Last Updated on December 2, 2025 by Bilal Hasdemir
dbs
Deep brain stimulation (DBS) surgery is a new hope for many. It treats neurological conditions like Parkinson’s disease. Over 100,000 patients worldwide have undergone this procedure, offering new hope for those with debilitating symptoms.
We dive into the details of DBS surgery. It includes its uses and the big question: is it reversible? This surgery implants a device that stimulates the brain. It might help ease symptoms of Parkinson’s and other conditions.
Key Takeaways
- DBS surgery is used to treat various neurological conditions.
- The procedure involves implanting a brain stimulation device.
- Reversibility of DBS surgery is a significant concern.
- Understanding the benefits and risks is crucial.
- DBS has been a treatment option for over a decade.
What Is Deep Brain Stimulation (DBS) Surgery

A detailed cross-section of a human brain, showcasing the complex circuitry and neural pathways. The foreground features intricate electrodes delicately implanted into the brain tissue, their thin wires carefully threaded through the skull. The middle ground reveals the intricate neuronal networks, with glowing synaptic connections pulsing with energy. In the background, a soft, muted color palette creates a sense of depth and tranquility, evoking the precision and thoughtfulness required in deep brain stimulation surgery. Crisp, high-resolution photorealistic rendering with subtle lighting and shadows to emphasize the delicate nature of the procedure.
Deep Brain Stimulation (DBS) sends electrical impulses to certain brain areas. It helps manage symptoms of some neurological conditions. This treatment has changed how we treat movement disorders and some mental health issues.
The Mechanics of DBS Technology
DBS technology has a few main parts. The leads (or electrodes) go into the brain. The extension connects these leads to the pulse generator (or neurostimulator). The pulse generator is placed under the skin near the collarbone.
The surgery happens in two parts. First, the leads are put in the brain area that needs stimulation. This is done under local or general anesthesia, depending on the patient and the surgeon. Then, the pulse generator is implanted and connected to the leads.
Common Conditions Treated with DBS
DBS is used for several neurological conditions. These include Parkinson’s disease, dystonia, and essential tremor. For Parkinson’s, DBS can lessen tremors, stiffness, and slow movements. This improves the patient’s quality of life quality.
In dystonia, DBS can reduce muscle spasms and contractions. For essential tremor, it can stop the severe shaking.
We aim to give the best care and support to those getting DBS surgery. We want to help them live better lives.
The Concept of Reversibility in Neurosurgical Procedures

A detailed close-up view of a human brain implant, showcasing the reversible nature of deep brain stimulation (DBS) surgery. The implant is visible, with its wires and components delicately laid out against a stark, clinical background. The lighting is crisp and evenly distributed, allowing for clear visualization of the intricate device. The camera angle is slightly elevated, providing a sense of depth and emphasizing the technical complexity of the DBS system. The overall mood is one of scientific precision and medical innovation, reflecting the reversibility concept in neurosurgical procedures.
When thinking about DBS surgery, knowing about reversibility is key. Reversibility means you can change or take out the device. But, some effects of DBS might stay forever. It’s important to know the difference between taking out the device and reversing how it affects your body.
Temporary vs. Permanent Effects
DBS can change the brain in ways that last or not. You can adjust the stimulation, but some brain changes might stay even after the device is gone. Knowing this helps set realistic hopes for patients.
Effect Type | Description | Reversibility |
Temporary | Adjustable stimulation effects | High |
Permanent | Potential long-term neural changes | Low |
Why Reversibility Matters to Patients
For patients thinking about DBS, reversibility is a big deal. The chance to reverse DBS effects, by adjusting or removing the device, is a major factor. Patients need to know all about the possibility of reversibility and how DBS might affect their health long-term.
Understanding reversibility in DBS helps both patients and doctors make better choices. It’s important to think about the good and bad of DBS and what it might mean for the future.
Physical Components of DBS and Their Removability
A high-quality, detailed medical illustration of the physical components of a deep brain stimulation (DBS) system, showcasing the removable and non-removable parts. The image should feature a clear, well-lit view of the DBS components, including the implantable pulse generator (IPG), lead, and electrodes, against a clean, neutral background. Capture the various elements in sharp focus, highlighting their textures, materials, and precise anatomical details to convey a sense of technical precision and medical authenticity. The overall mood should be clinical, informative, and conducive to understanding the DBS system’s structure and potential for reversibility.
