A blood glucose level of 800 mg/dL or higher is a severe medical emergency. It needs immediate attention. High blood sugar can cause serious problems if not treated quickly.
At Liv Hospital, we know how critical quick action is for extreme hyperglycemia. Our team focuses on both urgent care and long-term health. This is because hyperglycemia dehydration is a big concern.
Hyperglycemia affects 22-46 percent of hospitalized patients. It’s linked to more complications and death. So, knowing how to handle a blood glucose level of 1000 mg/dL or slightly lower is key to avoiding serious issues.
Key Takeaways
- Recognize the severity of a blood glucose level of 800 mg/dL or higher as a medical emergency.
- Understand that hyperglycemia can lead to serious complications if not managed promptly.
- Timely intervention is critical in managing extreme hyperglycemia.
- Hyperglycemia dehydration is a significant concern in cases of high blood glucose.
- Liv Hospital provides complete care for patients with severe hyperglycemia.
Understanding Blood Sugar Level of 800: A Medical Emergency
When blood sugar levels hit 800, it’s a serious situation that needs quick action. Levels this high are linked to severe hyperglycemia. This can cause serious problems like diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS).
The American Diabetes Association says it’s key to test for type 2 diabetes in adults over 35 and those at risk. Knowing the dangers of very high blood sugar is vital for quick and right care.
What Constitutes a Dangerous Blood Sugar Level
A blood sugar level is dangerous when it’s way above normal, usually over 300 mg/dL. Levels around 800 mg/dL or higher are very risky. At these levels, the body’s cells don’t get enough glucose, and the blood has too much sugar.
Medical guidelines say a blood sugar level of 800 mg/dL is a big emergency. The danger isn’t just the level but how long it stays high.
The Life-Threatening Nature of Blood Sugar 800
Blood sugar levels of 800 or more can cause severe dehydration. This is because of the high sugar levels. It leads to a cycle where dehydration makes hyperglycemia worse, making things even more complicated.
“Severe hyperglycemia is a medical emergency that can lead to serious complications, including coma and even death if not treated promptly.”
The high risk of such blood sugar levels shows the need for fast medical help. Quick treatment can reduce the dangers of severe hyperglycemia and prevent lasting harm.
Recognizing the Symptoms of Extremely High Blood Sugar
It’s important to know the signs of blood glucose 800 to act fast and avoid health problems. When blood sugar levels spike, the body shows clear warning signs that need attention.
Early Warning Signs
Early signs of very high blood sugar include needing to pee a lot, feeling very thirsty, and having a dry mouth. You might also see your vision blur, feel extremely tired, or get headaches. These happen because your body tries to get rid of extra glucose by peeing a lot, which can lead to dehydration and other issues.
- Frequent Urination: Your body tries to get rid of extra glucose by peeing more often.
- Extreme Thirst: Peeing a lot makes you dehydrated, which makes you feel very thirsty.
- Dry Mouth: Not making enough saliva makes your mouth dry.
- Blurred Vision: High blood sugar can make your eye lens swell, causing blurry vision.
Critical Symptoms Requiring Immediate Action
As blood sugar levels keep going up, more serious symptoms can appear. These include feeling confused, having a fast or irregular heartbeat, and even losing consciousness. These serious symptoms need quick medical help to avoid serious harm.
- Confusion or Altered Mental State: High blood sugar can mess with your brain, causing confusion or changes in how you think.
- Rapid Heartbeat: Dehydration and imbalances in electrolytes can make your heart beat too fast or irregularly.
- Loss of Consciousness: In very bad cases, extremely high blood sugar can cause you to lose consciousness or even go into a coma.
Doctors say it’s very important to spot these symptoms early. This way, you can get help quickly and avoid serious problems (Source: American Diabetes Association).
Differences in Symptoms Between Type 1 and Type 2 Diabetes
Type 1 and Type 2 diabetes both can cause high blood sugar, but the symptoms are different. Type 1 diabetes often starts quickly and symptoms are more obvious. Type 2 diabetes symptoms may be milder and take longer to show up.
