Last Updated on December 2, 2025 by Bilal Hasdemir
CSF Leak After Craniotomy
Cerebrospinal fluid leaks after craniotomy worry both patients and neurosurgeons. Studies show these leaks happen in about 7.1% of cases.
It’s important to know about these leaks to help patients and improve care after surgery. We’ll look at what causes these leaks and their impact on patients having craniotomy.
A CSF leak can be serious. It might cause infections, longer hospital stays, and more surgeries. It’s key for patients to understand the risks. Also, doctors should work to lower these risks.
Key Takeaways
- Cerebrospinal fluid leaks occur in a significant percentage of craniotomy cases.
- The incidence rate varies, with some studies indicating a rate of around 7.1%.
- Understanding the risks is crucial for patient care and management.
- Cerebrospinal fluid leaks can lead to serious complications.
- Awareness and preventive strategies are key to minimizing risks.
Understanding Cerebrospinal Fluid and Its Function

A detailed cross-sectional view of the human brain, showcasing the intricate network of cerebrospinal fluid circulation. The image should depict the brain in a warm, muted color palette, with a focus on the ventricles, subarachnoid space, and the flow of the clear, watery fluid. Employ a realistic, high-resolution photographic style, with a shallow depth of field to highlight the anatomical structures. Ensure the image conveys a sense of depth and three-dimensionality, allowing the viewer to appreciate the complex interplay between the brain, spinal cord, and the cerebrospinal fluid system. The overall mood should be informative and educational, inspiring a deeper understanding of this vital physiological process.
Grasping cerebrospinal fluid is key to understanding brain protection and maintenance. Cerebrospinal fluid (CSF) is a clear, colorless body fluid in the brain and spine. It plays crucial roles for the central nervous system’s health.
What is Cerebrospinal Fluid?
Cerebrospinal fluid is made in the choroid plexus of the brain’s ventricles. It’s mostly water, with proteins, glucose, and other substances. CSF is constantly made and absorbed, with its composition and pressure strictly controlled.
The Role of CSF in Brain Protection
CSF is vital for protecting the brain and spinal cord. It acts as a cushion, shielding these vital areas from harm. It also helps exchange nutrients and waste between the brain and blood stream. This is key for the central nervous system’s health.
Normal CSF Production and Circulation
An average adult makes about 500 milliliters of CSF daily. The total CSF volume in the body is around 125-150 milliliters. CSF is made by the choroid plexus and flows through the ventricular system and subarachnoid space. It’s then absorbed into the bloodstream through the arachnoid villi.
Characteristic | Normal Value |
Appearance | Clear, Colorless |
Protein Level | 15-45 mg/dL |
Glucose Level | 50-80 mg/dL |
Pressure | 5-15 mmHg (lateral recumbent position) |
In conclusion, cerebrospinal fluid is crucial for the central nervous system’s protection and upkeep. Its production, circulation, and absorption are tightly regulated. These processes are essential for neurological health.
What is a Craniotomy?
a high-quality, highly detailed medical illustration of a craniotomy surgical procedure, depicting the various stages and steps involved in the operation. The image should show the patient’s head with the scalp incision, the removal of a section of the skull, and the exposure of the underlying brain tissue. The surgical instruments, such as the scalpel, bone saw, and retractors, should be clearly visible. The scene should be well-lit, with a crisp, clean, and precise presentation. The overall mood should be one of clinical professionalism and medical accuracy, conveying the technical complexity and importance of the procedure. The image should be suitable for use in a medical reference or educational context.
A craniotomy is a surgical procedure where a part of the skull is removed temporarily. This allows surgeons to access the brain. It’s key for many neurosurgical treatments.
Definition and Purpose
A craniotomy means removing part of the skull, called a bone flap. It lets surgeons get to the brain. This is vital for treating brain issues.
The bone flap is taken out to let surgeons work on the brain. They might fix aneurysms, remove tumors, or ease pressure from trauma. After the surgery, the bone flap is put back and secured.