The Deep Brain Stimulation (DBS) system has several parts implanted in the body. These parts include the neurostimulator, extension wires, and brain electrodes. They work together to send electrical impulses to the brain.
Neurostimulator Removal Process
The neurostimulator is the main power source of the DBS system. It’s placed in the chest area, just below the collarbone. Removing it is a simple surgery.
The surgeon goes back to the original incision site. They disconnect the device from the extension wires and then take it out. This surgery is usually safe, but there are risks like infection or damage to tissues.
Extension Wire Extraction Techniques
Extension wires link the neurostimulator to the brain electrodes. They run from the chest to the head under the skin. Removing these wires is tricky to avoid harming tissues or the electrodes.
Surgeons use a method that involves pulling gently and sometimes making more cuts. This helps remove the wires completely.
Brain Electrode Removal: Possibilities and Limitations
Removing brain electrodes is the most difficult part. It requires precise surgery to protect the brain tissue. Sometimes, it’s possible to remove them, but not always.
There are cases where the risks of removal are too high. This is especially true if there’s a lot of scar tissue around the electrodes.
In summary, removing DBS components is possible but varies in complexity. It’s important for patients and doctors to understand these differences. This helps make informed decisions about DBS therapy and its reversibility.
Is DBS Truly Reversible? The Complete Picture
A close-up view of a surgeon’s hands carefully implanting a deep brain stimulation (DBS) electrode into a patient’s skull. The procedure takes place in a dimly lit operating room, with the patient’s head secured in a specialized frame. The surgeon’s movements are precise and focused, aided by the glow of medical instruments and the soft light of the room. The background is hazy and out of focus, emphasizing the importance of the delicate task at hand. The overall scene conveys the gravity and complexity of DBS surgery, reflecting the carefully considered decision-making and skill required to perform this procedure.
Deep Brain Stimulation (DBS) reversibility is more than just removing hardware. The treatment’s effects on the body and brain are not fully reversible. This is because the body and brain adapt in ways that can’t be easily undone.
Hardware Removal vs. Physiological Reversibility
Removing DBS hardware means taking out the device and its parts. But, the body’s response to these devices and the brain changes they cause are harder to reverse.
Removing the hardware is simple. But, the body’s changes and brain adaptations are complex. These changes can affect how the body and brain work, even after the devices are gone.
Tissue Changes at Electrode Sites
DBS electrodes can cause tissue changes where they are placed. These changes might include inflammation and scarring. How much these changes can be reversed is still being studied.
Research shows that the brain forms a scar around the electrodes. This scar can affect how well the electrodes work. It also makes removing the electrodes more complicated.
Long-term Neural Adaptations
DBS can change the brain in lasting ways. These changes can be both good and bad. They affect how the brain works and can change neurotransmitter levels.
Understanding the long-term effects of DBS is important. It helps patients and doctors make better choices about treatment. Knowing these effects can also help manage expectations.
Aspect | Hardware Removal | Physiological Reversibility |
Definition | Surgical extraction of DBS devices | Reversal of physiological changes caused by DBS |
Complexity | Relatively straightforward | Complex and not fully understood |
Tissue Changes | Removal of electrodes and associated hardware | Potential for some tissue changes to be irreversible |
Neural Adaptations | Does not directly address neural adaptations | Involves reversal or management of long-term neural changes |
In conclusion, DBS reversibility is complex. It involves both removing hardware and reversing body and brain changes. Understanding this is key for those considering DBS and for doctors managing it.
