Last Updated on December 2, 2025 by Bilal Hasdemir
dbs surgery
Parkinson’s disease affects over 1 million people in the United States. Many turn to deep brain stimulation surgery as a treatment.
Dealing with neurological disorders treatment can be scary. It’s key to know what to expect from such a big medical step.
The time it takes for DBS surgery can change. But knowing what’s coming is important for those thinking about it.
Key Takeaways
- DBS surgery is a complex procedure for treating Parkinson’s disease and other neurological disorders.
- The surgery involves implanting electrodes in the brain.
- Understanding the duration and recovery process is vital for patients.
- DBS surgery offers significant benefits for patients with advanced Parkinson’s disease.
- Careful planning and consideration are required before undergoing DBS surgery.
What is Deep Brain Stimulation (DBS) Surgery?

A detailed cross-sectional view of a human brain, showcasing the intricate neural circuitry and the precise placement of electrodes for deep brain stimulation. Rendered in a high-resolution, photorealistic style, the image should depict the procedure with clinical accuracy, highlighting the surgical approach, the implanted device, and the targeted areas of the brain responsible for the patient’s condition. The lighting should be soft and directional, creating a sense of depth and emphasizing the delicate structures within the brain. The overall composition should convey a sense of medical professionalism and scientific inquiry, suitable for illustrating a technical article on the subject of DBS surgery.
Deep Brain Stimulation (DBS) surgery is a new way to treat brain diseases. It involves putting electrodes in the brain to send electrical signals. These signals help control brain activity that’s not normal.
The Science Behind DBS Therapy
DBS works by changing how the brain acts. It targets certain brain spots to help manage symptoms of diseases. For example, it can help with Parkinson’s disease by sending signals to the brain.
- Delivering electrical impulses to specific brain regions
- Regulating abnormal brain activity
- Improving symptom management for conditions like dystonia and essential tremor
Experts say DBS is a key treatment for serious brain diseases. This shows how important DBS is in today’s neurology.
“DBS has the potential to significantly improve the quality of life for patients with neurological conditions that are resistant to other treatments.”
— Neurological Expert
Common Conditions Treated with DBS
DBS is good for treating many brain diseases, including:
- Parkinson’s disease: Characterized by tremors, stiffness, and movement difficulties
- Dystonia: Involves involuntary muscle contractions and spasms
- Essential tremor: Marked by persistent tremors, especially during voluntary movements
These diseases cause abnormal brain activity. DBS can change this activity. This can greatly improve symptoms and life quality for patients.
The Complete DBS Surgery Timeline

A detailed, chronological timeline depicting the key stages of a deep brain stimulation (DBS) surgery, presented as a realistic medical illustration. The foreground showcases a surgeon’s hands performing various surgical procedures, with clear visualization of the different tools and equipment used. The middle ground features a cross-section of the human brain, highlighting the targeted region for the DBS implantation. The background sets a calm, sterile hospital environment with muted colors and subtle lighting, emphasizing the precision and care required during the operation. The overall composition conveys the intricate, step-by-step nature of a DBS surgery, allowing the viewer to follow the timeline from start to finish.
Knowing the DBS surgery timeline is key for patients. It helps them prepare for the procedure and recovery. The process includes pre-surgical evaluation, surgery, and post-operative care. We’ll outline the timeline’s main parts to help patients understand what’s ahead.
Pre-surgical Evaluation Period
The pre-surgical evaluation is a crucial step. It checks if a patient is right for DBS surgery. This phase includes tests and talks with doctors like neurologists and psychologists. It can take weeks to months, based on the patient’s health and the case’s complexity.
Key components of the pre-surgical evaluation include:
- Medical history review
- Neurological examinations
- Imaging studies (MRI, CT scans)
- Psychological assessments
- Discussion of treatment goals and expectations
Actual Surgical Duration Expectations
The surgery’s length varies. It depends on the case’s complexity and if the patient is awake or asleep. Generally, it takes 3 to 6 hours per hemisphere. For bilateral stimulation, it might take longer.
Factors influencing surgical duration include:
- The number of brain hemispheres being treated
- The surgical team’s experience
- The specific DBS technique used
- Any unexpected challenges during the procedure
Post-operative Hospital Stay
After surgery, patients stay in the hospital for monitoring. The stay’s length varies but usually is a few days to a week. Medical staff watch over the patient, manage any issues, and start programming the DBS device.
