Many parents see their newborns crying a lot and notice sticky discharge in their eyes. They often wonder if surgery is needed. Tear duct obstruction is common, affecting about 20 percent of infants today.Learn about eye duct surgery infants procedures for treating tear duct obstruction in babies. Understand the necessity of eye duct surgery infants.
Most cases get better on their own in the first year. But, knowing when to seek help is key for parents. At Liv Hospital, our team of pediatric ophthalmologists offers caring, evidence-based care. We help diagnose and treat tear duct obstruction, also known as nasolacrimal duct obstruction (NLDO).
Key Takeaways
- Tear duct obstruction is a common condition in newborns, affecting up to 20 percent of infants.
- Symptoms include excessive tearing, ocular discharge, and crusty buildup on eyelashes.
- Most cases resolve naturally within the first year.
- Conservative management and probing surgery are treatment options available.
- Professional intervention is necessary if symptoms persist.
Understanding Tear Duct Obstruction in Infants

It’s important for parents to know about nasolacrimal duct obstruction in infants. This condition, also known as NLDO, happens when the tear duct is blocked. This blockage stops tears from draining properly.
What is Nasolacrimal Duct Obstruction (NLDO)?
Nasolacrimal duct obstruction occurs when the tear duct can’t drain tears into the nasal cavity. This is usually because the duct didn’t fully develop, like at the valve of Hasner. This means tears build up, causing symptoms.
Prevalence and Common Age of Onset
About 1 in 5 newborns have tear duct obstruction. It’s often there from birth because the tear duct system isn’t fully formed. Symptoms show up in the first few months.
Many cases clear up as the baby grows. But some need medical help. Knowing about NLDO helps parents and doctors catch it early. This can prevent serious problems like dacryocystitis, an infection of the tear sac.
Anatomy of the Tear Duct System
The tear duct system is key to eye health. It drains tears from the eye into the nasal cavity. Tears, made by the lacrimal glands, clean the eye by removing dust and dirt.
Normal Tear Drainage Pathway
Tears leave the eye through small channels called canaliculi in the eyelid’s inner corner. These channels merge into the common canaliculus. Then, they flow into the lacrimal sac.
From there, tears move down the nasolacrimal duct and into the nasal cavity. “The normal tear drainage pathway is a complex process,” say ophthalmologists. It’s vital for eye health and preventing blockages.
The Valve of Hasner and Common Blockage Points
The valve of Hasner is at the end of the nasolacrimal duct. It stops nasal secretions from flowing back into the tear duct system. But, it’s a common blockage point, mainly in infants.
Blockages can happen at the valve of Hasner, the nasolacrimal duct, or where the canaliculi meet the lacrimal sac. Knowing these areas helps in diagnosing and treating tear duct blockages.
Signs and Symptoms of Blocked Tear Ducts
It’s important to know the signs of blocked tear ducts in babies. This issue, known as nasolacrimal duct obstruction, can be very upsetting for both babies and their parents.
Excessive Tearing (Epiphora)
Excessive tearing, or epiphora, is a key sign of a blocked tear duct. When the tear duct is blocked, tears can’t drain properly. This leads to tears spilling over onto the cheek, making it look like the eye is always watering.
Eye Discharge and Crusting
Eye discharge is another symptom, often causing crusting on the eyelashes, mainly after sleep. This discharge can be white or yellowish, known as “sticky eyes.” It happens because debris and bacteria build up in the eye, thanks to the blocked tear duct.
Symptom | Description |
Excessive Tearing | Overflow of tears onto the cheek due to obstructed tear duct |
Eye Discharge | White or yellowish discharge, potentially leading to crusting on eyelashes |
Redness and Irritation | Inflammation of the eye and surrounding area, potentially causing discomfort |
Redness and Irritation
Babies with blocked tear ducts may show redness and irritation in the affected eye. This is often because of the buildup of discharge and the inflammation it causes. The skin around the eye might also get irritated, making the baby even more uncomfortable.