Common Reasons for Craniotomy Procedures
Craniotomies are done for many important reasons, including:
- Removing brain tumors or cysts
- Repairing aneurysms or arteriovenous malformations (AVMs)
- Draining abscesses or hematomas
- Relieving pressure on the brain due to trauma
- Treating epilepsy by removing the seizure focus
These surgeries can save lives and greatly improve patients’ lives.
Overview of the Surgical Process
The surgical process of a craniotomy has several steps. First, the patient is prepared with anesthesia and positioning. Then, the scalp is incised, and a skull section is removed to reach the brain.
Once the surgery is done, the bone flap is put back, and the scalp is closed. A team of neurosurgeons, anesthesiologists, and nurses work together for the best results.
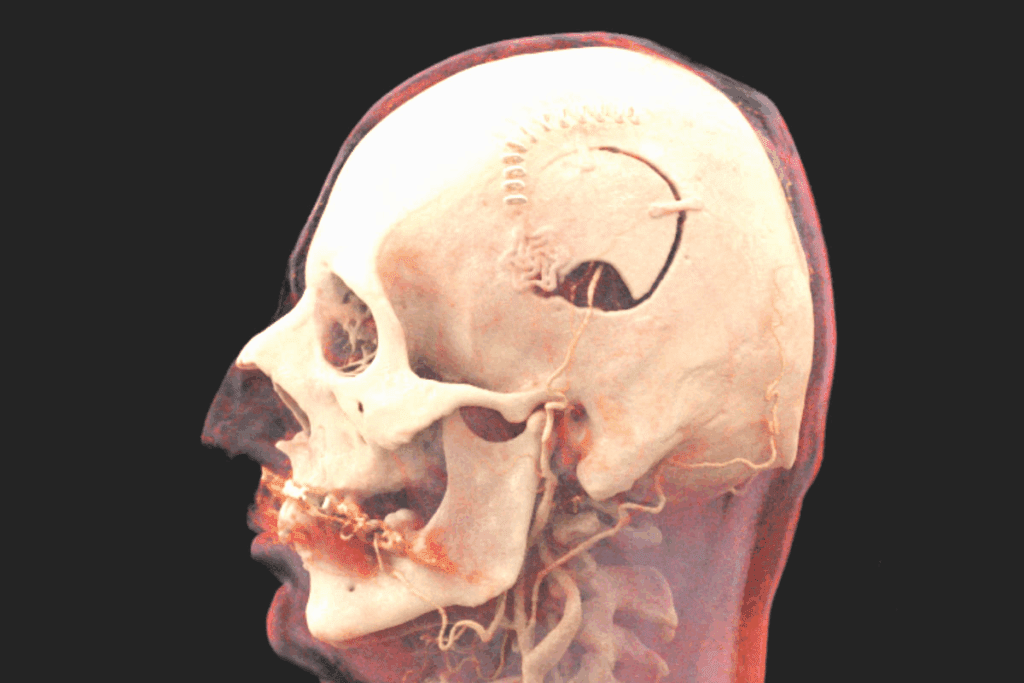
CSF Leak After Craniotomy: Definition and Mechanism
A high-resolution, photorealistic image of a cross-section view of the human head, revealing the intricate anatomy of a cerebrospinal fluid (CSF) leak. The image should clearly depict the dura mater (protective membrane) of the brain, the arachnoid membrane, and the subarachnoid space where the CSF flows. The leak should be shown as a visible breach or opening in the dura mater, allowing the CSF to escape from its normal pathways. The surrounding bony structures, such as the skull and cranium, should be visible to provide context and scale. The lighting should be soft and directional, highlighting the delicate details of the anatomy. The overall mood should convey the clinical and medical nature of the subject matter.
It’s important for surgeons and patients to know about CSF leaks after craniotomy. A cerebrospinal fluid (CSF) leak is a serious issue that can happen during or after brain surgery.
What Constitutes a CSF Leak
A CSF leak happens when cerebrospinal fluid escapes through a hole in the dura mater. This is the protective layer around the brain and spinal cord. Such leaks can cause infections, meningitis, and even air in the brain.
