Last Updated on December 5, 2025 by Bilal Hasdemir

Receiving a cancer diagnosis for a child is very tough. A pediatric oncologist plays a vital role in guiding families through diagnosis, treatment, and care. Pediatric oncology focuses on treating cancer in kids, and having a skilled pediatric oncologist ensures children receive the best possible outcomes. The time needed for treatment changes based on the cancer type and how advanced it is.
Top hospitals are working hard to find better ways to treat cancer in children. For example, the Pediatric Hematology-Oncology Fellowship Program at the University of Washington is a 3-year program. It trains doctors, including future pediatric oncologists, with the newest methods and knowledge.
Treatment for kids with cancer can take months or even years. But, thanks to new treatments and the expertise of a pediatric oncologist, more kids are surviving. This gives families around the world hope.
Key Takeaways
- Pediatric oncology treatment duration varies by cancer type and stage.
- Advanced medical centers offer cutting-edge care and innovative treatments.
- Specialized fellowship programs enhance the expertise of pediatric hematologists.
- Survival rates for pediatric cancer have significantly improved.
- Comprehensive care is key for the health of young patients.
Understanding Pediatric Oncology
Pediatric oncology is a special field of medicine. It deals with children who have cancer. It’s different from adult cancers because kids’ bodies and diseases are unique.
Definition and Scope of Pediatric Cancer Treatment
Pediatric cancer treatment uses chemotherapy, surgery, and radiation therapy. It’s not just about treating cancer. It also covers the emotional and physical needs of kids with cancer.
Places like the University of Washington’s Pediatric Hematology-Oncology Fellowship offer deep training. They teach both clinical and research skills. Treatment can last from months to years, depending on the cancer type and stage.
Differences Between Pediatric and Adult Oncology
Children and adults have different cancers. Kids often get acute lymphoblastic leukemia (ALL) and brain tumors. Adults usually get breast, lung, and colon cancers.
Treatment plans also vary. Kids get more aggressive treatments to help them grow up without long-term damage. Adults might focus on comfort and managing side effects.
The field of pediatric hematology and oncology needs both knowledge and kindness. Our team is committed to top-notch care and support for families from around the world.
The Role of a Pediatric Oncologist in Cancer Treatment
In the complex world of pediatric cancer treatment, oncologists are key. They bring together expertise, compassion, and the latest medical knowledge. Pediatric oncologists are doctors who specialize in treating children with cancer.

Education and Training Requirements
To become a pediatric oncologist, one must go through a lot of education and training. This includes medical school, residency in pediatrics, and fellowship in pediatric hematology-oncology. For example, the Pediatric Hematology-Oncology Fellowship Program at some places requires fellows to share their work in progress. This helps them learn and get better at treating pediatric cancers.
This training prepares pediatric oncologists to diagnose and manage childhood cancers. They learn about leukemias, lymphomas, and solid tumors. They also learn about the long-term effects of cancer treatment on children’s health.
Specialized Skills and Expertise
Pediatric oncologists have special skills and knowledge for treating childhood cancers. They are good at reading complex tests, making treatment plans for each patient, and managing treatment side effects. They also provide supportive care, meeting the physical, emotional, and psychological needs of their young patients.
The pay for pediatric oncologists shows their advanced training and expertise. The pediatric oncologist pay can change based on location, experience, and employer. But it’s usually in the same range as other specialized medical professionals.
Collaboration with Multidisciplinary Teams
Pediatric oncologists work with many teams to care for children with cancer. These teams include surgeons, radiation oncologists, nurses, social workers, and more. Working together is important for making good treatment plans, managing side effects, and supporting patients and their families.
- Developing and implementing personalized treatment plans
- Coordinating care with other specialists
- Providing emotional and psychological support
- Monitoring long-term effects of cancer treatment
By working together, pediatric oncologists and their teams can greatly improve outcomes for children with cancer. They help increase survival rates and improve quality of life. The role of a pediatric oncologist is not just about treating cancer. It’s about caring for the whole child and supporting their journey towards recovery and beyond.