Spotting these signs early can lead to getting the right medical help. This can prevent serious issues like dacryocystitis, an infection of the tear sac.
Causes of Tear Duct Obstruction
We look into why tear ducts get blocked in babies. This blockage, or nasolacrimal duct obstruction (NLDO), happens when the tear drainage system gets clogged. Knowing why it happens helps doctors find the best way to treat it.
Incomplete Canalization
The main reason for tear duct blockage in babies is incomplete canalization of the nasolacrimal duct. When a baby is growing in the womb, the tear duct system starts to form. But sometimes, this process doesn’t finish right, leaving a blockage. This blockage is there from birth and often shows up in the first few months.
Other Possible Causes
While incomplete canalization is the main reason, other things can also block tear ducts, but less often. Issues with the eye or eyelids, like a crooked eyelid, can cause problems. Also, an infection or swelling in the tear duct area might block it too.
It’s important to know that sometimes, tear duct blockage is linked to other birth defects or syndromes. But this is not common, and most cases of NLDO happen in healthy babies.
Figuring out why a tear duct is blocked is key to treating it right. Doctors can then suggest the best treatment based on the cause.
Conservative Treatment Approaches
For infants, the first step in treating tear duct obstruction is often conservative management. These methods are usually effective for babies under 1 year old. They can solve the problem without surgery.
Proper Tear Duct Massage Techniques
Tear duct massage is a key conservative treatment. To do it, press gently on the outside of your baby’s nose with your finger. Then, stroke downwards towards the nose tip. This helps drain tears and should be done 2 to 3 times a day.
Here’s a simple guide to the massage:
- Make sure your hands are clean before starting.
- Find the tear duct area on the inside corner of your baby’s eye, near the nose.
- Press your finger on this area and stroke downwards.
- Do this motion several times during each session.
Cleaning Practices for Affected Eyes