Post-operative care includes:
- Monitoring for surgical complications
- Initial programming of the DBS device
- Pain management
- Patient education on post-operative care and follow-up appointments
Understanding the DBS surgery timeline helps patients prepare. It’s vital to follow the healthcare team’s advice and keep all follow-up appointments. This ensures the best results.
Step-by-Step DBS Surgery Procedure
a detailed medical illustration of a DBS surgery frame, with the patient’s head securely fastened in a specialized neurosurgical frame, the frame’s metallic arms and supports clearly visible, the frame’s positioning precisely aligned to the patient’s skull, the frame designed to stabilize the head and provide a stable reference point for the surgical procedure, the frame’s components meticulously rendered with a high level of technical accuracy and visual realism, the image capturing the essential step-by-step process of frame placement prior to the DBS surgery, the frame’s structure and positioning conveying a sense of the care and precision required in this delicate neurosurgical procedure
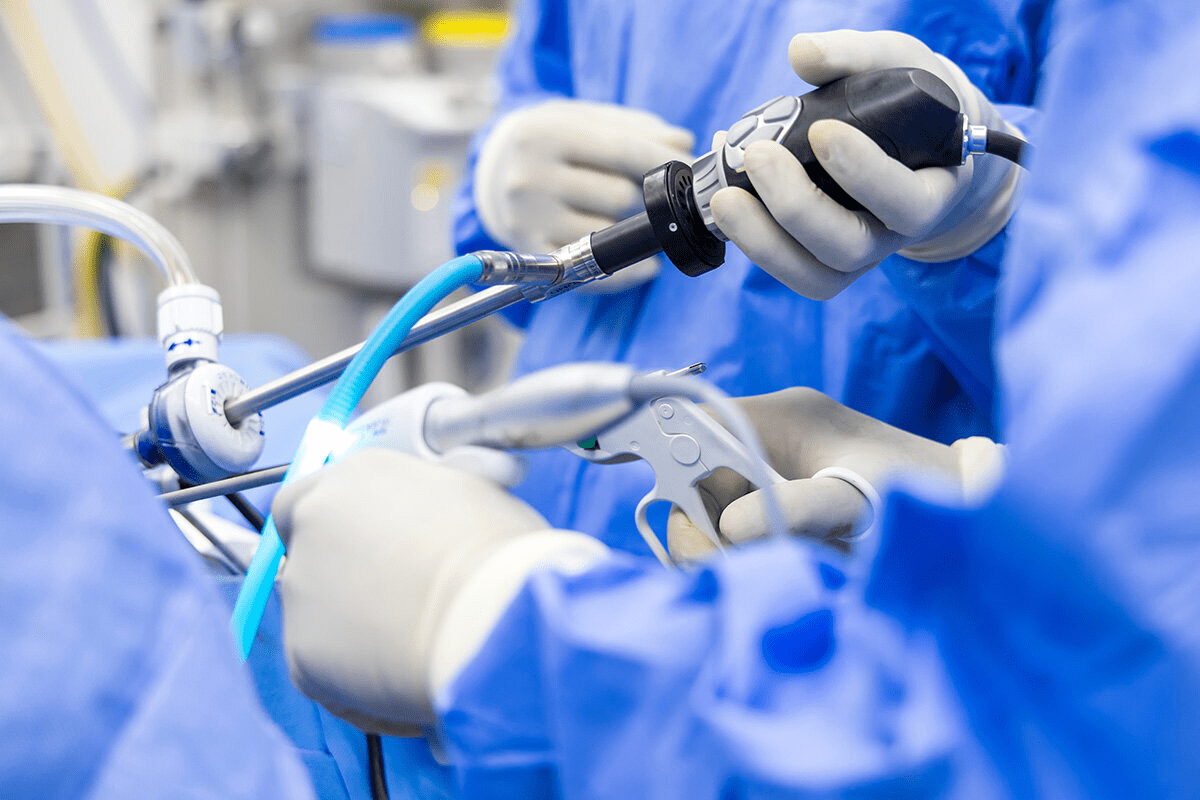
DBS surgery is a detailed process, from placing the frame to implanting the neurostimulator. Knowing these steps helps patients see the treatment’s complexity and precision.
