Last Updated on December 2, 2025 by Bilal Hasdemir

dbs
Parkinson’s disease affects millions worldwide, causing motor symptoms that significantly impact quality of life. Deep Brain Stimulation (DBS) has emerged as a surgical therapy to treat certain aspects of Parkinson’s disease. It is especially helpful for those experiencing disabling tremors, wearing-off spells, and medication-induced dyskinesias.
We explore how DBS surgery can potentially slow Parkinson’s progression, improving the lives of those affected. By understanding the role of Deep Brain Stimulation in managing Parkinson’s disease, we can better appreciate its benefits and limitations.
Key Takeaways
- Deep Brain Stimulation is a surgical therapy used to treat certain Parkinson’s disease symptoms.
- DBS is most effective for patients with disabling tremors and medication-induced dyskinesias.
- The potential of DBS to slow Parkinson’s disease progression is a significant area of research.
- Understanding DBS benefits and limitations is crucial for managing Parkinson’s disease.
- DBS surgery can improve the quality of life for Parkinson’s patients.
Understanding Parkinson’s Disease and Its Progression
Detailed visual representation of Parkinson’s disease progression stages. In the foreground, a series of portraits capturing the gradual changes in facial expressions and motor skills as the condition advances. The middle ground features a clinical diagram illustrating the affected brain regions and neurological mechanisms. The background showcases a subtle, hazy medical environment with diagnostic equipment and blurred silhouettes, conveying a sense of the scientific and clinical context. The lighting is soft and muted, emphasizing the seriousness and gravity of the subject matter. The overall composition should convey a balanced, informative, and visually engaging depiction of Parkinson’s disease progression.
Parkinson’s disease is a chronic and progressive neurological disorder. It poses significant challenges for patients and healthcare providers. We will explore its underlying mechanisms, progression, and monitoring in clinical settings.
The Pathophysiology of Parkinson’s Disease
Parkinson’s disease mainly affects dopamine-producing neurons in the brain. This part of the brain controls movement. The loss of these neurons leads to a lack of dopamine, causing tremors, stiffness, and bradykinesia (slowness of movement).
Natural Course and Stages of Parkinson’s Disease
The progression of Parkinson’s disease varies among individuals. It is categorized into several stages, like the Hoehn and Yahr scale. This scale ranges from Stage 1 (unilateral involvement) to Stage 5 (bed or wheelchair confinement). Understanding these stages helps in managing expectations and tailoring treatment plans.
Measuring Disease Progression in Clinical Settings
In clinical settings, disease progression is measured using various tools. The Unified Parkinson’s Disease Rating Scale (UPDRS) and assessments of motor and non-motor symptoms are used. These tools help monitor treatment effectiveness and make necessary adjustments.
Here’s a simplified overview of the Hoehn and Yahr stages:
Stage | Description |
1 | Unilateral involvement, typically with minimal or no functional impairment. |
2 | Bilateral involvement without impairment of balance. |
3 | Bilateral disease with some postural instability but physically independent. |
4 | Severe disability, but still able to stand or walk unassisted. |
5 | Confinement to bed or wheelchair unless aided. |
What is DBS? A Comprehensive Overview
A highly detailed medical illustration of deep brain stimulation, showcasing the surgical procedure and the implanted device. The foreground should depict the human brain with precision, revealing the placement of the electrodes within the specific target regions. The middle ground should feature the implantable pulse generator, connected to the brain leads by a thin, flexible cable. The background should provide a clean, clinical setting, with a sense of depth and scale to emphasize the complexity of the procedure. The lighting should be soft and directional, creating depth and highlighting the key anatomical structures. The overall mood should convey a sense of medical innovation, precision, and the potential therapeutic benefits of this neurosurgical intervention.
Deep Brain Stimulation (DBS) is a groundbreaking neurosurgical procedure. It has changed how we treat neurological conditions like Parkinson’s disease. This technology can greatly improve the lives of those with advanced Parkinson’s.
Definition and Basic Mechanism of Deep Brain Stimulation
DBS involves putting electrodes in the brain. These electrodes send electrical impulses to control abnormal brain activity. This helps reduce symptoms like tremors and stiffness.