Doctors usually diagnose a CSF leak by looking at symptoms like headaches, nausea, and clear fluid coming from the wound or nose.
How CSF Leaks Occur During or After Surgery
CSF leaks can happen for several reasons during or after a craniotomy. These include:
- Incomplete closure of the dura mater
- Infection or wound complications
- Increased intracranial pressure
The risk of CSF leak is higher during surgery. This is because of the surgery’s complexity and the patient’s health.
Types of Post-Craniotomy CSF Leaks
There are different types of CSF leaks that can happen after a craniotomy. These include:
Type of Leak | Description | Common Causes |
Wound Leak | CSF leakage through the surgical wound | Incomplete wound closure, infection |
Nasal Leak (Rhinorrhea) | CSF leakage through the nose | Fracture or defect in the cribriform plate |
Otic Leak (Otorrhea) | CSF leakage through the ear | Damage to the temporal bone or auditory canal |
Understanding the types and causes of CSF leaks is essential for effective prevention and management.
Incidence Rates: How Common Are CSF Leaks?
A detailed and realistic medical illustration showcasing the incidence rates of cerebrospinal fluid (CSF) leaks following craniotomy procedures. The foreground features a cross-section of the human skull, highlighting the dura mater and brain tissue. In the middle ground, a series of bar graphs and line charts depict the statistical data on CSF leak rates, presented in a clear and informative manner. The background maintains a clinical, sterile atmosphere with muted colors and subtle medical imagery, such as surgical instruments or anatomical diagrams. The lighting is soft and diffused, creating depth and emphasizing the technical details. The overall composition conveys a sense of professionalism and authority, suitable for inclusion in a medical journal or academic publication.
CSF leaks are a common problem after craniotomy. Different studies show different rates of these leaks. Knowing these rates helps us understand the risks of craniotomy.
Statistical Overview of CSF Leak Occurrence
Research shows CSF leaks happen in 4% to 10% of cases after craniotomy. On average, about 6% of patients experience a leak. This range shows the importance of studying what causes these leaks.
- Reported incidence rates range from 4% to 10% in various studies.
- The average incidence rate is around 6%, based on a comprehensive review of recent literature.
- Factors such as surgical technique and patient health contribute to the variability in incidence rates.
Variation in Incidence by Procedure Type
The type of craniotomy affects the risk of CSF leaks. For example, procedures involving the frontal sinus are associated with a higher risk of CSF leaks. Knowing this helps doctors plan better for each patient.
Procedure Type | Incidence Rate (%) |
Frontal Craniotomy | 8-12 |
Temporal Craniotomy | 4-8 |
Occipital Craniotomy | 3-6 |
Trends in CSF Leak Rates Over Time
New surgical methods and better care have lowered CSF leak rates. These improvements are expected to keep reducing leak rates. Watching these changes helps us see how well our treatments are working.
By looking at CSF leak rates and what affects them, doctors can improve patient care. This leads to better results for everyone.
Risk Factors for Developing a CSF Leak
Realistic close-up view of the human head, revealing the inner anatomy and key risk factors for a cerebrospinal fluid (CSF) leak. Detailed depiction of the skull, dura mater, and arachnoid membrane. Clearly highlight potential weaknesses or openings that could lead to CSF leakage, such as craniotomy sites, trauma, congenital defects, or previous surgery scars. Employ a high-quality medical illustration style, with soft lighting and muted colors to convey the seriousness and importance of the subject. Ensure the overall composition directs the viewer’s attention to the critical risk factors in a clear, informative manner.
Several factors can increase the risk of a CSF leak after a craniotomy. It’s important for healthcare providers to know these risks. This helps them take steps to prevent and manage complications.
Patient-Related Risk Factors
Some patient characteristics can make a CSF leak more likely. These include:
- Younger Age: Younger patients might face a higher risk of CSF leaks. This is because they are often healthier and more active after surgery.
- Higher BMI: People with a higher Body Mass Index (BMI) may have more pressure inside their skull. This can increase the risk of a CSF leak.
- Smoking: Smoking can harm wound healing. It also weakens tissue, making CSF leaks more likely.