Treatment Duration for Common Pediatric Cancers
Knowing how long treatments for common pediatric cancers last is key. It helps us manage what to expect and give the best care. Pediatric hematologist oncologists face different cancers, each with its own treatment time and plan.
Acute Lymphoblastic Leukemia (ALL) Treatment Timeline
Acute Lymphoblastic Leukemia (ALL) is the top cancer in kids, making up a big part of pediatric oncology. Treating ALL usually takes 2 to 3 years. It involves several rounds of chemotherapy.
Initial Treatment Phase: The first phase is intense. It lasts a few months. Patients get strong chemotherapy to start fighting the cancer.
Maintenance Therapy: After the first phase, patients start maintenance therapy. This can last up to 2 years. They get less strong chemotherapy to keep the cancer away.
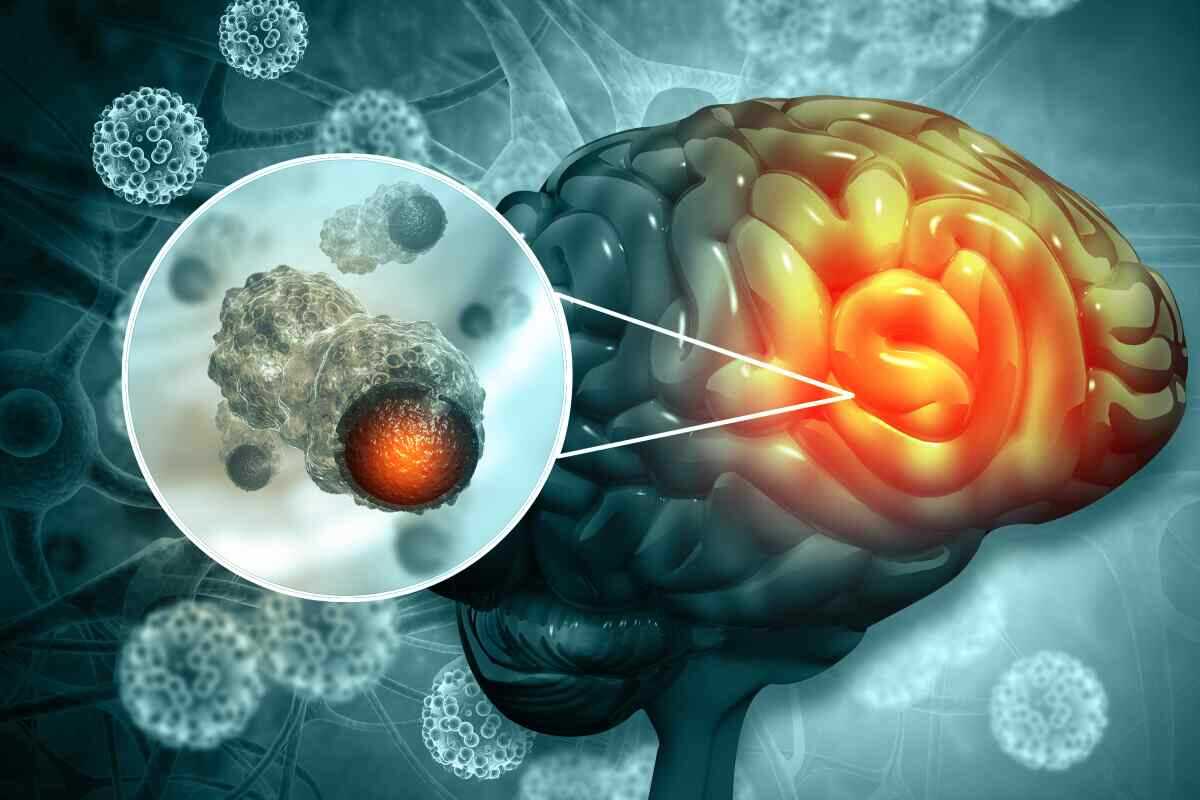
Brain Tumor Treatment Duration
Brain tumors in kids need special treatment plans. These plans often include surgery, radiation, and chemotherapy. The time it takes to treat brain tumors can be quite different, from a few months to a few years.