The DBS system has three main parts: the lead, the extension, and the pulse generator. The lead goes in the brain, the extension connects it to the pulse generator, and the pulse generator is a battery under the skin.
History and Development of DBS Technology
The idea of DBS started decades ago, with early trials in the 1950s and 1960s. But it wasn’t until the 1980s that it became a common treatment for movement disorders. Thanks to technology and brain research, DBS has gotten much better over time.
- Early DBS systems were simple but caused many side effects.
- Today’s DBS technology is more precise and adjustable.
- Improvements in imaging and surgery have made DBS safer and more effective.
Components of a Modern DBS System
A modern DBS system has several important parts. Each plays a key role in delivering effective treatment. These include:
- The Lead: This is implanted in the brain and sends electrical impulses.
- The Extension: This wire connects the lead to the pulse generator.
- The Pulse Generator: This is the power source, usually under the skin near the collarbone.
Knowing how these parts work together helps us understand the complexity of modern DBS technology.
How DBS Works for Parkinson’s Patients
A high-resolution, scientifically accurate 3D rendering of the target brain regions involved in deep brain stimulation (DBS) for Parkinson’s disease. The image should showcase the key anatomical structures, including the subthalamic nucleus, globus pallidus, and substantia nigra, in a clear and detailed manner. The scene should be illuminated by a soft, even light that accentuates the intricate neural pathways and highlights the precise locations of the DBS electrodes within the brain. The composition should be centered and focused, with a clean, clinical background that emphasizes the medical and scientific nature of the image. The overall atmosphere should convey a sense of precision, clarity, and scientific understanding of how DBS modulates neural activity to alleviate the symptoms of Parkinson’s disease.
DBS is a complex treatment that targets specific brain areas to help Parkinson’s symptoms. It changes abnormal brain activity. This can greatly improve motor function and quality of life for patients.
Target Brain Regions in Parkinson’s Treatment
In treating Parkinson’s, DBS focuses on three key brain areas: the subthalamic nucleus (STN), the globus pallidus internus (GPi), and the ventral intermediate nucleus of the thalamus (Vim). These areas are vital for controlling movement. Stimulation here can lessen Parkinson’s symptoms.
The right area to target depends on the patient’s symptoms and medical history. For example, STN DBS is often used to reduce medication needs. GPi DBS is better for managing dyskinesia.
Electrical Stimulation Effects on Neural Circuits
DBS sends electrical impulses to certain neural circuits. This changes their activity. It helps normalize the brain’s activity patterns in Parkinson’s disease.
The stimulation impacts the cortico-basal ganglia-thalamo-cortical loop, key for motor control. This can help with symptoms like tremors, rigidity, and slow movement.
Neurophysiological Changes After DBS Implementation
After DBS is set up, the brain undergoes several changes. These include new activity patterns, changes in neurotransmitter release, and possible neuroprotective effects.
Research shows DBS can reduce abnormal brain activity seen in Parkinson’s. It may also help the brain adapt and manage symptoms over time.
It’s important to understand these changes to make DBS therapy better. Ongoing research aims to improve Parkinson’s treatment with DBS.
The Primary Question: Can DBS Halt Disease Progression?
A detailed, high-resolution medical illustration showcasing the progression of Parkinson’s disease and the potential impact of Deep Brain Stimulation (DBS) treatment. The foreground depicts the human brain, with a clear visualization of the affected neural pathways and the gradual deterioration of dopaminergic neurons over time. The middle ground features a series of illustrative diagrams highlighting the surgical implantation of DBS electrodes and the electrical stimulation of targeted brain regions. The background provides a clinical, scientific atmosphere, with medical imagery, diagnostic scans, and subtle textural elements that convey the seriousness of the condition and the complexity of the treatment. Realistic lighting and photographic quality create a sense of depth and authenticity, allowing the viewer to fully comprehend the primary question of whether DBS can halt the progression of Parkinson’s disease.
Deep Brain Stimulation (DBS) is known to manage Parkinson’s disease symptoms well. But can it stop the disease from getting worse? It’s important to understand the difference between managing symptoms and changing the disease itself.