Frame Placement and Imaging
The first step is placing a stereotactic frame on the patient’s head. This frame is key for targeting brain areas accurately. After securing the frame, the patient gets imaging tests like MRI or CT scans. These tests help the team map the brain and plan the DBS leads’ path.
Lead Implantation Process
Next, the patient is ready for the DBS leads’ implantation. A small incision is made in the scalp, and a burr hole is created in the skull. The neurosurgeon uses the frame and imaging to guide the lead to the brain area. The lead’s position is checked with microelectrode recording and intraoperative imaging.
Neurostimulator and Extension Placement
After placing the DBS lead, the neurostimulator is implanted in the chest. An extension wire is then tunneled under the skin from the head to the neurostimulator. The neurostimulator is set to send the right electrical impulses to the brain through the DBS lead.
Step | Description | Key Elements |
1. Frame Placement and Imaging | Securing a stereotactic frame and conducting imaging tests. | Stereotactic frame, MRI/CT scans |
2. Lead Implantation | Implanting the DBS lead into the targeted brain area. | DBS lead, microelectrode recording |
3. Neurostimulator Placement | Implanting the neurostimulator and connecting it to the DBS lead. | Neurostimulator, extension wire |
Understanding the DBS surgery steps helps patients prepare for the treatment. It shows the complexity of advanced therapy.
Factors Affecting How Long DBS Surgery Takes
A detailed, technical medical diagram depicting the key factors that can influence the duration of deep brain stimulation (DBS) surgery. The foreground shows a detailed cross-section of the human brain, with labeled regions highlighting areas targeted by the DBS procedure. The middle ground features medical equipment such as electrodes, surgical tools, and imaging devices used during the operation. The background depicts a sterile operating room environment, with bright overhead lighting and clinical, neutral-toned surfaces. The overall mood is one of scientific precision and medical professionalism, conveying the complex, nuanced nature of DBS surgery and the many variables that can impact its duration.
DBS surgery time varies for everyone. Different things can affect how long it takes. Knowing these factors helps manage what patients expect and improves surgery results.
Patient-Specific Considerations
Things about the patient can change how long DBS surgery lasts. This includes the patient’s health, how complex their condition is, and their body’s shape.
- Anatomical Complexity: People with special body shapes might need more time for the leads to be placed right.
- Health Status: Those with other health issues might need extra care or changes during surgery.
- Previous Surgeries: If someone has had brain surgery before, it could make the new surgery harder.
A study found that those with more complex body shapes needed about 30 minutes more for lead placement.
Patient Factor | Potential Impact on Surgery Duration |
Anatomical Complexity | More time for precise lead placement |
Comorbidities | Extra precautions or changes needed |
Previous Surgeries | Changes in body shape make surgery harder |
Surgical Approach Variations
The way the surgery is done can also change how long it takes. Different methods are used based on the patient and the team’s choice.
“The choice of surgical approach is critical in determining the efficiency and effectiveness of DBS surgery.”
- Awake vs. Asleep DBS: Awake DBS gives feedback but takes longer because the patient has to stay awake.
- Image-Guided Techniques: Using advanced images makes the surgery more precise but might take longer.
Surgical Team Experience and Facility
The skill of the surgical team and the quality of the place where surgery happens are key. They can affect how long and successful the surgery is.
“A seasoned surgical team with a well-coordinated approach can significantly streamline the DBS procedure, reducing overall surgery time.”
Expert Opinion
- Team Experience: Teams with more experience can handle complex cases better.
- Facility Quality: Top-notch facilities with the latest tech make procedures smoother and faster.
Understanding these factors helps patients get ready for DBS surgery. It also helps them know what to expect during it.
Awake vs. Asleep DBS Surgery: Time Differences
A dimly lit surgical suite, the patient’s head illuminated by a focused surgical lamp. On one side, the patient’s eyes are wide open, expression alert and attentive, surrounded by a team of focused medical professionals. On the other, the patient’s eyes are gently closed, body relaxed, as the team works with precision around the sleeping form. The contrast between the two scenes highlights the distinct approaches of awake and asleep deep brain stimulation (DBS) surgery, each with its own unique considerations and time requirements. Crisp, high-resolution medical imagery captures the nuances of these two surgical states, providing a visual representation of the section title "Awake vs. Asleep DBS Surgery: Time Differences".
DBS surgery comes in two main types: awake DBS and asleep DBS. Each has its own timeline and things to consider for patients. The choice depends on the patient’s health, the surgeon’s style, and what the surgery needs.