Surgical Technique-Related Factors
The way a craniotomy is done can also affect the risk of a CSF leak. Important factors include:
- Infratentorial Surgery: Surgeries in the infratentorial area are riskier for CSF leaks. This is because of the complex anatomy and challenges in closing the dura mater tightly.
- Dural Closure Techniques: How the dura mater is closed during surgery is crucial. Techniques that ensure a tight seal are key to preventing leaks.
Post-Operative Behavioral Factors
What patients do after surgery can also affect the risk of a CSF leak. Important factors include:
- Activity Level: Doing too much too soon can raise pressure inside the skull. This increases the risk of a CSF leak.
- Adherence to Post-Operative Instructions: Following the doctor’s advice on rest, positioning, and care can lower the risk of complications. This includes CSF leaks.
Understanding and addressing these risk factors helps healthcare providers. They can take steps to reduce the chance of CSF leaks in patients after a craniotomy. This improves patient outcomes.
Recognizing the Symptoms of a CSF Leak
A high-resolution, photorealistic image of common symptoms of a cerebrospinal fluid (CSF) leak, as seen in a close-up view. The scene depicts a person’s head and upper shoulders, with visible signs of the condition such as a clear fluid seeping from the nose or ear, swelling around the incision site, or a persistent headache. The lighting is soft and diffused, with a warm, natural color palette that highlights the details of the skin and facial features. The image is captured at a slightly elevated angle to provide a clear view of the affected areas, conveying a sense of clinical examination or medical observation.
It’s important to know the signs of a cerebrospinal fluid (CSF) leak. This is especially true for those who have had a craniotomy. Being aware of these signs can help get the right treatment quickly.
Common Clinical Presentations
CSF leaks can show up in different ways. You might feel a headache, nausea, or vomiting. These happen because the fluid pressure inside your head drops.
The headache from a CSF leak gets worse when you’re standing up. It feels better when you lie down. Other symptoms include:
- Dizziness or vertigo
- Neck pain or stiffness
- Tinnitus or hearing changes
- Photophobia or sensitivity to light
Immediate vs. Delayed Symptoms
There are two types of symptoms from a CSF leak. Immediate symptoms happen right after surgery. Delayed symptoms can show up days or weeks later.
Watching for any signs of CSF leakage is key. Finding it early can make treatment much more effective.
When to Seek Medical Attention
If you notice any of these, get help right away:
- Severe or worsening headache
- Confusion or altered mental status
- Fever or signs of infection
- Clear fluid drainage from the nose or ear
Acting fast on CSF leaks is vital. It helps avoid serious problems and ensures the best results.
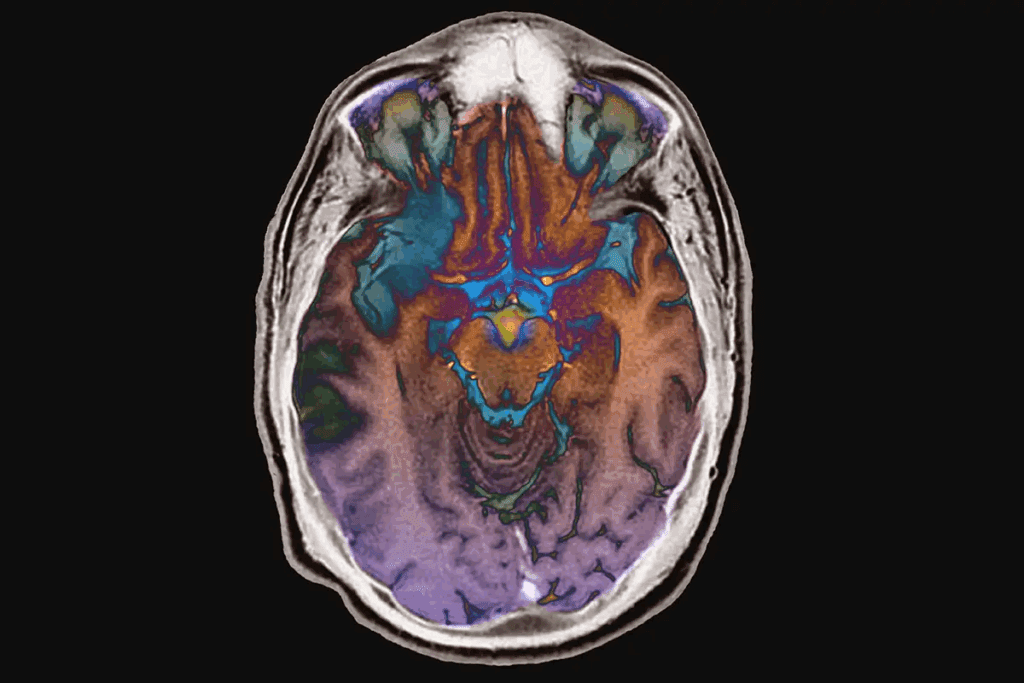
Diagnostic Approaches for CSF Leaks