Current Scientific Evidence and Research Findings
Studies have looked into how DBS affects Parkinson’s disease progression. DBS greatly improves symptoms and quality of life. However, its effect on slowing down the disease is still debated.
Distinguishing Symptom Management from Disease Modification
It’s key to know the difference between managing symptoms and changing the disease. Symptom management helps with symptoms like tremors and rigidity. But it doesn’t change the disease itself. Disease modification means the treatment could slow or stop the disease’s progression.
DBS is great at managing symptoms. But its role in changing the disease is still being looked into. “Understanding the difference between symptom management and disease modification is crucial for knowing DBS’s true impact on Parkinson’s disease,” says Medical Expert, a leading researcher.
The DBS Surgical Procedure Explained
A detailed surgical scene of a deep brain stimulation (DBS) procedure. In the bright, sterile operating theater, a team of skilled neurosurgeons carefully navigate the patient’s skull, exposing the brain’s intricate structures. Precise incisions and the delicate placement of electrodes are captured with a high-resolution camera, revealing the technical complexity of this life-changing intervention. The scene conveys the gravity and importance of this procedure, which aims to alleviate the debilitating symptoms of Parkinson’s disease.
The journey to DBS implantation starts with a detailed pre-surgical evaluation. This first step is key to see if a patient is right for DBS therapy.
Pre-surgical Evaluation and Planning
Before DBS surgery, patients go through a detailed evaluation. This includes:
- Neurological checks to see how bad Parkinson’s symptoms are
- Imaging like MRI to find the best spot for the electrodes
- Psychological tests to check mental health and thinking skills
This team effort makes sure DBS surgery fits each patient’s needs perfectly.
Step-by-Step Surgery Process
The surgical procedure for DBS has several important steps:
- Putting electrodes in the brain’s target spots
- Putting a pulse generator under the skin, usually in the chest
- Connecting the electrodes to the pulse generator with an extension wire
Patients are usually under local anesthesia during the surgery. This lets them give feedback to the team.
Post-operative Care and Initial Recovery
After DBS surgery, patients are watched closely in the hospital for any problems. Post-operative care includes managing pain, stopping infection, and checking how well the device works.
Device Activation and Initial Programming
The last step in the DBS surgical procedure is device activation and first programming. This happens a few weeks after surgery, when swelling goes down. The healthcare team then sets the device to best control symptoms.
Knowing about the DBS surgical procedure helps patients get ready for this big step in their Parkinson’s treatment.
Ideal Candidates for DBS Treatment
Detailed medical diagram showcasing the key criteria for deep brain stimulation (DBS) candidacy in Parkinson’s disease. A crisp, high-resolution illustration against a clean, clinical background. The foreground features a patient profile with labeled anatomical regions and metrics such as disease severity, medication response, and cognitive function. The middle ground includes a schematic of the DBS implant components and surgical placement. The background contextualizes the treatment with informative icons and infographic elements. Conveys an authoritative, educational tone suitable for a medical publication.
Finding the right candidates for Deep Brain Stimulation (DBS) is key to its success in treating Parkinson’s disease. DBS has changed how we manage advanced Parkinson’s, offering relief from symptoms and improving life quality for many.
Medical Criteria for DBS Candidacy
The criteria for DBS are complex, looking at the patient’s Parkinson’s disease, medical history, and health. Those with advanced Parkinson’s and severe motor symptoms despite medication are often considered. Factors like tremor, rigidity, and bradykinesia are also important.
“DBS is not a cure for Parkinson’s disease, but it can significantly improve motor symptoms and reduce medication-induced complications,” say leading neurologists. This highlights the need for a detailed assessment to find the right candidates.
Optimal Timing of DBS in Disease Course
The best time for DBS implantation is a topic of ongoing debate. Traditionally, it was seen as a late-stage treatment. But recent studies suggest early intervention might lead to better results. Now, we consider DBS for patients with 4-10 years of Parkinson’s and significant motor issues. The decision depends on the disease’s progression, medication response, and comorbidities.