Traditional Awake DBS Procedure Duration
Awake DBS surgery is done with the patient awake but under local anesthesia. This way, the patient can give feedback in real-time. It’s important for placing the DBS leads correctly. The surgery can take 4 to 6 hours per lead.
Steps include putting on a frame, imaging, and implanting the lead. All these happen while the patient is awake and can give feedback.
Key aspects of awake DBS include:
- Real-time patient feedback for precise lead placement
- Local anesthesia to keep the patient comfortable and awake
- Potential for longer surgical times due to the need for patient interaction
Asleep DBS Procedure Duration
Asleep DBS surgery is done under general anesthesia. The patient is not awake during the surgery. New imaging and surgical methods allow for accurate lead placement without patient feedback. These surgeries are usually shorter, lasting 2 to 4 hours per lead.
Benefits of asleep DBS include:
- Reduced patient discomfort and anxiety
- Potential for shorter surgical times
- Reliance on advanced imaging techniques for lead placement
In conclusion, choosing between awake and asleep DBS surgery depends on many factors. These include the patient’s needs and the surgeon’s skills. Knowing the differences in time and care is key for making the right choice for DBS surgery.
One-Stage vs. Two-Stage DBS Surgery
A high-resolution, photorealistic image of a surgical suite depicting two distinct scenarios of deep brain stimulation (DBS) surgery: one-stage and two-stage procedures. The foreground showcases a surgeon performing a one-stage DBS implantation, with the patient’s head opened and the DBS device being precisely placed. In the middle ground, a two-stage DBS surgery is shown, where the surgeon is connecting the implanted DBS device to the patient’s brain through delicate wiring. The background features advanced medical equipment, such as monitoring screens and surgical lights, creating a professional, well-equipped atmosphere. The lighting is clean, bright, and directional, highlighting the intricate details of the procedures. The camera angle is slightly elevated, providing a comprehensive view of the surgical suite and the two distinct DBS techniques.
DBS surgery can be done in one or two stages. This choice depends on the patient’s health and how complex the surgery is.
Choosing between one-stage and two-stage DBS surgery depends on several factors. These include the patient’s health, the surgery’s complexity, and the surgeon’s experience. We will look at the timelines and what to consider for both options.
Single-Day Complete Procedure Timeline
A one-stage DBS surgery is done in one session. This method is good for patients who are healthy enough and can recover faster.
Key aspects of a single-day complete procedure include:
- Reduced overall anesthesia exposure
- Potential for shorter total recovery time
- Coordination among the surgical team for a streamlined process
The time needed for a one-stage DBS surgery is usually 4 to 6 hours. This depends on the surgery’s complexity and how efficient the surgical team is.
Separated Lead and Stimulator Implantation Schedule
A two-stage DBS surgery is split into two surgeries. The first is for lead implantation, and the second is for the neurostimulator and extension.
Considerations for a two-stage procedure include:
- The first surgery places the lead, done under general or local anesthesia with sedation.
- There’s a recovery period after the first surgery to watch for any side effects.
- The second surgery puts in the neurostimulator and connects the extension leads.
The time between the two surgeries varies. It can be a few days to a few weeks, based on the patient’s health and the surgeon’s preference.
DBS Surgery Recovery Timeline
A highly detailed, realistic photographic image of a DBS surgery recovery timeline. The foreground depicts a patient’s head with an incision scar, showcasing the progression of healing over time, with bandages and stitches slowly disappearing. The middle ground features medical equipment, such as electrodes and leads, illustrating the surgical procedure. The background is a sterile, clean hospital environment with subdued lighting, creating a calming and professional atmosphere. The image conveys the gradual recovery process, with a sense of medical precision and care.
The journey to recovery after DBS surgery has several stages. These include immediate care, short-term recovery, and long-term adjustment. Knowing these phases helps patients set realistic goals and improve their outcomes.
Short-Term Recovery (4-6 Weeks)
In the short-term recovery, patients might see swelling, bruising, or discomfort. These symptoms are usually mild and go away in a few weeks. It’s advised to avoid heavy lifting, bending, or strenuous activities to protect the surgical site.
As patients move through this phase, they start to feel better. The full effects of DBS therapy may take time to show. Regular check-ups with the healthcare provider are key to track healing and address any issues.