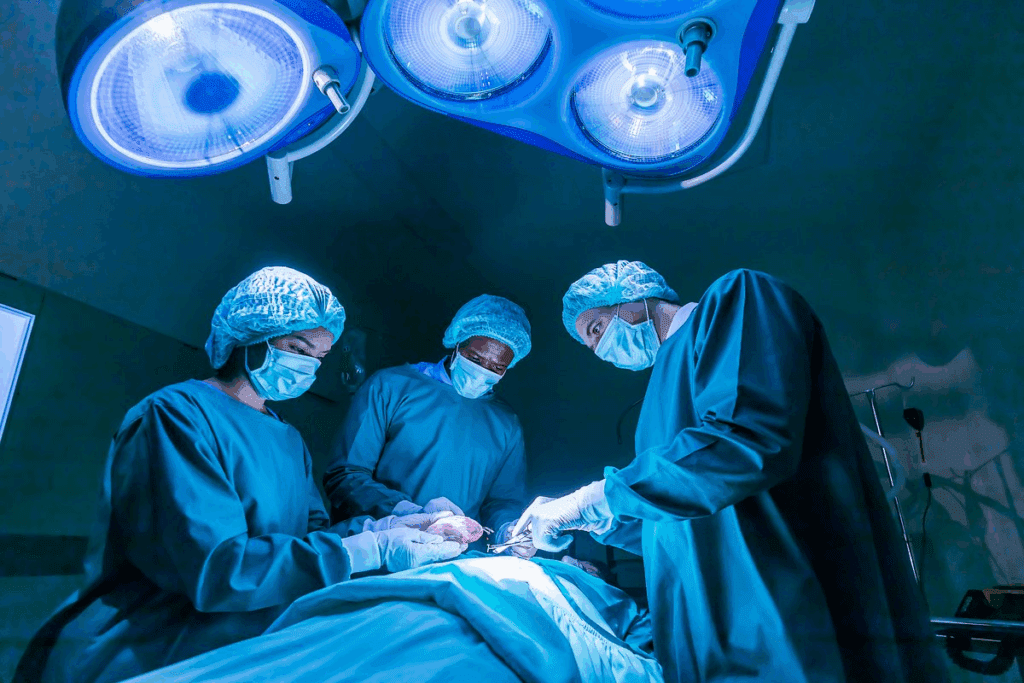
The DBS Deactivation and Removal Process
A detailed, life-like depiction of the DBS removal process. Show a surgical procedure in progress, with a neurosurgeon carefully extracting the DBS device from the patient’s brain. Depict the various components of the DBS system, including the electrode leads, extension cable, and implanted pulse generator. Capture the delicate nature of the surgery, with the neurosurgeon’s hands and surgical tools visible. Use soft, diffused lighting to create an atmosphere of precision and medical care. Render the scene in a realistic, photographic style that conveys the gravity and complexity of this procedure.
Removing a Deep Brain Stimulation (DBS) system is a detailed process. It involves several steps, from turning off the device to surgically removing it.
Temporary Deactivation Protocol
The first step is often temporary deactivation. We adjust the device’s settings to slowly reduce its effect. This helps us see how the patient will react without it.
We watch the patient’s symptoms closely during this time. We also adjust their medications as needed. This helps us prepare for the possibility of increased symptoms after removal.
Programming Adjustments Before Removal
Before surgery, we make important programming changes. We adjust the device’s settings to lessen withdrawal effects or symptom rebound. Our team works carefully to ensure a smooth transition.
These changes help manage patient expectations and reduce anxiety. By fine-tuning the device, we aim to make the removal process as comfortable as possible.
Surgical Procedure for Complete System Removal
The surgery to remove the DBS system is precise and careful. We start by removing the neurostimulator from the chest. Then, we take out the extension wires and the brain electrodes.
The surgery is done under general anesthesia or conscious sedation. Our team aims to minimize tissue damage and reduce complications.
After surgery, patients are watched closely for any issues or returning symptoms. We also guide them on post-removal care and rehabilitation. This helps them recover and adjust to life without the DBS device.
Surgical Risks of DBS Removal
A detailed surgical scene depicting the risks of deep brain stimulation (DBS) removal. In the foreground, a patient’s head is exposed, revealing the implanted DBS device. Surgical tools and equipment are arranged nearby, hinting at the complexity of the procedure. The middle ground shows a team of experienced neurosurgeons carefully navigating the delicate brain tissue, mindful of potential complications. The background is dimly lit, creating a somber, serious atmosphere befitting the gravity of the situation. Bright surgical lighting casts sharp shadows, emphasizing the precision required. The overall scene conveys the technical challenges and inherent risks associated with the reversal of this neurological intervention.
Understanding the risks of DBS removal is key. This complex procedure needs careful planning and evaluation. It’s important to know what might happen.
Potential Complications During Extraction
Removing DBS components can cause problems like infection and bleeding. It’s vital to watch patients closely before and after surgery to avoid these issues.