Contraindications and Exclusion Factors
Some conditions make a patient unsuitable for DBS. These include significant cognitive issues, severe depression or psychosis, and certain medical conditions. Those with implanted devices or frequent MRI needs are also excluded. A detailed pre-surgical check is essential to identify these issues.
The Screening and Selection Process
The process for selecting DBS candidates involves a team of healthcare experts. This includes neurologists, neurosurgeons, psychiatrists, and sometimes psychologists. The evaluation covers medical history, neurological exams, neuropsychological tests, and imaging studies. The goal is to ensure the procedure will significantly improve symptoms and quality of life.
As we learn more about DBS, the criteria for candidacy may change. Ongoing research and clinical experience will help refine the selection and timing for DBS in Parkinson’s disease management.
Proven Benefits of DBS for Parkinson’s Symptoms
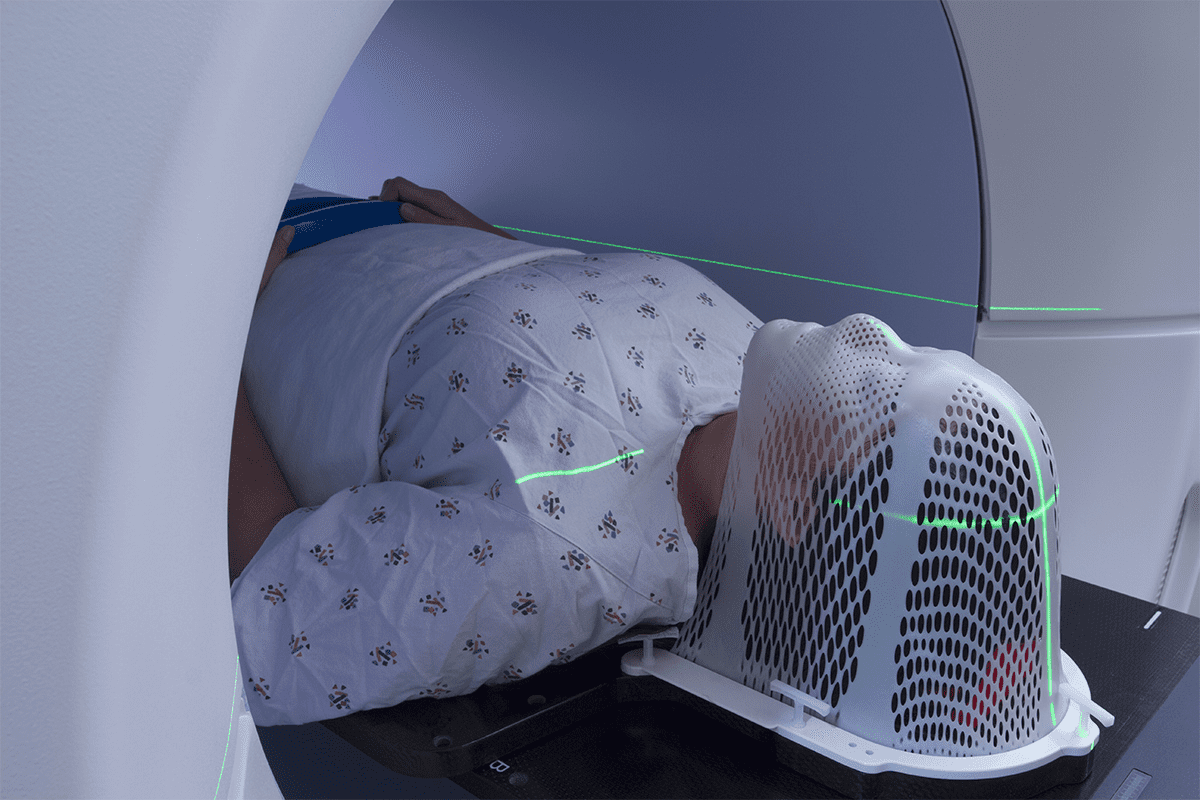
Detailed, high-resolution photograph of a person with Parkinson’s disease undergoing deep brain stimulation (DBS) treatment to alleviate motor symptoms. The foreground features the patient’s head with surgical implants visible, surrounded by medical equipment and tools used during the procedure. The middle ground showcases a team of neurosurgeons and specialists carefully monitoring the patient’s vital signs and brain activity on various display screens. The background depicts a modern, well-lit operating room with clean, sterile surfaces and advanced medical technology. The overall scene conveys a sense of precision, expertise, and the potential benefits of DBS for improving Parkinson’s motor symptoms.