Knowing these differences helps in managing and treating diabetes better. For example, people with Type 1 diabetes might see symptoms like severe high blood sugar quickly. Those with Type 2 diabetes might not notice their symptoms as much because they come on more slowly.
Immediate Actions When Blood Sugar 800 Is Detected
A blood sugar reading of 800 is a medical emergency that demands swift response. When faced with such a high blood sugar level, it’s critical to understand the necessary steps to take to prevent further complications.
Call Emergency Services Immediately
The first and most critical step when detecting a blood sugar level of 800 is to call emergency services right away. This condition is life-threatening and requires immediate medical attention. We cannot stress enough the importance of acting quickly.
Do not attempt to drive to the hospital yourself. Instead, call for an ambulance or emergency medical services. Medical professionals can provide the necessary care during transport, which is vital for managing severe hyperglycemia.
Position and Monitor the Person
If the person is unconscious or showing signs of severe distress, it’s essential to position them on their side to prevent choking in case of vomiting. We must monitor their vital signs, such as pulse and breathing rate, until medical help arrives.
Stay with the person and provide any information about their condition, including their medical history and any medications they are taking, to the emergency responders when they arrive.
What Not to Do During This Emergency
While waiting for medical help, there are several things that should be avoided. Do not give the person any medication without consulting medical professionals first. This includes insulin, as administering it without proper guidance can lead to further complications.
Avoid giving the person anything to drink if they are unconscious or unable to swallow. Dehydration is a significant concern, but improper fluid administration can cause more harm.
Action | Reason |
Call Emergency Services | Immediate medical attention is critical for blood sugar level 800. |
Position on Side | Prevents choking in case of vomiting. |
Monitor Vital Signs | Helps in assessing the severity of the condition. |
Avoid Self-Medication | Prevents incorrect dosing and possible complications. |
In conclusion, when a blood sugar level of 800 is detected, every minute counts. By calling emergency services immediately, positioning and monitoring the person, and avoiding certain actions, we can help mitigate the risks associated with such a severe hyperglycemic episode.
Medical Interventions for Severe Hyperglycemia
Severe hyperglycemia needs quick and effective treatment to avoid serious problems. When blood sugar levels get too high, the body can’t manage fluids and electrolytes well. This can lead to life-threatening conditions.
Emergency Room Procedures
When someone with severe hyperglycemia gets to the emergency room, they get help right away. The first steps are:
- Quick check of the patient’s condition, including blood sugar and vital signs.
- Starting IV fluids and medicines.
- Getting blood samples for tests on electrolytes, kidney function, and ketones.
“Quick and right treatment for severe hyperglycemia in the emergency room is key to avoid serious problems,” says Medical Expert, an endocrinologist. “It’s not just about lowering blood sugar. It’s about fixing the body’s metabolic problems too.”
Intravenous Fluid Administration
IV fluids are key in treating severe hyperglycemia, mainly when it causes dehydration. The goals of IV fluids are:
- To rehydrate the patient and fix the blood volume.
- To lower blood sugar by improving kidney function and glucose removal.
- To fix electrolyte imbalances that come with severe hyperglycemia.
The type and amount of IV fluid given depend on the patient’s needs. This includes their hydration, electrolyte levels, and heart health.
Insulin Therapy Protocols
Insulin therapy is vital for managing severe hyperglycemia. In emergencies, intravenous insulin infusion is often used. It lets doctors control insulin delivery closely and adjust quickly as blood sugar changes.
The insulin dose is changed based on blood sugar tests every hour. The goal is to lower blood sugar slowly and safely. When the patient is stable, they might switch to insulin shots.
In summary, treating severe hyperglycemia involves many steps in the emergency room. These include IV fluids and insulin therapy. By knowing and using these treatments, doctors can lower the risks of very high blood sugar levels.
Understanding Diabetic Ketoacidosis (DKA) at Blood Sugar 800
When blood sugar hits 800, knowing about diabetic ketoacidosis (DKA) is key. DKA is a serious diabetes problem. It happens when the body makes too many ketones, which are harmful acids.
The Mechanism of DKA Development
DKA starts when the body can’t use glucose for energy because it lacks insulin. So, it starts breaking down fat, making ketones. This change can make the blood too acidic.