Long-Term Adjustment Period
The long-term adjustment period can last several months. During this time, patients work with their healthcare team to adjust the DBS device settings. This may involve several programming sessions to get the best results.
As the brain adjusts to the DBS therapy, patients may see big improvements in their symptoms. This can lead to a better quality of life. It’s important to stay in touch with healthcare providers to report any changes or concerns.
Key Considerations:
- Follow post-operative instructions carefully to minimize the risk of complications.
- Attend all scheduled follow-up appointments for device programming and monitoring.
- Report any unusual symptoms or concerns to your healthcare provider promptly.
By understanding the recovery timeline and working closely with their healthcare team, patients can maximize the benefits of DBS surgery. This leads to a better quality of life.
Life After DBS Surgery
Life after DBS surgery means making adjustments and following up with care. It’s important to understand the timeline for programming sessions and medication changes.
Programming Sessions Timeline
After DBS surgery, the device needs to be set up right. This is done in several sessions.
- The first session is a few weeks after surgery, when the site is healed.
- More sessions are needed, based on how well the therapy works. They can be a few days to weeks apart.
- These sessions help fine-tune the device for the best results.
Medication Adjustments Over Time
Changing medications is a big part of care after DBS surgery. As the therapy starts to work, you might need less medicine.
- Patients often see a drop in medication within a few months.
- How long it takes to find the right balance can vary. Some need more time.
- Regular check-ups with your healthcare team are key to adjusting treatment.
We stress the importance of following your treatment plan and talking openly with your healthcare team. This helps achieve the best results.
DBS Device Components and Longevity
For those thinking about DBS surgery, knowing about the device’s parts and how long it lasts is key. The DBS system is a complex device made to help with different brain conditions.
Understanding DBS Leads and Connections
The DBS device has important parts like leads, connections, and a neurostimulator. The leads are thin wires put in the brain. They connect to the neurostimulator, which is under the skin in the chest.
The connections between the leads and the neurostimulator are vital. They make sure the electrical signals from the neurostimulator reach the right brain areas.
Battery Types and Lifespan
The neurostimulator runs on a battery, which can be rechargeable or non-rechargeable. The battery type affects how long the DBS device lasts. Rechargeable batteries need daily or weekly charging and can last 10 to 15 years.
Non-rechargeable batteries last less, needing replacement every 3 to 5 years. The choice between rechargeable and non-rechargeable depends on the patient’s lifestyle and their DBS therapy needs.
Battery Replacement Procedure Duration
When the DBS neurostimulator’s battery runs out, a replacement is needed. This procedure is simpler than the first DBS surgery, as it doesn’t involve new leads.
The battery replacement surgery takes about 30 minutes to an hour per side, depending on the system type. It’s usually done under local anesthesia, so patients can go home the same day.
Knowing about the DBS device’s parts and how long they last helps patients manage their therapy long-term. This includes planning for battery replacements and adjusting device settings.
Potential Complications That May Extend DBS Surgery Time
DBS surgery is usually safe, but surgeons face several challenges during the procedure. It’s important for patients to know about these risks and benefits.
Common Intraoperative Challenges
Several challenges can make DBS surgery longer. These include:
- Difficulty in finding the right spot due to body differences or imaging issues.
- Bleeding or hemorrhage that needs quick action.
- Air embolism, a rare but serious problem.
- Issues with the hardware, like a broken lead or malfunction.
Handling these challenges well is key to a successful DBS surgery. Surgeons and their teams need the right skills and tools.
Managing Unexpected Events During Surgery
Dealing with surprises during DBS surgery needs experience, skill, and teamwork. Surgeons must be good at solving problems as they happen. This might mean changing the surgery plan, keeping an eye on the patient’s health, or fixing hardware issues.
“The key to successful DBS surgery lies not only in the technical proficiency of the surgeon but also in the ability to anticipate and manage potential complications effectively.” – Expert in Neurosurgery
Sometimes, the team might need to stop the surgery to fix a problem. Being flexible and having a good plan before surgery helps reduce risks and get the best results for the patient.
Knowing about the possible complications and how they are managed helps patients understand the complexity of DBS surgery. It shows the skill needed to do it right.
Who Is a Good Candidate for DBS Surgery?
To find out if someone is a good candidate for DBS surgery, we look at several important things. These include their medical condition, overall health, and how much they might benefit from the surgery. We check many factors to see if a patient is right for this advanced treatment.