Seattle Children’s Hospital has a Brain Tumor Program. It offers detailed care, like advanced surgery and targeted treatments. These can change how long treatment lasts.
Solid Tumor Treatment Protocols
Solid tumors, like neuroblastoma and Wilms tumor, need a team effort for treatment. This includes surgery, chemotherapy, and sometimes radiation. The time it takes to treat solid tumors depends on the tumor type, stage, and how well it responds to treatment.
At places like Seattle Children’s Hospital’s Solid Tumor Program, patients get plans made just for them. These plans change based on how they do and their health.
Factors Affecting Treatment Length in Pediatric Oncology
Understanding what affects treatment length is key in pediatric oncology. The time it takes to treat pediatric cancers varies a lot. This is due to several important factors.
Cancer Type and Stage
The type and stage of cancer greatly influence treatment length. Each cancer type has its own treatment plan. The stage at diagnosis also affects how long and intense the treatment will be.
Acute Lymphoblastic Leukemia (ALL), the most common pediatric cancer, usually takes 2-3 years to treat. This includes maintenance therapy.
The University of Washington’s Pediatric Hematology-Oncology Fellowship Program says knowing the biology of pediatric cancers is key. The stage of cancer at diagnosis also impacts treatment length. Early stages often mean shorter treatments.
Patient Age and Overall Health
The age and health of the patient are also important. Younger patients might need special treatment plans because of their developing bodies. Older children might handle more intense treatments.
Children with health issues may need treatment plans adjusted for them. This can affect how long treatment lasts.
A pediatric hematologist specialist notes that a patient’s health and age are key. For example, young children with brain tumors might get lower doses of chemotherapy. This helps avoid long-term side effects.
Response to Initial Treatment
How well a child responds to initial treatment is also a big factor. Children who respond well might need shorter treatments. Those who don’t respond as expected might need longer, more intense treatments.
“The initial response to treatment is a strong predictor of outcome in pediatric oncology,” says a leading pediatric oncologist. “Tailoring treatment based on early response can help optimize outcomes and minimize unnecessary treatment.”
We know every child’s response to treatment is different. Our approach is to keep a close eye and adjust treatment plans as needed. This personalized care aims to get the best results for each child.
Phases of Pediatric Cancer Treatment
It’s key for patients and families to know about the different stages of pediatric cancer treatment. This process is complex and involves many important steps. Each step is vital for the care of the patient.
Diagnosis and Initial Assessment
The first step is diagnosis and initial assessment. This is the foundation of the treatment plan. Specialists do detailed tests like imaging and biopsies to find out the cancer type and stage.
Places like Seattle Children’s Hospital have a detailed Cancer Survivor Program. They make sure every child gets a precise diagnosis and a treatment plan that fits them.
Active Treatment Phase
The next phase is active treatment. This is when the actual treatment happens. It can include chemotherapy, surgery, or radiation. The length of this phase depends on the cancer type, stage, and how well the child responds.
Our team keeps a close eye on the child’s progress. They adjust the treatment plan as needed to get the best results.
Long-term Follow-up Care
The last phase is long-term follow-up care. It’s important for checking the child’s health and catching any late treatment effects. This care can last for years and includes regular visits with a pediatric oncologist.
Our team stresses the need for long-term care. They offer full support to families during and after treatment. Knowing about the treatment phases helps families understand the process better. It ensures their child gets the best care.
Multidisciplinary Approach to Pediatric Oncology
Pediatric oncology is a complex field that needs a team effort to treat children with cancer. This team includes many medical specialties working together. They aim to give the best care to young patients.
At the center of this team are pediatric hematologists and oncologists. They specialize in diagnosing and treating childhood cancers. They work with surgeons, radiologists, and radiation oncologists to create treatment plans for each patient.
Chemotherapy Protocols and Duration
Chemotherapy is key in treating pediatric cancer, often used with other treatments. The type and length of chemotherapy depend on the cancer type, stage, and how the patient responds.
The University of Washington’s Pediatric Hematology-Oncology Fellowship Program focuses on chemotherapy. It shows how important this treatment is in pediatric oncology. Chemotherapy can last from months to years, with treatment plans adjusted as needed.