DBS is a promising treatment for Parkinson’s disease. It helps reduce motor symptoms and improves patient outcomes. The benefits of DBS for Parkinson’s patients are many, improving both symptoms and quality of life.
Motor Symptom Improvements
DBS is great at improving motor symptoms of Parkinson’s disease. Studies show it can lessen tremors, rigidity, and slow movements. This allows patients to move more easily.
DBS targets specific brain areas. It helps control motor fluctuations in advanced Parkinson’s disease.
Impact on Medication Requirements and Management
DBS also helps with medication management. By reducing symptoms, DBS can lower the need for dopamine medications. This can reduce side effects like dyskinesias.
Quality of Life Enhancements
Improvements in symptoms and medication needs boost quality of life. Patients feel more independent and can do daily tasks more easily. They also experience fewer motor fluctuations and dyskinesias.
Long-term Effectiveness Data
Long-term studies show DBS’s lasting benefits for Parkinson’s symptoms. Research indicates that DBS’s effects can last for years. This makes it a reliable treatment option.
Advances in DBS technology and programming are continually improving outcomes.
Limitations of DBS as a Parkinson’s Treatment
DBS has changed how we treat Parkinson’s disease. Yet, it has its limits. Knowing these helps us set the right expectations for patients.
Symptoms Unresponsive to DBS Therapy
DBS works well for motor symptoms like tremors and stiffness. But, it doesn’t help with everything. For example:
- Postural instability and gait disturbances
- Speech difficulties, such as dysarthria
- Non-motor symptoms like constipation, urinary issues, and sleep disturbances
It’s important to know these limits when thinking about DBS.
Cognitive and Psychiatric Considerations
DBS affects different people in different ways. Some see improvements, while others may not. Or, in some cases, symptoms can get worse.
Cognitive considerations include:
- Memory issues
- Executive function challenges
- Potential for cognitive decline
Psychiatric considerations may involve:
- Mood disorders, such as depression or anxiety
- Impulse control disorders
- Psychosis or hallucinations
Choosing the right patients and watching them closely is key.
The Disease Progression Question Revisited
Many wonder if DBS can stop or slow Parkinson’s disease. So far, it seems DBS manages symptoms well but doesn’t change the disease’s course.
Managing Expectations for Patients and Families
It’s vital to manage what patients and families expect from DBS. They need to know both the good and the bad. This includes:
- Realistic outcome expectations
- Understanding the need for ongoing programming and adjustments
- Awareness of potential side effects and complications
Good education and support help patients make the best choices for their treatment.
Potential Risks and Side Effects of DBS
DBS offers big benefits for Parkinson’s patients. But, it’s important to know the risks and side effects. Like any surgery, DBS can have complications that patients and doctors need to think about.
Surgical Complications and Risks
DBS surgery can have some complications. These might include:
- Infection at the site of the device implantation
- Bleeding or hemorrhage in the brain
- Stroke or cerebral edema
- Seizures
- Headaches or discomfort
Even though these risks are serious, they don’t happen often. Most people have DBS surgery without big problems.
Hardware-Related Issues and Failures
The DBS system has parts like the lead, extension, and pulse generator. Problems with these parts can happen, such as:
- Lead fracture or migration
- Extension wire damage
- Pulse generator malfunction or battery depletion
- Skin erosion over the implanted hardware
These problems might need more surgeries to fix or replace the parts.
Stimulation-Related Side Effects
The DBS system sends electrical impulses. This can cause side effects like:
- Dyskinesias or involuntary movements
- Speech disturbances, such as dysarthria or stuttering
- Mood changes, including depression or hypomania
- Cognitive changes, such as confusion or memory issues
- Balance problems or gait disturbances
Many of these side effects can be managed by changing the stimulation settings.