A high-resolution, photorealistic image of a medical diagnostic procedure for a cerebrospinal fluid (CSF) leak. The scene depicts a patient undergoing a radiological imaging test, such as a computed tomography (CT) or magnetic resonance imaging (MRI) scan. The patient is lying on an examination table, surrounded by advanced medical imaging equipment. The foreground shows the patient’s head and neck area, with the imaging device positioned close to capture detailed views of the cranial and spinal regions. The middle ground includes the medical staff operating the imaging system, wearing professional attire and focused on the diagnostic process. The background showcases a modern, well-equipped medical facility with clean, sterile surfaces and diagnostic equipment. The overall mood is serious and clinical, conveying the importance of accurately diagnosing a CSF leak.
Diagnosing a CSF leak requires a detailed strategy. This includes clinical checks, lab tests, and imaging. We use various tools to find and treat CSF leaks accurately.
Physical Examination Findings
A detailed physical check is key in spotting a CSF leak. We look for signs like nasal or ear discharge. Clear, watery discharge is a common sign that needs more testing.
We also review the patient’s medical history and do a neurological check. This helps find any related issues or complications.
Laboratory Tests for CSF Detection
Labs are crucial in confirming a CSF leak. We test nasal or ear discharge for CSF. The β2-transferrin assay is a common test because it’s very specific for CSF.
Laboratory Test | Description | Specificity for CSF |
β2-transferrin assay | Detects the presence of β2-transferrin protein in nasal or ear discharge | High |
Glucose testing | Measures glucose levels in nasal or ear discharge | Moderate |
CSF tracer studies | Involves injecting a tracer into the CSF to track its movement | High |
Imaging Studies in Diagnosis
Imaging is vital for finding and pinpointing CSF leaks. We use CT scans, MRI, and CT cisternography. These help us see the problem clearly.
CT scans spot bone defects and where CSF might leak. MRI is great for soft tissue issues and finding leaks. CT cisternography uses contrast to show the CSF space and where it’s leaking.
“Imaging studies, particularly CT and MRI, play a crucial role in diagnosing and managing CSF leaks. They help identify the site of leakage and guide treatment decisions.”
— Neurosurgical Guidelines
By combining physical checks, lab tests, and imaging, we can accurately diagnose and manage CSF leaks. This improves patient outcomes.
Impact of Surgical Techniques on CSF Leak Risk
It’s key to know how different surgical methods affect CSF leak risk. The method used can greatly change the chance of complications like CSF leaks after surgery.
Dural Closure Methods and Their Effectiveness
Dural closure is a vital part of craniotomy surgery. It directly affects the risk of CSF leaks. Techniques like sutures, staples, and sealants are used to improve dural closure. Effective dural closure is essential to prevent CSF leaks by creating a tight seal.
Studies have found that advanced sealants and careful suturing can lower CSF leak rates. For example, using dural sealants can make the dural closure stronger, reducing the chance of leaks after surgery.
Minimally Invasive vs. Traditional Approaches
The debate between minimally invasive and traditional surgeries is ongoing. Minimally invasive surgeries have smaller cuts and less tissue damage, which might lower CSF leak risk. But, they can make dural closure harder due to limited visibility.