Keeping the affected eye clean is key in managing tear duct obstruction. Regular cleaning helps prevent infections and aids in healing.
To clean the eye:
- Use a clean, damp cloth to wipe away discharge or crusting.
- Wipe from the inner corner of the eye outward to avoid pushing debris back into the tear duct.
- Use a fresh section of the cloth for each wipe to prevent spreading infection.
Antibiotic Drops for Secondary Infections
If a secondary infection happens, antibiotic drops might be needed. These drops help clear the infection and prevent further problems.
It’s important to follow the dosage and use instructions given by your healthcare provider. This ensures the treatment works well.
By using these conservative treatments, many infants can overcome tear duct obstruction without surgery.
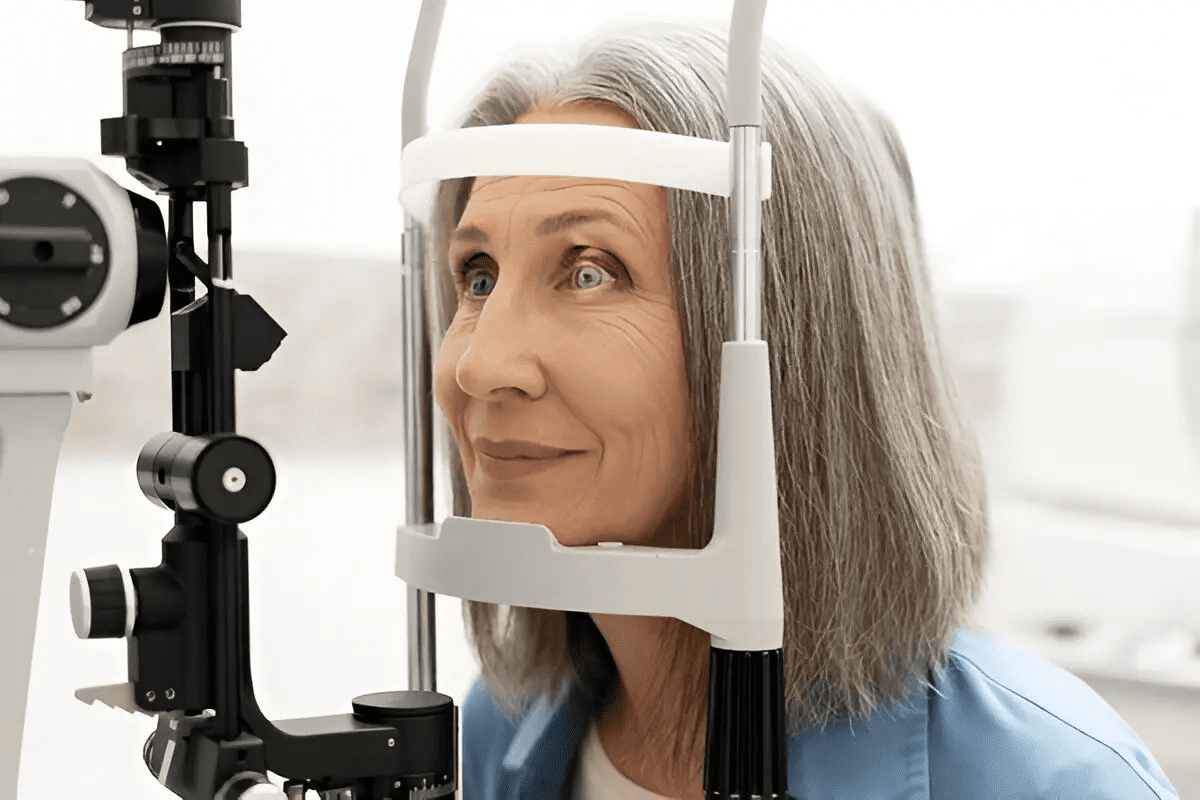
When to Consider Eye Duct Surgery for Infants
Infants with tear duct blockages might need surgery if other treatments don’t work. It’s important to know when surgery is needed.
Age Considerations for Surgical Intervention
The age of the baby is key in deciding if surgery is needed. Usually, if the blockage lasts over 12 months, surgery is considered. Always talk to a pediatric ophthalmologist for advice.
Age | Likelihood of Spontaneous Resolution | Surgical Consideration |
0-6 months | High | Low |
6-12 months | Moderate | Moderate |
Beyond 12 months | Low | High |
Signs That Conservative Methods Are Failing
If treatments like massage and drops don’t help, surgery might be needed. Signs like too much tearing, discharge, and redness mean it’s not getting better.
Key indicators that conservative methods are failing include:
- Persistent or worsening symptoms
- Recurring eye infections
- Failure of symptoms to improve with conservative management
Finding a Pediatric Ophthalmologist
Seeing a pediatric ophthalmologist is a big step in deciding on surgery. They can check the baby’s eyes and suggest the best treatment. Ask your doctor for a referral to see one.
Knowing when to choose surgery helps parents make the best choices for their baby. We’re here to support and guide you every step of the way.