Long-term Safety Considerations
DBS safety over time is still being studied. Research shows DBS can be safe and effective for Parkinson’s disease for a long time. But, there are long-term risks and things to consider, like:
Long-term Consideration | Description |
Battery Replacement | The pulse generator battery may need to be replaced every 3-5 years, requiring additional surgery. |
Hardware Evolution | Advances in DBS technology may necessitate hardware upgrades or replacements. |
Tolerance or Habituation | Some patients may experience a decrease in the effectiveness of DBS over time. |
Imaging and MRI Compatibility | Patients with DBS may face limitations when undergoing MRI scans. |
It’s key for patients thinking about DBS for Parkinson’s disease to know these risks and side effects. Talking about these with a healthcare provider is important for making a good decision.
DBS Cost and Insurance Coverage in the United States
The cost of DBS surgery and devices is high. This makes insurance coverage very important. We need to know what affects the total cost of DBS treatment.
Insurance Coverage Landscape
Most private insurance in the U.S. covers DBS for Parkinson’s disease. But, how much they cover can differ a lot. Some insurers need prior approval or have special rules for coverage. It’s key for patients to talk with their healthcare team and insurance about what’s covered.
Medicare and Medicaid Considerations
Medicare usually covers DBS surgery if it’s medically needed. But, there might be rules for the device and programming. Medicaid coverage changes by state, so patients should check their state’s rules. Knowing these details helps manage costs.
Financial Assistance Options
There are ways to help pay for DBS treatment. Device makers, non-profits, and Medicaid or state programs offer help. Patients should look into these options to reduce costs.
In summary, while DBS treatment is expensive, knowing about insurance and financial help can make it more affordable. This way, more people can get the treatment they need.
Living with DBS: Patient Experiences and Adjustments
DBS therapy changes a lot for Parkinson’s patients. It brings big improvements in symptoms but also new challenges. After DBS surgery, people see big changes in their life.
Daily Life with a DBS System
Life with a DBS system is different. The device sends electrical signals to the brain. This helps control Parkinson’s symptoms.
Patients find it easier to do daily tasks. But, managing the device is a big part of life now. This includes:
- Learning to use the device controller
- Keeping track of battery life and recharging
- Going to appointments for adjustments and maintenance
Programming and Maintenance Requirements
The DBS system needs regular care. This means:
- Going to appointments for adjustments
- Watching for symptom changes or side effects
- Keeping the device and parts clean
These steps are key to getting the most from DBS therapy. They help avoid side effects too.
Activity Restrictions and Precautions
DBS therapy improves life a lot. But, there are things to avoid. For example:
- Staying away from strong magnetic fields, like MRI machines
- Being careful with sudden head movements or sports
- Telling doctors about the DBS system before medical procedures
Patient Testimonials and Reported Outcomes
Many patients say DBS has greatly improved their life. For example, a patient might say,
“DBS has given me my life back. I can now walk without freezing, and my tremors are almost gone.”
These stories show DBS’s benefits for some patients. While results vary, most agree DBS is a good treatment for Parkinson’s.
Living with a DBS system needs adjustments. But, with the right help, many patients live full and active lives.
Alternative and Complementary Treatments to DBS
Managing Parkinson’s disease often means using a mix of treatments. This includes DBS and other options tailored for each person. It’s key to know how these treatments work together or separately to help care for Parkinson’s.
Advanced Medication Strategies
Medicine is a big part of treating Parkinson’s. Advanced strategies aim to make medications work better and have fewer side effects. This might mean changing doses, switching to different forms, or trying new medicines.
Levodopa is a common treatment, but it can cause problems like dyskinesia over time. To avoid these issues, doctors might add dopamine agonists or MAO-B inhibitors to the treatment plan.
Other Surgical Approaches for Parkinson’s
DBS is a well-known surgery for Parkinson’s, but there are others too. Pallidotomy and thalamotomy are examples. These surgeries create specific lesions in the brain to help symptoms.