Traditional open surgeries, on the other hand, provide better visibility and access for dural closure. They have larger cuts and more tissue damage, which can raise CSF leak risk. The choice between these methods depends on the patient’s needs and the surgery’s specifics.
Innovations in Reducing CSF Leak Risk
New surgical techniques and materials are promising in lowering CSF leak risk. The creation of advanced dural sealants and closure devices has improved craniotomy outcomes. Also, minimally invasive surgical techniques have become more precise and safe.
We’re moving towards more tailored and precise surgeries. This is thanks to better imaging and surgical technology. These advancements are vital for better patient results and less CSF leak risk after craniotomy.
Conservative Management of CSF Leaks
Managing CSF leaks can often be done without surgery. We use several methods to help patients recover after a craniotomy. These strategies aim to lower the risk of complications and support healing.
Bed Rest and Positioning
Bed rest and careful positioning are key. They help reduce pressure inside the skull and lower the chance of more leaks. Patients are usually told to stay in a certain position to help the leak close on its own.
Hydration and Medication Management
Drinking enough water is very important. It helps make more cerebrospinal fluid and keeps it moving. Some medicines may also be given to help with symptoms and healing.
CSF Drainage Techniques
CSF drainage techniques are used in some cases. They help lower pressure and aid in healing. This might include using lumbar drains to move CSF away from the leak site.
The success of these methods can depend on the individual case and how bad the leak is. It’s important to keep an eye on the patient and adjust treatment as needed.
Management Strategy | Description | Benefits |
Bed Rest | Reducing physical activity to minimize intracranial pressure | Reduces risk of further leakage |
Hydration | Maintaining adequate fluid intake | Supports CSF production and circulation |
CSF Drainage | Using lumbar drains to divert CSF | Reduces pressure at the leak site, facilitating healing |
Surgical Interventions for CSF Leak Repair
When other treatments don’t work, surgery might be needed for a CSF leak. This is a key step for leaks that don’t get better with initial treatments.
Indications for Surgical Repair
Surgery is needed if a CSF leak doesn’t get better or gets worse. Symptoms like severe headaches, nausea, or infection signs also point to surgery.
- Persistent CSF leak despite bed rest and hydration
- Presence of significant symptoms or signs of infection
- Failure of conservative management to resolve the leak
Common Repair Techniques
Several surgical methods are used to fix CSF leaks, including:
Technique | Description | Success Rate |
Direct Closure | Suturing or stapling the dura mater | 85-90% |
Grafting | Using a graft to reinforce the dura | 80-95% |
Sealant Application | Applying sealants to the leak site | 70-85% |
Success Rates of Surgical Interventions
The success of surgery for CSF leaks depends on the method and the case. Direct closure and grafting usually work better than sealants alone.
Most patients see their symptoms improve after surgery. The right technique depends on the leak’s details and the patient’s health.
Complications Associated with Untreated CSF Leaks
Untreated cerebrospinal fluid (CSF) leaks after brain surgery can be very dangerous. It’s important for patients and doctors to know about these risks. This way, they can get the right treatment quickly.
Infection Risks and Meningitis
One big risk is getting infections, like meningitis. Meningitis is when the membranes around the brain and spinal cord get inflamed. This usually happens because of an infection. A CSF leak can let bacteria into the brain, causing infection.
Key infection risks include:
- Bacterial meningitis: A serious infection that can harm the brain, cause hearing loss, and even be fatal if not treated right away.
- Post-surgical infections: Having a CSF leak makes it more likely to get infections at the surgery site.
Infection Type | Risks | Consequences |
Bacterial Meningitis | Entry of bacteria through the dura mater breach | Brain damage, hearing loss, death |
Post-surgical Infections | Increased risk due to CSF leak | Delayed healing, further complications |
Pneumocephalus and Brain Herniation
Untreated CSF leaks can also cause pneumocephalus. This is when air gets into the brain. It happens when there’s a hole between the outside and inside of the skull. In bad cases, it can push brain tissue across skull structures, which is very dangerous.