Scar Tissue Challenges
Scar tissue often forms after DBS removal. This can make the surgery harder and cause more symptoms. Knowing how much scar tissue there is helps plan the surgery better.
Post-Removal Monitoring Requirements
Patients need close monitoring after DBS removal. They must see their healthcare providers often to adjust treatments and handle any new symptoms.
Complication | Description | Management Strategy |
Infection | Bacterial infection at the site of DBS components | Antibiotic therapy, possible surgical drainage |
Bleeding | Hemorrhage during or after DBS removal | Immediate surgical intervention, monitoring |
Neural Tissue Damage | Damage to brain tissue during electrode removal | Careful surgical technique, post-operative monitoring |
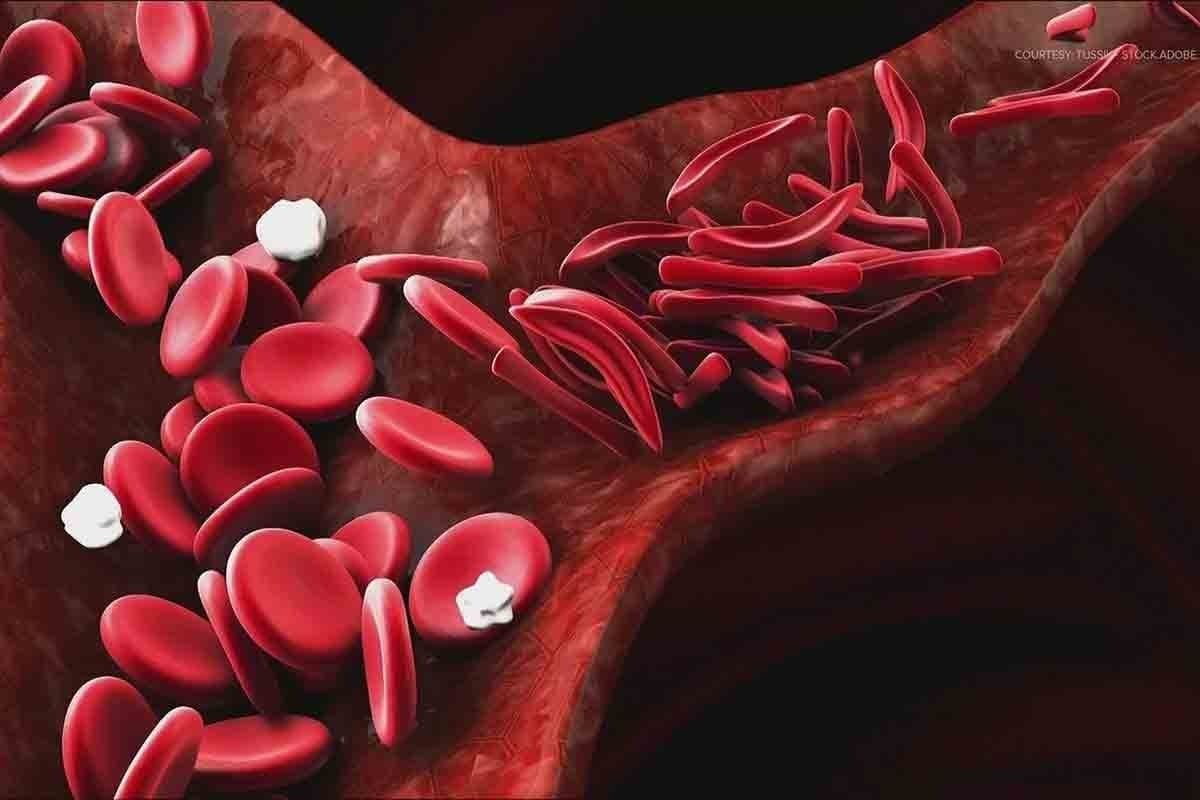
Reversibility in Parkinson’s Disease DBS Patients
A close-up view of a human head, with a detailed cross-section of the brain highlighting the deep brain stimulation (DBS) device implanted to treat Parkinson’s disease. The brain is rendered in realistic anatomical detail, with the DBS electrodes precisely placed within the targeted regions. The image has a clinical, scientific atmosphere, with muted colors and a focus on the technical aspects of the DBS procedure. The lighting is soft and directional, emphasizing the depth and complexity of the brain structure. The angle is slightly elevated, giving the viewer a sense of observing the subject from a medical professional’s perspective.
