ve looked at the different parts of craniotomy surgery, like preparation, the surgery itself, and aftercare.
Helping patients know what to expect can reduce anxiety and aid in recovery. Our aim is to offer top-notch healthcare and support to international patients getting craniotomy surgery for brain tumors.
A well-coordinated care team and a supportive setting are vital for treating brain tumors. We stress the need for a patient-focused approach to craniotomy surgery. This ensures individuals get the care and kindness they need during this tough time.
FAQ
What is a craniotomy?
A craniotomy is a surgery where a part of the skull is removed. This lets doctors access the brain. It’s often done to remove brain tumors.
How long does a craniotomy surgery take?
The time for a craniotomy surgery varies. It depends on the tumor’s location and the surgery’s complexity. It can last from 4 to 12 hours or more.
What is the life expectancy after brain tumor surgery?
Life expectancy after surgery depends on the tumor type and location. It also depends on the patient’s health. Generally, benign tumors have a better outlook than malignant ones.
Why would I be referred to a neurosurgeon after an MRI?
An MRI might show a condition needing surgery. If so, a neurosurgeon will be referred to you. This is often for brain tumors.
What are the possible complications of craniotomy surgery?
Complications can include infection, bleeding, and stroke. Seizures and neurological issues are also possible. The risk varies by case and the surgeon’s skill.
How long is the recovery time after a craniotomy?
Recovery time varies. Patients usually stay in the hospital for several days. Full recovery can take weeks to months, based on the surgery and health.
Can a neurologist perform surgery?
No, neurologists diagnose and treat but don’t perform surgery. Neurosurgeons are trained for brain and nervous system surgeries.
What is the cost of brain surgery?
Brain surgery costs vary. They depend on location, procedure complexity, and healthcare system. Always check with your provider and insurance.
How is a tumor behind the eye removed?
Removing tumors behind the eye varies by location and size. Neurosurgeons and ophthalmologists might work together.
What are the benefits of awake craniotomy?
Awake craniotomy lets the team watch the brain in real-time. This can help save important brain areas and improve outcomes.
What is the mortality rate associated with brain surgery?
Mortality rates vary by surgery type and patient health. Craniotomy risks are low with skilled surgeons.
How do I prepare for brain tumor surgery?
Preparing involves medical checks, medication adjustments, and mental preparation. Your team will guide you based on your needs.
What are the signs of complications after craniotomy?
Look out for severe headaches, confusion, weakness, and speech issues. Seizures are also a sign. Seek help immediately if you notice these.
How long does it take to recover from a craniotomy?
Recovery can take weeks to months. You’ll start with a hospital stay, then recover at home, gradually getting back to normal.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560922/