The risks of pneumocephalus and brain herniation show why treating CSF leaks fast is so important.
Long-term Neurological Consequences
CSF leaks that aren’t treated can also cause long-term brain problems. These can include headaches that never go away, problems with thinking, and other brain issues. This is because CSF keeps leaking, and there’s a chance for more infections or air in the brain.
We stress that finding and treating CSF leaks early is key. It helps avoid these serious problems and gives patients the best chance for recovery.
Prevention Strategies for CSF Leaks
To prevent CSF leaks, we assess patient risks, use careful surgical methods, and focus on post-operative care. Understanding how to prevent CSF leaks helps us lower the chance of this problem.
Pre-Operative Planning and Risk Assessment
Preventing CSF leaks starts with careful planning and risk checks. We look at factors like age, health, and past surgeries to spot risks. This helps us adjust our surgery and care to lower these risks.
Advanced imaging, like MRI, helps us see the patient’s skull and find weak spots. This lets us plan our surgery to avoid harming important areas.
Intra-Operative Preventive Measures
During surgery, we take steps to prevent CSF leaks. One key method is making sure the dura is closed tightly. We use special materials and techniques for this.
We also try to avoid damaging tissues and keep important areas safe. Using less invasive methods can help with healing.
Post-Operative Care Protocols
After surgery, we watch the patient closely to prevent leaks. We manage pressure in the skull and avoid activities that raise it. This includes heavy lifting or straining.
We also teach patients how to care for their wound and the importance of follow-up visits. Following these steps helps us catch and fix any problems early.
Prevention Stage | Key Measures | Benefits |
Pre-Operative | Risk assessment, advanced imaging | Tailored surgical approach, reduced risk |
Intra-Operative | Meticulous dural closure, minimally invasive techniques | Watertight closure, reduced tissue trauma |
Post-Operative | Monitoring, intracranial pressure management | Early detection of complications, improved outcomes |
By taking a full approach to preventing CSF leaks, we can greatly improve patient results and cut down on complications. Our focus on quality care, from planning to recovery, shows our commitment to our patients’ health.
Patient Recovery and Follow-Up Care
After a craniotomy, managing recovery is key. We focus on healing and avoiding complications like CSF leaks. Our care covers both immediate recovery and long-term health.
Typical Recovery Timeline
The recovery time after a craniotomy varies. It depends on health, surgery complexity, and complications. Patients usually stay in the hospital for a few days to a week.
During this time, we watch for CSF leaks or other issues. Full recovery, including strength and activity return, can take weeks to months.
Key aspects of the recovery timeline include:
- Immediate post-surgery care in the ICU or recovery room
- Monitoring for potential complications, including CSF leaks
- Gradual mobilization and rehabilitation
- Follow-up appointments to assess healing progress
Monitoring Protocols After Discharge
After leaving the hospital, patients follow a monitoring plan. This ensures a smooth recovery and quickly spots any issues, like CSF leaks. The plan includes:
- Regular follow-up appointments with the neurosurgical team
- Monitoring for symptoms that could indicate a CSF leak, such as headache, nausea, or clear discharge from the wound
- Adherence to post-operative instructions regarding rest, activity levels, and wound care
We also teach patients and caregivers to recognize complications and when to seek help.
Long-term Follow-Up Considerations
Long-term care is crucial for checking on neurological recovery and managing late complications. This may involve:
- Periodic imaging studies to monitor for any changes or complications
- Neurological evaluations to assess recovery and function
- Adjustments to rehabilitation plans as needed
Our team provides ongoing support and care to patients and their families.
Recent Advances in CSF Leak Management
CSF leak management has seen big changes thanks to new sealants and diagnostic tools. These updates help improve patient care and lower the chance of problems from CSF leaks.
New Sealant Materials and Technologies
New sealant materials have changed how we handle CSF leaks. They help close dural defects better, cutting down leak risks. Some key improvements include:
- Bioadhesives: These materials stick to wet surfaces well, creating a strong seal.