“The body is stressed and can’t use glucose well,” says a top diabetes expert. This stress is often caused by infections, not enough insulin, or other stressors.
Knowing these causes is important to stop DKA before it starts.
Complications of Untreated DKA
If DKA isn’t treated, it can cause serious problems. These include:
- Cerebral edema (swelling of the brain)
- Acute kidney injury
- Cardiac arrhythmias
- Respiratory failure
Quick medical help is vital to avoid these issues and lower death risk.
Treatment Approaches for DKA
DKA treatment has several main parts:
- Fluid replacement to fix dehydration
- Insulin therapy to lower blood sugar and stop ketones
- Electrolyte replacement to balance out
Watching the patient closely is key during treatment. “The main steps in treating DKA are giving lots of fluids and insulin,” says a doctor.
Understanding DKA’s causes, effects, and treatments helps doctors give better care. This is very important when blood sugar levels are extremely high, like 800.
Hyperosmolar Hyperglycemic State (HHS) at Glucose Levels of 1000
When blood glucose levels hit 1000 mg/dL or more, a serious condition called Hyperosmolar Hyperglycemic State (HHS) can happen. HHS is a dangerous complication for people with diabetes, mainly those with type 2. It’s marked by very high blood sugar, often over 600 mg/dL, and severe dehydration.
How HHS Differs from DKA
HHS is different from Diabetic Ketoacidosis (DKA), another diabetes complication. Both have high blood sugar, but HHS doesn’t have ketoacidosis. Instead, it’s known for extreme hyperglycemia and dehydration.
Even without ketoacidosis, HHS is very dangerous. It’s often seen in older adults or those with other health issues.
The Vicious Cycle of Dehydration and Rising Blood Sugar
In HHS, high blood sugar causes dehydration, which then raises blood sugar even more. High glucose in the blood makes urine, leading to water and electrolyte loss.
This dehydration makes blood thicker and more viscous. It can cause serious problems like blood clots and organ failure if not treated quickly.
Special Considerations in HHS Treatment
Treating HHS needs careful attention to fluid status, electrolyte balance, and blood glucose. Aggressive fluid replacement is key to fix dehydration and lower blood sugar. But, it must be done carefully to avoid brain swelling or heart failure.
Insulin therapy may be used to lower blood sugar, but it starts after fluid replacement. This is because insulin can dehydrate the patient too much if given too soon.
It’s important to watch the patient closely during treatment. Check blood glucose, electrolytes, and fluid status regularly. This helps adjust the treatment plan for the best results.
Addressing Severe Dehydration in Hyperglycemic Emergencies
High blood sugar can lead to severe dehydration, which is very dangerous. This is true for conditions like diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS). Dehydration makes high blood sugar worse and harder to treat.
The Critical Role of Fluid Replacement
Fluid replacement is key in treating high blood sugar emergencies. Intravenous fluids are best because they quickly replace lost fluids and electrolytes. We start with isotonic saline solution to help the heart and kidneys.
“Fluid replacement is vital to avoid more problems and help the body heal,” say doctors. The amount and type of fluid depend on the patient’s condition and how much fluid they lose.
Electrolyte Imbalances and Their Correction
High blood sugar can cause big changes in electrolytes like potassium and sodium. It’s important to watch these levels to fix them right. Even if potassium levels seem okay, we often need to add more because the body is short.
- We must watch potassium levels to avoid too little or too much.
- Managing sodium levels is also key, even with very high blood sugar.
Monitoring Fluid Status During Treatment
Keeping an eye on how much fluid the patient has is very important. We check vital signs, urine output, and how hydrated they seem. Fluid balance charts are vital to track fluids and make sure we’re not giving too much or too little.
By treating dehydration and fixing electrolyte imbalances, we can greatly improve patient outcomes. Effective treatment needs a detailed plan, close monitoring, and adjustments as needed.
Hospital Care and Recovery After Initial Stabilization
After the patient’s condition is stable, the focus turns to hospital care and recovery plans. Managing a blood sugar level of 800 needs a detailed approach. This is to prevent future problems and help the patient recover safely.
