Last Updated on November 25, 2025 by
Bladder removal, or cystectomy, is a big deal because it’s complex and changes the urinary tract a lot. We know it’s scary to think about cystectomy surgery. We’re here to help you understand it better. Radical cystectomy means taking out the whole bladder, and it’s often needed for bladder cancer.
In this article, we’ll dive into what bladder removal surgery is all about. We’ll talk about why it’s done and what recovery is like.
Bladder removal surgery is a big deal for those facing it. It’s called a cystectomy and removes the bladder. This is often needed for bladder cancer or other serious urinary issues.

Bladder removal surgery takes out part or all of the bladder. Sometimes, nearby organs like the prostate or uterus are removed too. It’s needed for bladder cancer, severe incontinence, and some neurological problems.
Doctors decide if surgery is needed based on the condition’s severity and the patient’s health. We’ll look at why bladder removal is sometimes necessary.
Bladder removal surgery is chosen when other treatments fail. The main reasons include:
Bladder removal surgery is for those with specific medical issues that haven’t been helped by other treatments. This includes:
Knowing why bladder removal surgery is needed helps patients prepare. It also helps them understand the changes in their urinary system after surgery.
A radical cystectomy is a big deal because it’s complex and changes a patient’s life a lot. It removes the bladder and nearby tissues. Sometimes, other organs are taken out too, based on the patient’s health and gender.
Radical cystectomy is a big surgery because it takes out the bladder and lymph nodes. In men, it might also remove the prostate and seminal vesicles. Women might lose the uterus, ovaries, and part of the vagina. This makes it a major operation.
The surgery is complex and can change how patients urinate and have sex. Knowing why it’s needed is key for those facing this choice.
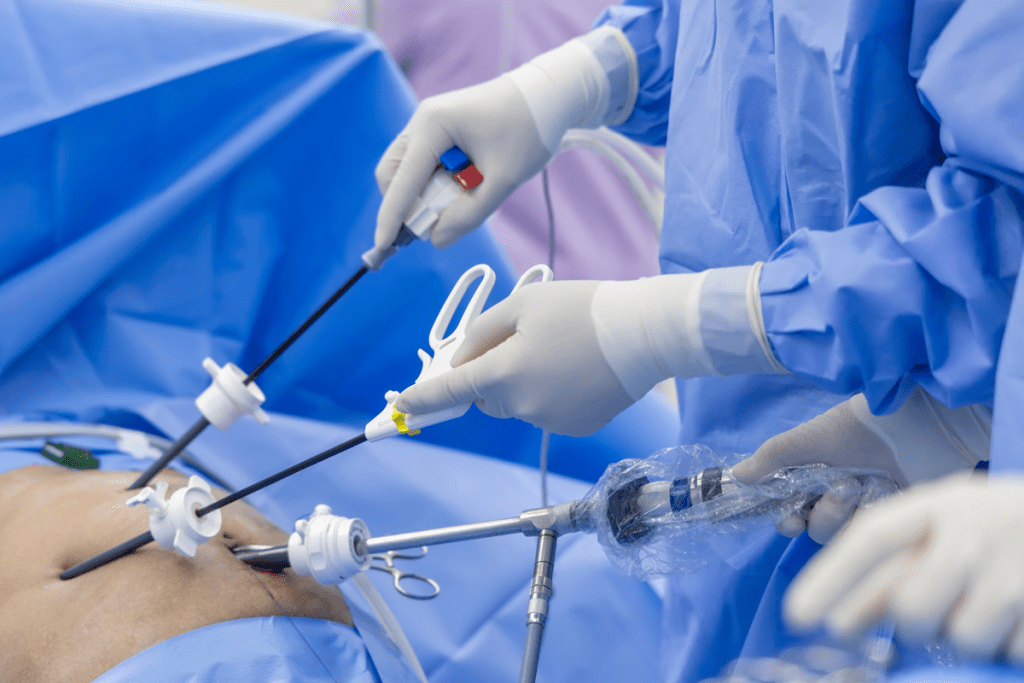
There are two main ways to do a radical cystectomy: open surgery and robotic-assisted surgery. Open surgery uses a big cut in the belly to reach the bladder. It’s old-school but can be more invasive.
Robotic-assisted surgery uses small cuts and a robotic system. It’s less invasive and might lead to less blood loss and quicker healing. But the best choice depends on the patient’s situation.
During radical cystectomy, the bladder and other organs are removed. A urinary diversion is made so the patient can urinate after the bladder is removed. The type of diversion depends on the patient’s health, the reason, and their wishes.
Knowing what happens during and after surgery helps patients get ready for the changes radical cystectomy brings.
When the bladder is removed, a new way for urine to leave the body is needed. This is called urinary diversion. It helps patients manage their urine effectively after surgery. We will look at the different ways to divert urine and how they affect daily life.
Ileal conduit is a common method. It uses a part of the intestine as a tube for urine. The ureters are attached to the intestine, then brought to the abdomen. A stoma is created, and urine goes into a bag on the skin.
Key aspects of ileal conduit urinary diversion include:
Neobladder makes a new bladder from the intestine. It’s connected to the urethra. This way, patients can urinate naturally.
Benefits of neobladder reconstruction include:
A continent urinary reservoir is made from the intestine. It stores urine. Patients use a stoma to empty it.
Advantages of a continent urinary reservoir:
Each method affects daily life differently. Lifestyle, personal preferences, and health are important. They help decide which method is best.