- Synthetic Dural Substitutes: These substitutes are more friendly to the body and lower infection risks.
- Hydrogel Sealants: These can hold a lot of water, making them great for sealing leaks.
Emerging Diagnostic Tools
New tools are key for spotting and managing CSF leaks. Some recent highlights are:
- Advanced Imaging Techniques: MRI with special contrast is getting better, helping see leaks clearer.
- Biomarkers: Finding specific biomarkers in CSF helps diagnose leaks and check treatment success.
- Point-of-Care Tests: These tests let doctors quickly diagnose and act at the bedside.
Research Directions in Prevention and Treatment
Research in CSF leak management is moving forward, with exciting areas to explore:
Research Area | Description | Potential Impact |
Personalized Medicine | Tailoring treatment to fit each patient | Could lead to better results with therapy tailored to each person |
Stem Cell Therapy | Using stem cells to fix dural defects | Could help grow back damaged tissues |
Advanced Biomaterials | Creating materials that adjust to body changes | Could make sealants last longer and work better |
These new developments and research paths show how fast CSF leak management is evolving. As we keep pushing the boundaries, we’ll see better results for patients after craniotomy surgeries.
Conclusion
It’s important to know about the risks and complications of craniotomy for good patient care. A CSF leak after craniotomy is a big worry because it can cause serious problems. We’ve talked about what CSF leaks are, how common they are, who’s at risk, their symptoms, how to diagnose them, and how to manage them.
Handling CSF leaks after craniotomy needs a detailed plan. This plan should include both non-surgical and surgical steps. It’s key to spot the signs of a CSF leak early and start the right treatment. This helps avoid long-term brain damage. Knowing about craniotomy complications, like CSF leaks, helps doctors and nurses create better prevention and treatment plans.
New ways to deal with CSF leaks, like better sealants and new tests, have made things better for patients. As we learn more about CSF leaks and how to manage them, we can give patients even better care. It’s crucial to handle CSF leaks well to lower the chance of brain surgery problems and help patients recover fully.
FAQ
What is a cerebrospinal fluid (CSF) leak, and how does it occur after a craniotomy?
A CSF leak happens when fluid around the brain and spinal cord leaks out. This can happen after a craniotomy if the dura mater isn’t closed well. It might also be due to how the surgery was done or the care after it.
What are the common symptoms of a CSF leak after craniotomy?
Common signs include headaches, nausea, vomiting, and clear fluid from the surgical site or nose. Some people might not notice symptoms right away, so it’s important to watch for any unusual signs after surgery.
How is a CSF leak diagnosed?
To diagnose a CSF leak, doctors do a physical check, lab tests, and imaging like MRI or CT scans. These help find and locate the leak.
What are the risk factors for developing a CSF leak after craniotomy?
Risk factors include things like age, being overweight, or having had surgery before. The type of craniotomy and how the dura is closed also play a part. So does how active you are after surgery.
How can CSF leaks be prevented?
To prevent CSF leaks, doctors plan carefully before surgery. They use special techniques during surgery and follow strict care plans after. This includes watching for signs of a leak and managing how active you can be.
What are the treatment options for a CSF leak?
Treatment can range from rest, staying hydrated, and taking medicine to surgery. The choice depends on how bad the leak is and how long it lasts.
What are the potential complications of an untreated CSF leak?
Not treating a CSF leak can lead to serious problems. These include infections, air in the brain, brain swelling, and long-term brain damage. This shows why it’s so important to treat it quickly.
How do surgical techniques impact the risk of CSF leaks?
The way surgery is done can affect the risk of CSF leaks. New methods and materials are being developed to make this risk lower.
What is the typical recovery process after a craniotomy, and how is a CSF leak monitored?
After a craniotomy, you’ll be watched for signs of a CSF leak. You’ll manage symptoms and follow a care plan. It’s also important to keep up with follow-up visits to catch any issues early.
What advancements have been made in CSF leak management?
New sealants and diagnostic tools are being developed. There’s also ongoing research into better prevention and treatment. All these aim to improve care for patients with CSF leaks.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34499261/