- Pallidotomy can help reduce dyskinesia and improve motor function.
- Thalamotomy is often used to treat tremors that are resistant to other treatments.
Non-invasive Brain Stimulation Options
Non-invasive brain stimulation is another way to treat Parkinson’s. Transcranial Magnetic Stimulation (TMS) and Transcranial Direct Current Stimulation (tDCS) are being studied for their benefits. They might help improve motor symptoms and slow disease progression.
These methods are still being researched. Their effectiveness can vary. Yet, they show promise for non-drug treatments.
Lifestyle and Rehabilitative Approaches
Changing your lifestyle and using rehabilitative therapies are important for Parkinson’s management. Exercise can improve mobility and balance. Physical therapy helps keep physical function up, while occupational therapy helps with daily activities.
Nutritional advice and stress management can also help. By adding these lifestyle and therapy approaches, people with Parkinson’s can live better and possibly slow symptom progression.
Latest Research on DBS and Neuroprotection
Recent studies are looking into Deep Brain Stimulation (DBS) for Parkinson’s disease. They aim to manage symptoms and slow the disease’s progression. This research is key to finding new treatments for this condition.
Ongoing Clinical Trials and Studies
Several clinical trials are studying DBS’s neuroprotective effects. They aim to understand how DBS can change Parkinson’s disease progression. Key areas include:
- The optimal target for DBS in terms of neuroprotection
- The duration of DBS therapy required to achieve disease-modifying effects
- The impact of DBS on non-motor symptoms of Parkinson’s disease
Biomarker Research Related to DBS
Biomarker research is vital in DBS studies. It helps understand how DBS may protect the brain. Identifying reliable biomarkers is crucial for advancing this field. Researchers are looking at various biomarkers to predict and monitor DBS therapy’s effectiveness.
Future Directions in DBS Research
The future of DBS research is exciting. New areas include closed-loop DBS systems and novel targets for DBS. These advancements could lead to better outcomes for patients.
As research progresses, we’ll learn more about optimizing DBS for Parkinson’s disease. The potential for DBS to impact this disease is significant. The medical community is eagerly awaiting these findings.
Advances in DBS Technology and Techniques
DBS technology is getting better, helping those with Parkinson’s disease. These new advancements are making treatments more effective. They also improve the lives of those with the condition.
Next-Generation DBS Devices
New DBS devices are smarter and more flexible. Next-generation DBS devices offer better precision and customization. They can be adjusted as needed, helping patients more.
These devices can also change their settings on their own. This is called adaptive stimulation. It helps manage symptoms more effectively.
Adaptive and Closed-Loop Stimulation Systems
Adaptive and closed-loop systems are big steps forward. They use sensors to adjust stimulation based on brain activity. This closed-loop approach makes treatment more efficient and effective.
The benefits include:
- Improved symptom control
- Reduced side effects
- Potential for reduced battery consumption
- Enhanced patient experience due to more personalized treatment
Directional and Targeted Stimulation
Directional and targeted stimulation are also key advancements. Traditional DBS sends stimulation in all directions. But, directional DBS targets specific areas, improving results and reducing side effects.
Miniaturization and Battery Improvements
DBS technology has also become smaller and batteries last longer. Smaller devices are easier to implant. Longer-lasting batteries mean fewer surgeries.
A comparison of traditional and modern DBS devices is shown in the table below:
Feature | Traditional DBS Devices | Modern DBS Devices |
Stimulation Type | Omni-directional | Directional/Targeted |
Battery Life | Typically 3-5 years | Up to 10 years or more |
Device Size | Larger and more invasive | Smaller and less invasive |
These advancements in DBS technology are making treatments better for Parkinson’s disease patients. As research goes on, we’ll see even more new developments.
When to Consider DBS in Your Parkinson’s Treatment Journey
For many Parkinson’s patients, deciding when to consider DBS is a big question. Deep Brain Stimulation (DBS) is a treatment option for managing symptoms. It’s especially helpful for those with medication issues or side effects.
Timing Considerations and Warning Signs
Knowing when to consider DBS means looking for warning signs. If your motor symptoms like tremors or rigidity get worse, it might be time. Also, if your medications cause side effects like dyskinesia, DBS could be an option.