Patients with Parkinson’s disease often wonder if Deep Brain Stimulation (DBS) can be reversed. It’s important to understand how DBS affects Parkinson’s disease treatment.
Return of Motor Symptoms After Deactivation
When DBS is turned off or removed, some patients see their motor symptoms come back. The severity and timing of this return can vary significantly among individuals. Some may see symptoms return slowly over weeks or months, while others may experience a quicker return.
The adjustment period after DBS deactivation or removal requires careful management. Doctors often need to adjust medication to help control symptoms. In some cases, patients may need to go back to their pre-DBS medication levels or even higher doses.
Medication Adjustments Following DBS Removal
After DBS removal, adjusting medications is key. Patients often require a period of trial and error to find the optimal medication regimen that controls their symptoms without causing side effects. This process can be challenging and requires close monitoring by healthcare professionals.
- Medication types may need to be adjusted or changed.
- Doses may need to be increased or decreased.
- Alternative therapies may be considered.
DBS Reversibility for Psychiatric and Movement Disorders
DBS is being used more to treat complex psychiatric and neurological issues. It’s showing promise in treating depression, OCD, essential tremor, and dystonia. This raises the question of its reversibility.
Depression and OCD Treatment Reversibility
DBS has greatly helped those with treatment-resistant depression and OCD. Experts say knowing if DBS can be reversed is key for patients. Being able to stop or adjust DBS is crucial for managing side effects or changes in condition.
Studies show DBS can be reversed in these patients. But, it’s important to watch for withdrawal effects closely.
Key considerations for reversibility in depression and OCD include:
- Gradual adjustment of stimulation parameters
- Monitoring for symptom recurrence
- Potential need for alternative treatments post-DBS
Essential Tremor and Dystonia Considerations
DBS has greatly helped with movement disorders like essential tremor and dystonia. But, reversing DBS in these cases needs careful thought. It involves both removing the hardware and managing the effects of long-term stimulation.
Stopping DBS in essential tremor usually brings back the tremors. But, some may still feel some benefit. Dystonia’s response to stopping DBS can vary, with some seeing long-lasting benefits.
Neuropsychiatric Effects After Discontinuation
Stopping DBS can cause various neuropsychiatric effects. It’s important for doctors to watch patients closely and be ready to act. These effects can differ a lot from person to person, based on their condition and health.
“The discontinuation of DBS can lead to a complex array of neuropsychiatric effects, necessitating a comprehensive follow-up care plan.”
Knowing about these effects helps manage patient expectations and support them through treatment.
Comparing DBS Reversibility to Alternative Treatments
When looking into DBS therapy, it’s key to compare its reversibility to other treatments. DBS is a big deal for many neurological conditions. But, knowing how it stacks up against other options is crucial.
Lesioning Procedures vs. DBS
Lesioning, like radiosurgery, makes permanent or temporary marks in the brain. It’s used for Parkinson’s and essential tremor. Unlike DBS, it can’t be easily changed or removed.
Key differences between DBS and lesioning procedures include:
- DBS can be adjusted or removed if needed
- Lesioning is permanent and can’t be easily changed
- DBS can be customized for each patient through programming
Medication-Only Approaches
Medications are often the first choice for many conditions. They can work well, but they have limits. Unlike DBS, they can’t be turned off or adjusted as easily.
Considerations for medication-only approaches include:
- Side effects and the need for constant dosage adjustments
- Medications can be changed or stopped if needed
- They might not work for everyone
Newer Non-Invasive Brain Stimulation Methods
New methods like TMS and tDCS are non-invasive and don’t require surgery. They’re good for some conditions and are reversible. They don’t involve implanted devices.
Advantages of non-invasive brain stimulation include:
- No risk of surgical complications
- Treatment can be easily stopped or adjusted
- They might be an option for more people
In conclusion, DBS is reversible, but it’s important to look at other options too. Knowing the pros and cons of each helps patients and doctors make the best choice.
Technological Advancements Improving DBS Reversibility
Recent breakthroughs in DBS technology are changing how we think about reversibility in neuromodulation treatments. We’re exploring new ways to make Deep Brain Stimulation better. This includes several key areas of research that are crucial for making DBS procedures more reversible.