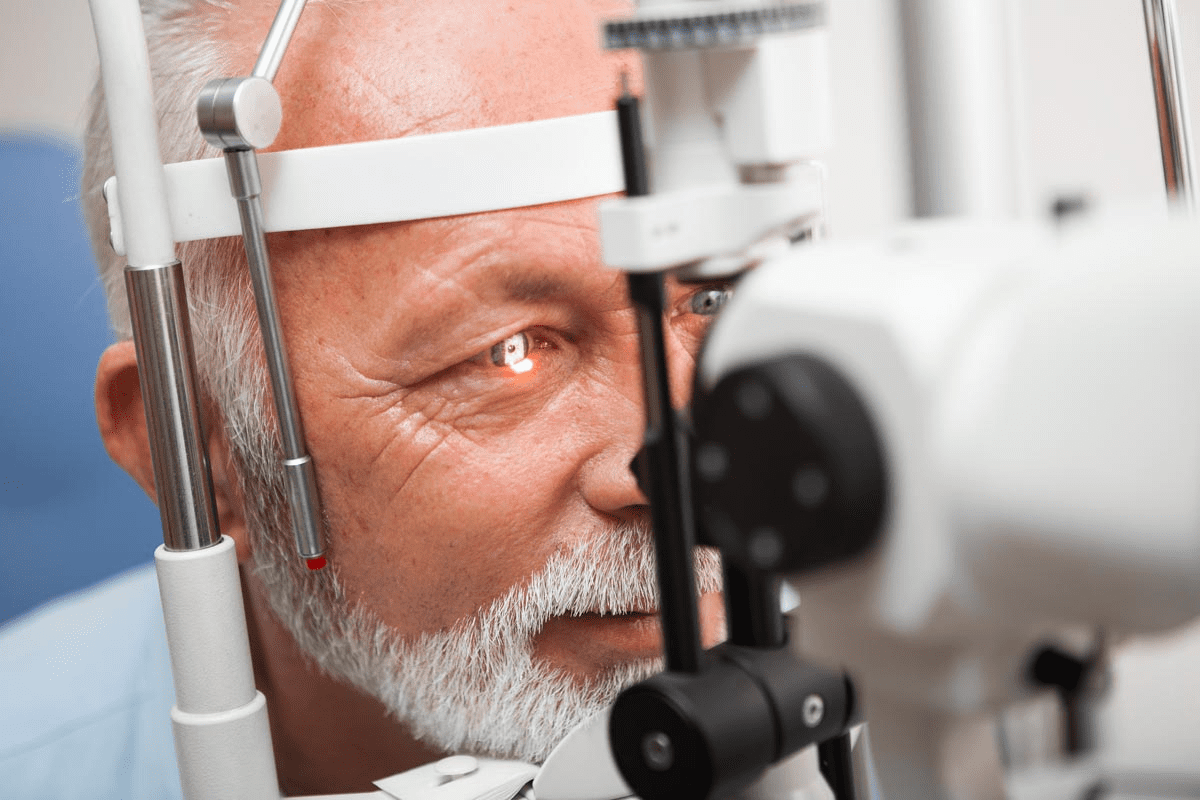
Tear Duct Probing Procedure Explained
The tear duct probing procedure is a simple surgery to remove blockages in the tear duct. It’s often chosen when other treatments don’t work for babies.
How Probing Surgery Works
Infants are usually under general anesthesia for this surgery. The surgeon uses a thin, smooth metal probe through the punctum (the small opening in the eyelid) to clear the blockage. This opens up the tissue that might be blocking the tear duct, allowing tears to drain properly again.
As one medical expert notes,
“Tear duct probing is a highly effective procedure for treating congenital nasolacrimal duct obstruction, with success rates varying by age.”
Knowing how the procedure works can ease parents’ worries if they’re thinking about it for their baby.
Success Rates by Age
The success of tear duct probing depends a lot on the baby’s age. Younger infants tend to have higher success rates. Babies under 12 months have a success rate over 90%. Those between 12 and 18 months have a slightly lower rate. And for babies over 18 months, the success rate goes down even more, making early treatment key.
- Under 12 months: >90% success rate
- 12-18 months: slightly lower success rate
- Over 18 months: decreased success rate
Potential Risks and Complications
While tear duct probing is generally safe, there are risks and complications to know about. These can include infection, bleeding, or damage to nearby structures. But serious problems are rare if a skilled pediatric ophthalmologist does the procedure.
Parents should talk to their child’s surgeon about these risks. This helps them understand the benefits and risks of tear duct probing. They can then make a well-informed choice for their baby’s treatment.
Advanced Surgical Options for Persistent Obstruction
When simple treatments don’t work, more serious surgery is needed for tear duct blockage in babies. These surgeries aim to clear the blockage and help tears drain properly.
Balloon Catheter Dilation
Balloon catheter dilation is a gentle surgery for tear duct blockage. A small balloon is inserted into the tear duct and inflated to open it up. It’s done under general anesthesia to keep the baby safe and comfortable.
A study in the Journal of AAPOS found this method works well for many cases. How well it works depends on the baby’s age and how bad the blockage is.