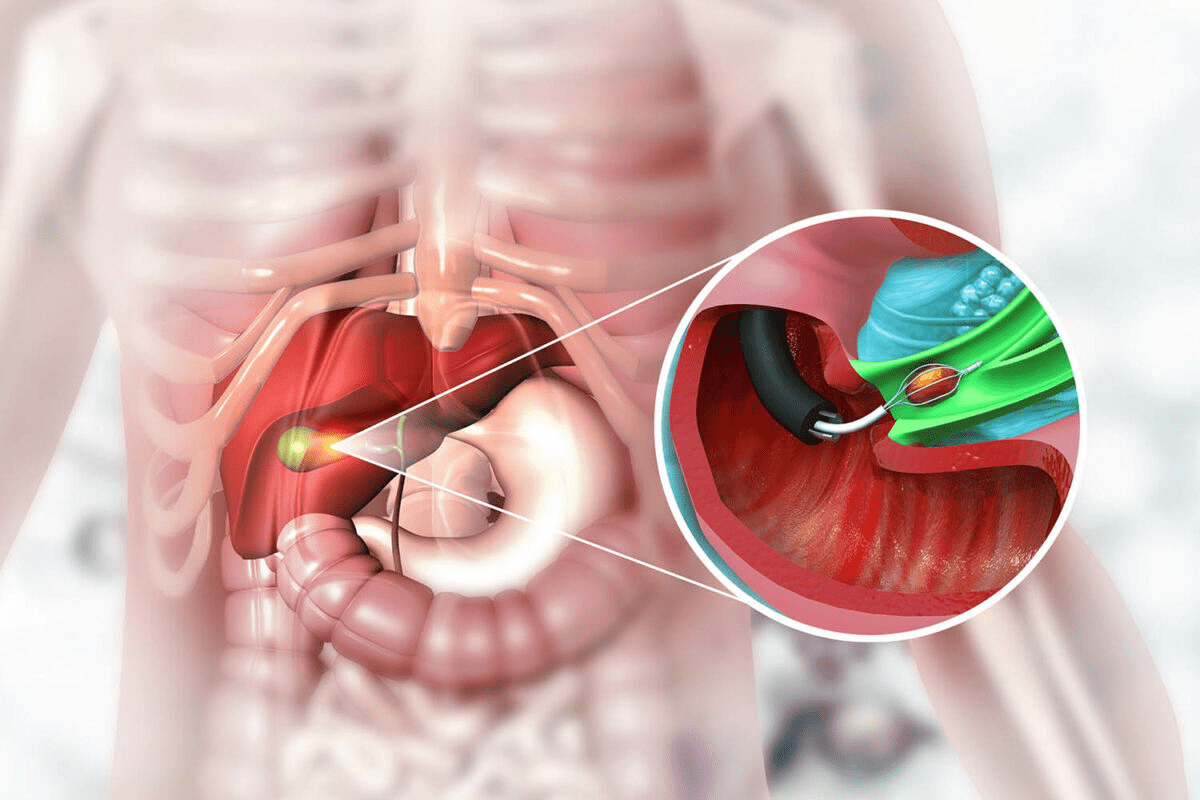
Surgical Interventions and Recovery Time
Surgery is vital in treating many pediatric cancers, like solid tumors. The goal is to remove the tumor without harming nearby tissues or organs.
How long it takes to recover from surgery varies. It depends on the surgery’s complexity and the patient’s health. Pediatric surgeons and oncologists plan post-operative care to help the patient recover well and avoid complications.
Radiation Therapy Schedules
Radiation therapy is also important in pediatric oncology. It targets cancer cells while protecting healthy tissues. The schedule and duration depend on the cancer type, location, and how the patient responds.
Radiation oncologists work with the treatment team to create personalized plans. They aim to be effective while reducing long-term side effects.
By using these treatments together, we can offer complete care to children with cancer. This improves their chances of successful treatment and long-term survival.