Ideal Candidates for the Procedure
People who are the best fit for DBS surgery usually have certain traits. These include:
- Diagnosis of a condition treatable by DBS: Conditions like Parkinson’s disease, dystonia, and essential tremor are often treated with DBS.
- Failed or inadequate response to other treatments: Those who haven’t gotten better with other treatments might benefit from DBS.
- Significant impairment in quality of life: If daily life is greatly affected by their condition, DBS could be an option.
- Good overall health: Patients should be fairly healthy, aside from the condition being treated.
We check these things through a detailed assessment. This includes looking at their medical history, doing a physical exam, and sometimes extra tests.
Contraindications and Risk Factors
Even though DBS can help many, there are some things to think about. These include:
Contraindication/Risk Factor | Description |
Severe cognitive impairment | Those with big cognitive problems might not be good candidates. |
Active infection or significant medical comorbidity | Having an active infection or serious health issues can make surgery riskier. |
Unrealistic expectations | People with too high hopes for DBS surgery might not be the best fit. |
By looking at these factors carefully, we can figure out if someone is a good candidate for DBS surgery. We can see if they are likely to get good results from it.
Cost and Insurance Considerations for DBS Surgery
DBS surgery is a big investment in your health. It’s important to know the costs involved. This helps you make the right choice for your treatment.
Average Costs and Coverage
The cost of DBS surgery can change a lot. It depends on the place, the doctor’s fees, and the technology used. On average, it can cost between $30,000 and $50,000 or more for each electrode. Since it’s usually done on both sides, the total cost is even higher.
Insurance coverage is key in paying for these costs. Most insurance plans, including Medicare and Medicaid, cover DBS surgery for certain conditions. But, the coverage can differ a lot. It depends on your insurance and policy. You should check what you’ll have to pay out of pocket.
Conclusion
DBS surgery is a complex but potentially life-changing treatment for various neurological conditions. It’s important for patients to understand the procedure, its benefits, risks, and recovery process.
We’ve looked into the details of DBS surgery, from the first evaluation to recovery. This shows that DBS surgery needs careful planning and thought. It’s a significant medical step that offers new hope for those with movement disorders and other neurological conditions.
In summary, our detailed look at DBS surgery emphasizes its importance. It shows how DBS surgery can be a turning point for many patients. It marks the start of a new chapter in their treatment journey.
FAQ
What is Deep Brain Stimulation (DBS) surgery?
DBS surgery is a neurosurgical procedure. It involves implanting a device that sends electrical impulses to the brain. This helps manage symptoms of various neurological conditions.
How long does DBS surgery take?
DBS surgery can take several hours. The exact time depends on the procedure’s complexity and the surgical team’s experience.
What are the benefits of DBS surgery?
DBS surgery can greatly improve symptoms of Parkinson’s disease, dystonia, and essential tremor. It enhances the quality of life for patients.
What is the recovery process like after DBS surgery?
Recovery starts right after surgery. It includes a short-term recovery phase of about 4-6 weeks. Then, there’s a long-term adjustment period. During this time, patients may need to adjust their medication and DBS settings.
What are the potential complications of DBS surgery?
DBS surgery is generally safe but carries risks. These include infection, bleeding, and hardware-related complications. Proper care and follow-up can manage these risks.
How is the DBS device programmed?
The DBS device is programmed through sessions with a healthcare professional. They adjust the settings to control symptoms and minimize side effects.
Can DBS surgery be performed on patients with other medical conditions?
Suitability for DBS surgery depends on various factors. These include the severity of the condition and overall health. Each case is evaluated individually.
How long does the DBS battery last?
The DBS battery’s lifespan varies. It usually lasts from 3 to 5 years. After that, it may need to be replaced.
What are the costs associated with DBS surgery?
DBS surgery costs are significant. They include the procedure, hospital stay, and follow-up care. Insurance may cover some or all of these costs, depending on the provider and policy.
Is DBS surgery reversible?
DBS surgery is generally reversible. The device can be turned off or removed if needed. However, the decision to undergo DBS surgery should be made carefully, considering its benefits and risks.
How does DBS surgery differ from other treatments for neurological conditions?
DBS surgery is a unique treatment. It directly targets specific brain areas. It offers an alternative or complement to medication and other therapies for managing neurological symptoms.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/802237