Silicone Tube Intubation
Silicone tube intubation puts a silicone tube in the tear duct to keep it open. This is done when other treatments don’t work or the blockage is very stubborn. The tube stays in for months before it’s removed.
Research shows this method is very effective. Here’s a table with results from different studies.
Study | Success Rate | Complications |
Study A | 85% | 5% |
Study B | 90% | 3% |
Study C | 88% | 4% |
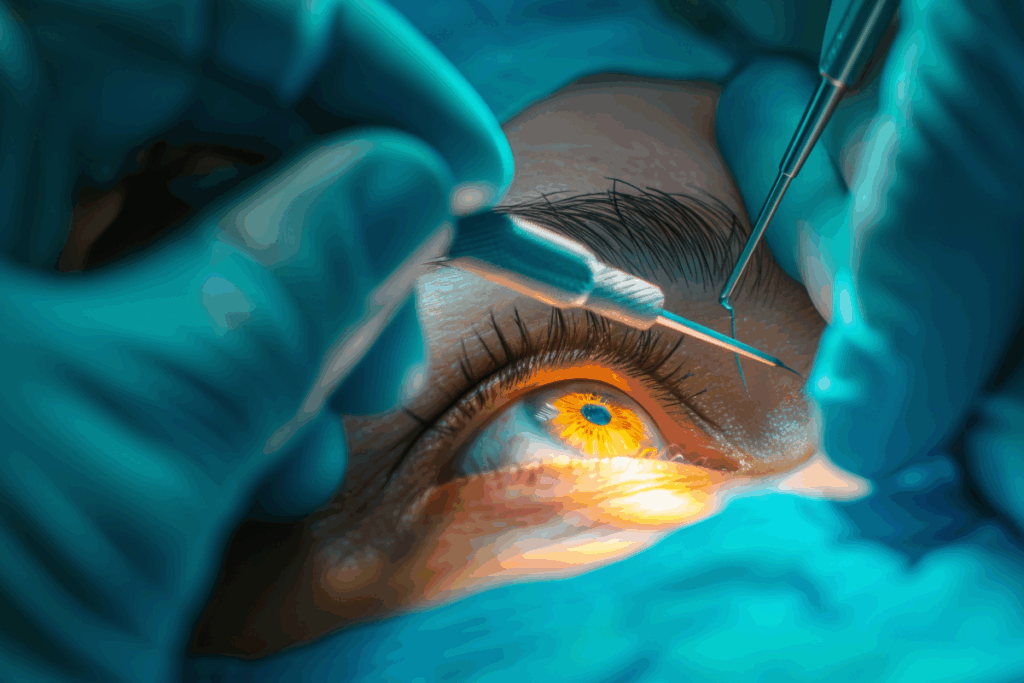
Dacryocystorhinostomy (DCR) for Severe Cases
For very bad cases, Dacryocystorhinostomy (DCR) is used. DCR makes a new path for tears to drain from the lacrimal sac to the nose. It’s done under general anesthesia.
“DCR is considered a highly effective treatment for complex tear duct obstructions, improving symptoms for selected patients.”
— Ophthalmology Journal
As shown in the image below, DCR creates a new drainage pathway, bypassing the obstructed area.
Thinking about surgery can worry parents. But these surgeries are safe and work well. Choosing the right one can greatly help babies with tear duct problems.
Post-Surgical Care and Recovery
After your baby has tear duct surgery, it’s important to take good care of them. Following the right steps can help them heal faster and avoid problems.
Immediate Aftercare Instructions
Right after surgery, keep the eye clean to avoid infection. Use antibiotic eye drops or ointment a few times a day for a week. Clean the eye gently with a warm, damp cloth to remove any discharge or crusting.
Key aftercare practices include:
- Administering antibiotic eye drops as prescribed by your doctor
- Gently cleaning the eye area with a warm, damp cloth
- Avoiding touching or rubbing the eye to prevent infection
Managing Pain and Discomfort
It’s important to manage your baby’s pain and discomfort after surgery. Some babies might feel a little uncomfortable or swollen. We might suggest over-the-counter pain relief for babies, but always check with your pediatrician first.