Survival Rates and Long-term Outcomes
The world of pediatric oncology has seen big changes. Survival rates for kids with cancer have gone up a lot. This is thanks to better treatments, finding cancer early, and more support care. We’ll look at the latest survival rates and long-term results in pediatric cancer. We’ll also talk about what affects how well a child might do.
Overall 5-Year Survival Statistics
Recent numbers show that over 80% of kids with cancer live for 5 years or more. This big jump shows how far we’ve come in treating kids with cancer. The Children’s Oncology Group (COG) has been key in making treatments better and safer for kids.
Cancer-Specific Survival Rates
It’s important to look at survival rates for each type of cancer. Some cancers have seen bigger jumps in survival rates than others. For example, acute lymphoblastic leukemia (ALL), the most common cancer in kids, now has a 5-year survival rate over 90%. But, some brain and solid tumors are harder to beat, even though survival rates are getting better.
Factors Influencing Prognosis and Treatment Length
Many things can affect how well a child might do and how long treatment will last. These include the type and stage of cancer, the child’s age and health, and how well the cancer responds to treatment. Genetic factors also play a big role. Knowing these helps doctors make treatment plans that are just right for each child.
Challenges in Pediatric Cancer Treatment Timelines
Despite big steps forward in treating pediatric cancer, there are many hurdles. We see that while we’ve made progress, there’s more to do. Ensuring timely and effective care for all patients is a big goal.
Access to Specialized Care Centers
Getting to specialized care centers is a big challenge. The University of Washington’s Pediatric Hematology-Oncology Fellowship Program is a key example. But, not all families can easily get to these centers, causing delays in treatment.
We know that getting to these centers is key for better care. Families face many barriers like distance, cost, and logistics. We need to find ways to overcome these to ensure all patients get the care they need.
Delays in Clinical Trial Implementation
Another big challenge is the slow start of clinical trials for pediatric cancers. These trials are essential for finding new treatments. But, the process of setting them up is long and complicated.
These delays mean patients might not get the latest treatments. This is a big problem for those with rare or aggressive cancers. They need access to new treatments quickly.
Treatment Protocols for Rare Pediatric Cancers
Creating good treatment plans for rare pediatric cancers is hard. There’s not much research or data for these cancers. This makes it tough to set up standard treatment plans.
This lack of standard plans can lead to different care and outcomes. We need to keep researching and finding new treatments. This will help improve care for families with rare cancers.
To improve treatment timelines and outcomes, we must work together. Healthcare providers, researchers, and families need to join forces. This way, we can ensure all patients get the care they need quickly and effectively.
Innovations Shortening Pediatric Oncology Treatment
Recent breakthroughs in pediatric oncology are changing how we treat childhood cancers. These new methods are not just making treatments more effective. They’re also making them shorter for many young patients.
Targeted Therapies and Immunotherapy Advances
Targeted therapies and immunotherapy are leading the charge in pediatric oncology. These treatments aim directly at cancer cells, sparing healthy tissues. For example, Seattle Children’s Hospital is a top name in immunotherapy research and treatment. They provide advanced care to kids with cancer.
- Immunotherapy: Uses the body’s immune system to combat cancer.
- CAR-T cell therapy: A promising immunotherapy for leukemia and lymphoma.
- Targeted therapies: Drugs that target cancer cells, lowering side effects.
Precision Medicine Approaches
Precision medicine is changing pediatric oncology by tailoring treatments to each patient’s genetic makeup. This method leads to more effective treatments with fewer side effects.
- Genetic profiling: Finds specific genetic mutations in cancer.
- Personalized treatment plans: Created based on the tumor’s genetic profile.
- Continuous monitoring: Adjusts treatment based on patient response.
Innovative Hospitals and Treatment Centers
Institutions like Seattle Children’s Hospital are at the forefront of pediatric oncology care. These centers offer top-notch treatment and drive research and innovation.
By combining hematology pediatric and pediatric hem onc expertise, these places are boosting cancer treatment outcomes for kids. Their teams work together to give kids full care, from diagnosis to long-term follow-up.
Support Systems Throughout Extended Cancer Treatment
Support systems are key during long cancer treatments for kids. They help with medical, emotional, and mental health needs. Families and kids get better care with a strong support network.