Ileal conduit means regular bag changes and stoma care. Neobladder requires learning to urinate naturally and managing incontinence. Continent reservoirs need regular catheter use.
Patients need to understand these differences. We help patients choose the best method for them. We consider their needs and preferences.
Knowing about the hospital stay and recovery after bladder removal is key. This time is important for a good outcome later on.
Patients usually stay in the hospital for 5 to 9 days after bladder removal surgery. Doctors keep a close eye on them, managing pain and looking for any problems. Good care after surgery helps avoid infections and makes sure the patient is ready to go home.
Patients need a lot of care after bladder removal surgery. They are watched for any issues, their pain is managed, and they get the nutrients they need to heal. They also learn how to take care of their new urinary system to avoid infections.
Managing pain is a big part of care after surgery. Patients get medicine to help with pain, and the doctor adjusts it as needed. Doctors also watch for early signs of problems like infections or bleeding. Catching these early helps avoid bigger problems.
Many hospitals use special recovery plans for bladder removal patients. These plans, called ERAS, aim to reduce stress from surgery, improve nutrition, and lower the risk of complications. ERAS includes steps like pre-surgery advice, nutrition support, and early movement to help patients recover faster.
Recovering fully after bladder removal surgery is key for patients to regain strength and adjust to their new life. This journey includes physical healing, mental adjustment, and changes in lifestyle.
Recovery from bladder removal surgery can take 3 to 6 months. During this time, patients are watched closely by their healthcare team. This ensures they heal well and handle any issues that come up.
Key milestones in the recovery timeline include:
Physical therapy is essential after bladder removal surgery. Patients start with light exercises and slowly increase them as advised by their healthcare provider.
Activity restrictions typically include:
Adjusting mentally to the changes from bladder removal surgery is as important as physical recovery. Patients must accept changes in their urinary function and other bodily changes.
Seeking support from healthcare professionals, support groups, or counseling is recommended. This helps patients cope with these changes.
Getting back to normal activities is a big step in recovery. Patients should follow their healthcare provider’s advice on when to start driving, return to work, and resume physical activities.
Tips for a smooth return to normal activities include:
Understanding the long-term recovery process and making necessary adjustments can improve life after bladder removal surgery. We are dedicated to supporting our patients through every step of their recovery journey.
It’s important for patients to know about the risks and long-term effects of bladder removal surgery. This surgery, known as cystectomy, has its own set of complications. Patients should be aware of these to make informed decisions.
Over 60% of patients face complications within 90 days after surgery. These can include infections, bleeding, and issues with the urinary system. We keep a close eye on patients to quickly address any problems.
Readmission rates after cystectomy are between 27 and 30%. Knowing what leads to readmission helps us improve care. We aim to support patients so they can manage their recovery well.
Bladder removal surgery can affect a patient’s quality of life and sexual function. While we try to preserve sexual function, the impact varies. We offer support to help patients adjust to these changes.
The survival rate after bladder removal surgery depends on the reason for the surgery, like bladder cancer. For bladder cancer patients, the five-year survival rate is about 66%. We help patients understand their prognosis and plan follow-up care.
Knowing the risks and long-term effects of bladder removal surgery helps patients make better choices. We’re dedicated to supporting and guiding patients through their recovery.
Bladder removal surgery, or cystectomy, is a big change. But, with the right care, people can live well without a bladder. We’ve talked about the surgery, why it’s done, and how to manage without a bladder.
Choosing how to manage urine after surgery is key. Options include ileal conduit, neobladder, and continent reservoir. Each has its own pros and cons. The best choice depends on the patient’s needs.
Adjusting to life without a bladder takes time. But many people find ways to live happily. With the right support, managing urine and avoiding problems is possible. We stress the need for full care and guidance to help patients thrive after surgery.
A cystectomy is a surgery to remove the bladder. It’s done to treat bladder cancer or severe bladder issues. We choose this surgery when other treatments don’t work.
After removing the bladder, there are several ways to manage urine. These include ileal conduit, neobladder reconstruction, and continent urinary reservoir. Each has its own benefits and drawbacks. We’ll help you choose the best one for you.
Recovery time varies, but most patients stay in the hospital for 5-9 days. It can take 3 to 6 months to fully recover. We’ll keep an eye on your progress and offer support.
Cystectomy carries risks, like infection or bleeding, which happen in over 60% of patients within 90 days. Long-term, it can affect your quality of life and sexual function.
Yes, it’s possible to adapt to life without a bladder with the right urinary diversion and support. Many patients lead fulfilling lives after recovery.
Surgery can impact your quality of life and sexual function. We’ll discuss these effects with you and help you manage them for the best outcome.
Survival rates vary based on cancer stage at diagnosis. Generally, the five-year survival rate is about 66%. We’ll give you personalized information based on your condition.
An ileal conduit uses a part of the intestine to create a urine conduit. It’s chosen for its simplicity and effectiveness.
Neobladder reconstruction creates a new bladder from the intestine. It allows for more natural urination. But it requires careful consideration and patient selection.
A continent urinary reservoir is made from intestinal tissue to store urine. It allows for catheterization to empty the pouch, making it convenient and continent.
Caffeine stays in your system for 4 to 6 hours after drinking. It’s important to follow your healthcare provider’s dietary advice after surgery.
The bladder is in the pelvis, behind the pubic bone. It’s centered in the body, not on one side.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!