Next-Generation Electrode Designs
One big step forward is the creation of new electrode designs. These designs are more flexible and less invasive. This could make removal procedures simpler. For example, Medtronic’s latest DBS systems have advanced electrodes for better stimulation and easier removal.
“The new electrode designs are a big leap in DBS technology,” say experts. “They offer better flexibility and could lower risks during removal.”
Biodegradable Components Research
Research on biodegradable components for DBS systems is also growing. These components can dissolve or break down over time. This might mean no need for surgery to remove them. Scientists are looking into different materials, like bioresorbable metals and polymers.
- Biodegradable metals
- Bioresorbable polymers
- Nanomaterials for better biocompatibility
Minimally Invasive Removal Techniques
New surgical techniques are also key to improving DBS reversibility. We’re working on ways to remove DBS devices with less risk and complexity. This includes using advanced imaging and robotic surgery for more precise and less damaging procedures.
These advancements will greatly change DBS treatments in the future. They will make treatments more reversible and appealing to both patients and doctors.
Patient Decision-Making: The Reversibility Factor
Knowing if DBS can be reversed is key for patients. This idea greatly affects their choice to get the treatment.
Discussing Reversibility During Informed Consent
Informed consent is vital. It makes sure patients know what DBS surgery means, including if it can be reversed. We stress the need to talk about removing the hardware and its effects.
- The chance of removing the device and how it affects decisions
- The need for clear talk about the surgery for both putting in and taking out the device
- The risks and problems that can come with taking out the DBS
Knowing these details helps patients make better choices about their treatment.
Common Reasons Patients Request DBS Removal
Patients ask to have their DBS removed for many reasons, like:
- Infection or hardware problems: Sometimes, infections or issues with the hardware mean it needs to come out.
- Lack of benefit: If the DBS doesn’t work as hoped, patients might want it removed.
- Bad side effects: If the DBS causes unwanted side effects, patients might ask to have it taken out.
Knowing these reasons helps doctors support patients better during their decision-making.
Psychological Preparation for System Removal
Getting ready for DBS removal is not just about the body. It’s also about the mind. Patients need to know what to expect and what the removal process is like.
Psychological support is key. It helps patients deal with the choice to remove the DBS and adjust to life after.
By focusing on the mental side of DBS removal, we offer better care to our patients.
Expert Perspectives on DBS Reversibility
Experts have different views on whether Deep Brain Stimulation (DBS) surgery can be reversed. This shows how complex this neurosurgical procedure is. It’s important to look at what specialists in neurosurgery, neurology, and bioethics say.
Neurosurgeon Viewpoints
Neurosurgeons are key in putting in and taking out DBS devices. Medical Expert, a well-known neurosurgeon, says removing the device is complex but usually works without major problems. But, he stresses that deciding to remove a DBS device is a big choice. It depends on the patient’s health and why they want it removed.
Neurologist Assessments
Neurologists are vital in caring for patients before and after DBS surgery. Medical Expert, a neurologist who focuses on movement disorders, says DBS can greatly help Parkinson’s disease symptoms. But, she notes that reversing DBS doesn’t always mean symptoms go back to how they were before. Neurologists look at how DBS affects patients over time and what happens when it’s stopped.
Bioethical Considerations
The idea of reversing DBS also brings up big bioethical questions. Ethicists say that DBS’s reversibility is key to patient freedom and making informed choices. Medical Expert, a bioethicist, points out that patients need to know about the chance to reverse DBS and what it means. This ensures they fully understand the risks and benefits before deciding on DBS surgery.
Real Patient Experiences with DBS Removal
Choosing to have Deep Brain Stimulation (DBS) surgery is a big decision. It’s important to know what happens when you decide to remove it. Each person’s experience with DBS removal is unique.
Case Studies: Successful Removals
Many case studies show that removing DBS devices can be successful. For example, a study in the Journal of Neurosurgery talked about patients who had their devices removed. These patients saw big improvements after the removal.
A 62-year-old with Parkinson’s had his device taken out because of an infection. He got antibiotics and got better. This shows how important it is to choose the right patient and care for them well after surgery.
Case Study | Reason for Removal | Outcome |
62-year-old male with Parkinson’s | Infection | Successful removal, significant recovery |
45-year-old female with dystonia | Hardware malfunction | Device removed, symptoms managed with medication |
Challenges and Complications
Even with successful removals, some patients face problems. These can include infections, scar tissue, and symptoms coming back. It’s important for patients to know about these risks.