Family-Centered Care Models
Family-centered care is vital in treatment. It makes sure families are part of the care plan. This way, both the patient and family needs are met.
The University of Washington’s Pediatric Hematology-Oncology Fellowship Program focuses on this. It helps families make decisions, leading to better care.
These models bring together doctors and families. Pediatric hematologist oncologists work with families to create plans that fit the child’s needs. This approach improves care and makes the experience better for families.
Psychosocial Support During Long-Term Treatment
Psychosocial support is also key for kids with cancer. Long treatments can affect a child’s and family’s mental health. Services like counseling help lessen these effects.
Teams with psychosocial experts offer important support. They provide counseling, group therapy, and support groups. These offer a safe place for families to share and get help.
In summary, support systems are essential for families and kids with long cancer treatments. Family-centered care and psychosocial support improve the treatment experience and outcomes for young patients.
Conclusion
Pediatric oncology treatment is complex and needs a detailed approach. It involves specialized care and teams from different fields. We’ve looked at how long treatment lasts, what affects its length, and the need for ongoing research.
The University of Washington’s Pediatric Hematology-Oncology Fellowship Program is a top example. It shows the importance of advanced education and training in this field. To become a specialist, one must go through tough training and keep up with new discoveries.
Improving treatment outcomes and shortening treatment time is key. We must invest in research and innovation in pediatric oncology. This way, we can give the best care to children with cancer and support their families.
FAQ
What is pediatric oncology?
Pediatric oncology is a branch of medicine. It deals with the diagnosis and treatment of cancer in children.
How long does pediatric cancer treatment typically last?
Treatment time varies. It depends on the cancer type and stage. It can last from months to years.
What are the common types of pediatric cancer?
Common types include acute lymphoblastic leukemia (ALL), brain tumors, and solid tumors.
What is the role of a pediatric oncologist in cancer treatment?
Pediatric oncologists work with other healthcare professionals. They provide care to children with cancer. This improves survival rates and treatment outcomes.
How does pediatric oncology differ from adult oncology?
Pediatric oncology is different from adult oncology. It deals with different cancer types and treatment options. It also considers the unique needs of children.
What are the factors that affect treatment length in pediatric oncology?
Treatment length is affected by several factors. These include the cancer type and stage, the patient’s age and health, and how well they respond to treatment.
What are the phases of pediatric cancer treatment?
Pediatric cancer treatment has several phases. These include diagnosis and initial assessment, active treatment, and long-term follow-up care.
How do pediatric oncologists determine the best treatment approach?
Pediatric oncologists use a team approach. They consider the cancer type, stage, and patient needs to determine the best treatment.
What is the importance of follow-up care in pediatric oncology?
Follow-up care is vital in pediatric oncology. It helps monitor long-term effects of treatment. It ensures the best outcomes for patients.
What are some of the challenges in pediatric cancer treatment timelines?
Challenges include access to specialized care centers. Delays in clinical trial implementation and treatment for rare cancers also pose challenges.
How are innovations in treatment options improving pediatric oncology?
Innovations like targeted therapies and immunotherapy are improving outcomes. They are also reducing treatment duration in pediatric oncology.
What support systems are available for families throughout extended cancer treatment?
Families have access to support systems. These include family-centered care models and psychosocial support. They help families cope with extended treatment.
What is the average salary of a pediatric oncologist?
A pediatric oncologist’s salary varies. It depends on location, experience, and institution. It is generally competitive with other medical specialties.
How can I become a pediatric hematologist oncologist?
To become a pediatric hematologist oncologist, you need to complete medical school, residency, and fellowship in pediatric hematology and oncology.
References
- Molla, Y. M., et al. (2025). The magnitude and associated factors of childhood cancer treatment abandonment at the University of Gondar Comprehensive Specialized Hospital, Ethiopia. Scientific Reports. https://www.nature.com/articles/s41598-025-90493-3
- DuBois, S. G., et al. (2019). Children wait for new cancer drugs 6.5 years longer than adults. Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. Retrieved from https://answers.childrenshospital.org/wait-time-pediatric-cancer-drug-trials/