Continuous Glucose Monitoring
Continuous glucose monitoring (CGM) is key in managing blood sugar during recovery. CGM systems give real-time glucose level data. This helps doctors adjust insulin doses and treatments better.
This technology spots trends in blood glucose levels. It makes managing blood sugar more effective.
Transition from IV to Subcutaneous Insulin
Switching from IV insulin to subcutaneous insulin is a big step in recovery. This change must be done carefully to keep blood sugar stable. Healthcare providers start subcutaneous insulin while the patient is on IV insulin. They slowly reduce the IV insulin as the subcutaneous insulin starts working.
Length of Hospital Stay and Discharge Criteria
The time a patient stays in the hospital can vary. It depends on how severe the hyperglycemia is, if there are complications, and how well the patient responds to treatment. To be discharged, patients need stable blood sugar, enough hydration, and to be able to manage their diabetes at home.
Patient education on diabetes management is very important before leaving the hospital. This includes learning about insulin use and blood glucose monitoring.
Recovering from a severe hyperglycemic episode is tough. Our healthcare team works hard with patients. They help ensure a smooth move from hospital care to managing diabetes at home. They provide the support and guidance needed to avoid future problems.
Preventing Future Episodes of Severe Hyperglycemia
To avoid severe hyperglycemia, a few steps are key. These include sticking to your medication, checking your blood sugar often, and knowing how to handle sick days. By doing these things, people with diabetes can lower their risk of very high blood sugar, like 800 or more.
Medication Adherence and Adjustment
It’s very important to take your diabetes medicine as your doctor says. Being consistent with your medication helps keep your blood sugar in check. But, your needs might change. This could be because of diet, exercise, or other health issues. So, it’s important to talk to your doctor often to adjust your medicine.
“Taking your medicine as directed is a big part of managing diabetes,” a study on diabetes care points out.
“People who stick to their medication have better blood sugar control and lower risk of problems.”
This shows how important it is to take your medicine and talk to your doctor about any issues.
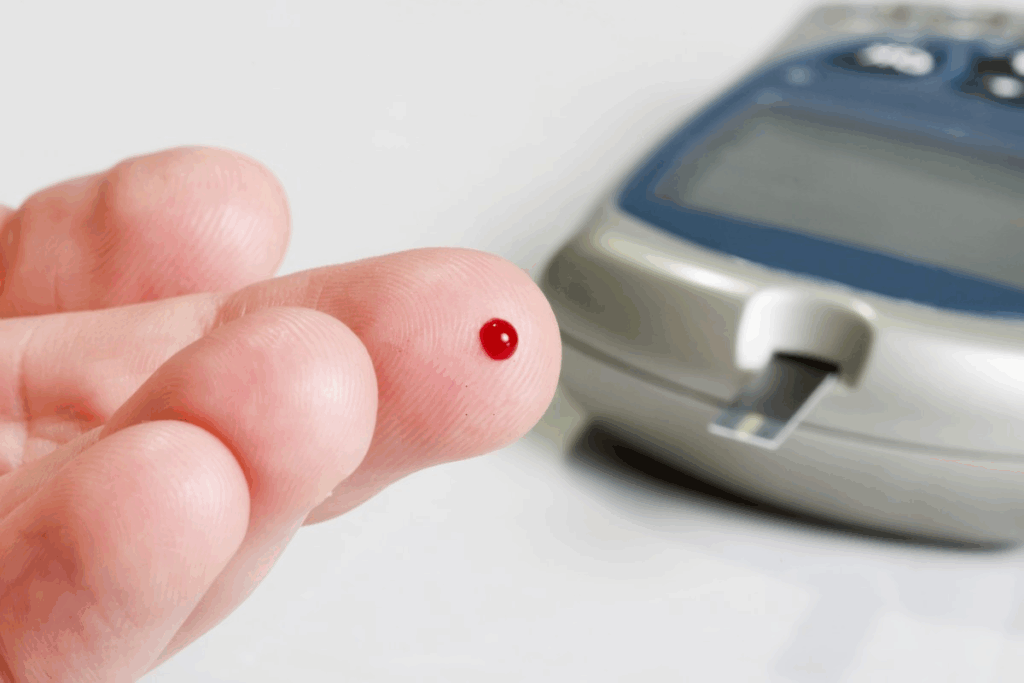
Blood Sugar Monitoring Schedules
Checking your blood sugar regularly is key to knowing how it’s affected by different things. Having a regular monitoring schedule helps spot problems early. This way, you can make smart choices about what you eat, how much you exercise, and your medicine, to avoid very high blood sugar.