Talking to your neurologist about your symptoms and treatment history is key. They can decide if DBS is right for you based on your current treatment.
Key Discussion Points for Your Neurologist
When talking to your neurologist about DBS, there are important points to cover. Discuss your symptoms, previous treatments, and disease progression. Also, ask about the benefits and risks of DBS and what to expect during the evaluation.
- Your current medication regimen and any fluctuations in effectiveness
- The impact of Parkinson’s on your daily life and activities
- Any previous surgical interventions or other treatments you’ve undergone
- Your overall health status and any comorbid conditions
Getting a Second Opinion
Getting a second opinion is a smart move when considering DBS. It can give you more insights and confirm if DBS is right for you. It can also introduce new treatment options.
Preparing for the Evaluation Process
Preparing for the DBS evaluation involves several steps. You’ll need a thorough neurological evaluation to assess your symptoms and health. This may include tests like MRI, neuropsychological assessments, and a review of your medical history.
It’s good to come prepared with questions for your healthcare team. Ask about the DBS procedure, post-surgery support, and how it will affect your daily life.
Understanding when to consider DBS and preparing for the evaluation can help you make an informed decision. Working closely with your healthcare team and seeking second opinions can guide you through this important choice.
Conclusion: The Role of DBS in Managing Parkinson’s Disease
Deep Brain Stimulation (DBS) is a key treatment for Parkinson’s disease symptoms. It doesn’t cure the disease, but it greatly improves life quality for those with advanced Parkinson’s.
We’ve looked into Parkinson’s disease and how DBS helps manage it. DBS involves surgery to implant a device that sends electrical impulses to the brain. This helps reduce motor symptoms.
DBS offers many benefits, like better motor function and less need for medication. It also improves overall well-being. But, it’s important to know its limits, like not stopping the disease from getting worse and possible side effects.
In summary, DBS is a vital part of managing Parkinson’s disease. It brings many benefits to patients with advanced disease. As research grows, we’ll see better DBS technology and techniques, leading to even better results for patients.
FAQ
What is Deep Brain Stimulation (DBS) and how does it work?
DBS is a surgery that implants electrodes in the brain. These electrodes send electrical impulses. They help control abnormal brain activity, easing symptoms of Parkinson’s and other conditions.
Can DBS stop or slow down Parkinson’s disease progression?
DBS can greatly improve symptoms and life quality for many Parkinson’s patients. But, it’s not proven to stop or reverse the disease’s progression. More research is needed.
What are the primary benefits of DBS for Parkinson’s patients?
DBS can greatly reduce symptoms like tremors and rigidity. It also lowers the need for medication, improving life quality for many.
Who is a good candidate for DBS treatment?
The best candidates have advanced Parkinson’s with big motor issues. They should have tried all medications. The choice depends on health, disease level, and personal wishes.
What are the potential risks and side effects of DBS?
Surgery risks include infection and stroke. There are also side effects like tingling and changes in mood or thinking. Long-term, you might need battery replacements.
How much does DBS surgery cost, and is it covered by insurance?
DBS surgery costs vary by location and doctor. In the U.S., insurance often covers it, including Medicare and Medicaid. But, coverage can differ.
What is the recovery process like after DBS surgery?
After surgery, you’ll stay in the hospital for a bit. Then, you recover at home. Adjustments to the device settings might be needed later.
Are there alternative treatments to DBS for managing Parkinson’s disease?
Yes, other treatments include new medications and surgeries. There are also non-invasive methods and lifestyle changes like physical therapy.
What advancements are being made in DBS technology?
New DBS devices have better batteries and smarter systems. They also offer more precise and targeted treatments. The devices are getting smaller too.
How do I know if DBS is right for me, and when should I consider it?
Talk to a neurologist or movement specialist about DBS. Consider your symptoms, medication response, health, and personal wishes. Look for signs like worsening motor issues and decreased quality of life.
References
National Center for Biotechnology Information. Deep Brain Stimulation in Parkinson’s Disease. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3002606/