Follow-up Appointments and Monitoring
Follow-up appointments are key for checking on your baby’s healing. These visits help us see how they’re doing and if everything is okay. How often you need to come back will depend on your baby’s surgeon.
Monitoring for Complications:
Potential Complication | Signs to Watch For | Action to Take |
Infection | Redness, swelling, increased discharge, or fever | Contact your doctor immediately |
Re-obstruction | Continued tearing or eye discharge after initial improvement | Schedule a follow-up appointment |
By following these care tips, you can help your baby recover well from tear duct surgery. If you have any worries or questions, always talk to your healthcare provider for help and advice.
Conclusion: Long-Term Outlook for Infants with Tear Duct Obstruction
The outlook for infants with tear duct obstruction is mostly good. About 90 percent of blocked ducts open up on their own by the first year. This usually happens in the first few months, but can take up to a year.
Knowing the prognosis helps parents and caregivers plan. Most cases get better on their own or with simple treatments. This means the chances of a good outcome are high with proper care.
If surgery is needed, the results are often positive. Pediatric ophthalmologists have high success rates. After treatment, the infant’s tear duct system works well.
FAQ
What is tear duct obstruction in infants?
Tear duct obstruction, or nasolacrimal duct obstruction (NLDO), is when the tear duct gets blocked. This stops tears from draining properly. It’s common in babies and can cause eye problems if not treated.
What are the symptoms of blocked tear ducts in infants?
Signs include too much tearing, eye discharge, redness, and irritation. Spotting these symptoms early is key to getting the right help.
What causes tear duct obstruction in infants?
The main reason is when the tear duct system doesn’t fully form, mainly at the valve of Hasner. Other things might also play a part.
How is tear duct obstruction diagnosed?
Doctors look for symptoms and examine the eyes. A pediatric ophthalmologist can tell if it’s a blockage and suggest treatment.
What are the conservative treatment approaches for tear duct obstruction?
Treatments include massaging the tear duct, keeping the eye clean, and using antibiotic drops for infections. These methods often work without surgery.
When should eye duct surgery be considered for infants?
Surgery might be needed if other treatments don’t work, usually by 12 months. A pediatric ophthalmologist should be consulted to decide the best action.
What is the tear duct probing procedure?
This surgery uses a probe to open the blocked duct. Success rates vary by age, and risks should be talked about with a doctor.
What are the advanced surgical options for persistent tear duct obstruction?
Options include balloon dilation, silicone tube insertion, and dacryocystorhinostomy (DCR). These are for cases where simpler treatments don’t work.
How should I care for my infant after tear duct surgery?
After surgery, follow the doctor’s instructions for aftercare. Manage pain and attend follow-up visits. Proper care helps in a smooth recovery.
What is the long-term outlook for infants with tear duct obstruction?
Most cases improve on their own or with little treatment. Knowing this helps parents plan and manage their expectations.
Can tear duct obstruction resolve on its own?
Yes, many cases clear up by themselves in the first year. But, it’s important to have a doctor check to avoid problems.
What is the role of the valve of Hasner in tear duct obstruction?
The valve of Hasner is key at the end of the tear duct. Not fully forming here often causes blockages.
How effective is tear duct massage in treating tear duct obstruction?
Massage is a helpful treatment, often effective when started early. It helps open the duct and drain tears properly.
What are the possible risks and complications of tear duct probing surgery?
Risks include infection, bleeding, and not fixing the blockage. Discussing these with a doctor helps understand the surgery’s benefits and risks.
Can adults experience tear duct obstruction, and how is it treated?
Adults can also get tear duct blockages, though it’s more common in babies. Treatment for adults might include surgery, but it depends on the cause.
References
National Center for Biotechnology Information. Infant Tear Duct Obstruction: Surgery Versus Conservative Management. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6313586/