One big challenge is when symptoms come back after the device is removed. For example, a person with essential tremor might start shaking again. It’s crucial to plan and manage these challenges carefully.
Life After DBS: Patient Testimonials
What patients say about life after DBS removal is very helpful. Some go back to how they were before, while others face new issues. Listening to patients can give hope and advice to others thinking about removal.
A patient with Parkinson’s said, “After removal, my symptoms came back, but with the right meds, I’m doing okay.” These stories show how important it is to have full care after removal.
Insurance and Financial Considerations for DBS Removal
Thinking about removing your DBS system? Insurance and costs are big worries. The cost of this procedure can be high. It’s important to know this to make good choices about your health.
Coverage Policies for Device Removal
Insurance for DBS removal changes a lot. Some plans cover it, while others don’t. Or they might need extra okay’s. Always check with your insurance to see what they say.
Here’s what to ask your insurance:
- Is DBS removal covered by your policy?
- Do you need to get approval before the procedure?
- What will you have to pay out of pocket, like deductibles?
Advocating for Insurance Approval
Having trouble getting insurance to approve DBS removal? Here are some tips:
- Work with your doctor to get all the needed papers.
- Write a strong appeal if your first request is turned down.
- Ask for help from a patient advocate or social worker.
Knowing about insurance and money matters with DBS removal helps you make better choices. It makes the process easier and more informed.
Conclusion: The Future of Reversible Brain Stimulation Therapies
Deep brain stimulation (DBS) is getting better, thanks to new research. This includes making DBS and other brain therapies more reversible. This means they can be adjusted or stopped if needed.
New technologies are on the horizon for DBS. Things like better electrode designs and biodegradable parts are being explored. These changes will make DBS more effective and easier to reverse. This is good news for patients, as it could reduce risks over time.
DBS and other reversible brain therapies are set to change how we treat many conditions. It’s crucial to keep working on new tech that’s both effective and reversible. This will help patients get better faster and with fewer side effects.
We’re excited about the future of DBS surgery. It’s expected to lead to better results for patients. By focusing on reversible treatments, we can offer patients more flexible and effective care. This will greatly improve their quality of life.
FAQ
What is Deep Brain Stimulation (DBS) surgery?
DBS surgery is a procedure where a device called a neurostimulator is implanted. It’s like a “brain pacemaker.” This device sends electrical impulses to the brain to treat movement and mental disorders.
Is DBS surgery reversible?
DBS surgery can be reversed in some ways. The device can be turned off or removed if needed. But, the idea of reversibility is more complex, involving both hardware and how the body responds.
What conditions are treated with DBS?
DBS helps treat several conditions. These include Parkinson’s disease, essential tremor, dystonia, OCD, and depression.
How does DBS work?
DBS sends electrical stimulation to the brain. This helps control brain activity. It can reduce symptoms of various neurological and psychiatric conditions.
Can the DBS device be removed?
Yes, the DBS device can be removed. First, the device is turned off. Then, a surgery is done to take out the neurostimulator and other parts.
What are the risks associated with DBS removal?
Removing DBS can have risks. These include complications during the surgery, scar tissue issues, and needing to monitor the body after removal.
Will symptoms return after DBS deactivation or removal?
Yes, symptoms can come back after DBS is turned off or removed. This might mean changing medications or trying other treatments.
How do technological advancements impact DBS reversibility?
New technologies are making DBS removal safer and easier. Advances include better electrode designs, biodegradable parts, and less invasive removal methods.
How does DBS reversibility compare to alternative treatments?
DBS is more flexible than some treatments, like lesioning, which can’t be reversed. DBS allows for adjustments or removal if needed.
What are the insurance and financial considerations for DBS removal?
Insurance for DBS removal varies. Patients might have to pay out of pocket. It’s important to fight for insurance approval and understand policies to manage costs.
How does patient decision-making involve DBS reversibility?
Knowing about DBS reversibility is key for patients. It helps them make informed choices about treatment and understand the options for device removal.
What are the long-term outcomes after DBS removal?
Results after DBS removal vary. They depend on the condition and the individual. Some might see symptoms return, while others might do better.