- Check your blood sugar at the same times every day.
- Keep a record of your readings to see patterns.
- Check more often when you’re sick or stressed.
Sick Day Management for Diabetic Patients
When you’re sick, it’s harder to keep your blood sugar in check. Having a sick day plan is very important. This plan should tell you how to adjust your medicine, how much to drink, and when to get medical help. Drinking plenty of water and keeping an eye on your blood sugar are key when you’re not feeling well.
When you’re sick, it’s important to stay in touch with your doctor for advice. They can help you adjust your treatment to avoid very high blood sugar.
By focusing on taking your medicine, checking your blood sugar, and knowing how to handle sick days, people with diabetes can lower their risk of very high blood sugar. This proactive approach not only improves health but also makes life better overall.
Conclusion: Living Safely After a Blood Sugar Emergency
After a blood sugar emergency, like hitting 800, it’s key to change your lifestyle. We talked about how to handle high blood sugar and dehydration. We also looked at the dangers of levels reaching 1000.
Staying safe means watching your blood sugar closely, taking your meds, and knowing the signs of severe high blood sugar. Understanding the dangers of very high blood sugar helps prevent future crises.
It’s vital to keep up with your care and stay alert. Regular doctor visits, eating right, and drinking plenty of water are essential. These steps help manage diabetes and keep you healthy and active.
FAQ
What is considered a dangerously high blood sugar level?
A blood sugar level of 800 or higher is very dangerous and needs immediate help. It can cause serious problems like diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS).
What are the symptoms of extremely high blood sugar?
Symptoms include feeling very thirsty and needing to pee a lot. You might also feel tired, see things blurry, and in bad cases, get confused or even lose consciousness. The symptoms can be different for Type 1 and Type 2 diabetes.
How is severe hyperglycemia treated in the emergency room?
In the emergency room, treatment starts with giving fluids to fix dehydration. Then, insulin is used to lower blood sugar. The team also watches your vital signs and blood sugar closely. Their goal is to make you stable and avoid more problems.
What is diabetic ketoacidosis (DKA), and how is it treated?
DKA is a serious problem that happens when your body makes too many ketones. Treatment includes fluids, insulin, and fixing any imbalances in your body. Quick action is key to avoid serious issues.
What is hyperosmolar hyperglycemic state (HHS), and how does it differ from DKA?
HHS is when your blood sugar is very high and you’re dehydrated, but you might not have ketones. It’s more common in Type 2 diabetes and is more deadly than DKA.
How can future episodes of severe hyperglycemia be prevented?
To prevent severe hyperglycemia, stick to your medication, check your blood sugar often, and manage your diabetes when you’re sick. Being proactive and having a routine can really help.
What is the role of fluid replacement in treating hyperglycemic emergencies?
Fluids are very important in treating dehydration from high blood sugar. They help rehydrate your body, improve blood flow, and keep your body working right.
How is blood sugar monitored in the hospital?
In the hospital, they use continuous glucose monitoring systems to track your blood sugar. This lets them make quick changes to your treatment as needed.
What are the key factors influencing hospital stay and discharge after a hyperglycemic emergency?
The length of your hospital stay depends on how bad the hyperglycemic episode was, if you had any complications, and how well you respond to treatment. You’ll be ready to go home when your blood sugar is stable, you’re well-hydrated, and you can manage your diabetes on your own.
How can patients manage their diabetes on sick days to prevent severe hyperglycemia?
On sick days, keep taking your diabetes medication and check your blood sugar often. Make sure to drink plenty of water. You might need to adjust your medication and how much water you drink based on how sick you are and your blood sugar levels.
References:
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699728/