Last Updated on December 1, 2025 by Bilal Hasdemir

Acute myeloid leukemia (AML) is the most deadly leukemia in kids. It grows fast and has lower survival rates than other types of leukemia.
Understanding AML is key because it affects kids’ health a lot. Studies show we need to find it early and treat it well.
It’s vital to keep researching and spreading the word about AML. This disease is a big health problem for kids all over the world.
Key Takeaways
- Acute myeloid leukemia (AML) is the deadliest form of leukemia in children.
- AML has a lower survival rate compared to other types of leukemia.
- Early detection and effective treatment are critical in fighting AML.
- Awareness and research into AML are essential for better outcomes.
- AML significantly impacts children’s health globally.
Understanding Childhood Leukemia
Childhood leukemia is a complex disease that affects thousands of kids every year. It starts in the blood and bone marrow, messing with blood cell production. Leukemia comes in several types, each with its own challenges.
Types of Leukemia Affecting Children
There are two main types of leukemia in kids: Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML). ALL is the most common, making up 80% of cases. AML is more aggressive and has a worse outlook. Knowing the differences is key for effective treatment.
ALL usually has a better chance of survival than AML. But, some ALL subtypes with genetic issues have a tougher road. AML, being more aggressive, often leads to higher death rates.
How Leukemia Develops in Children
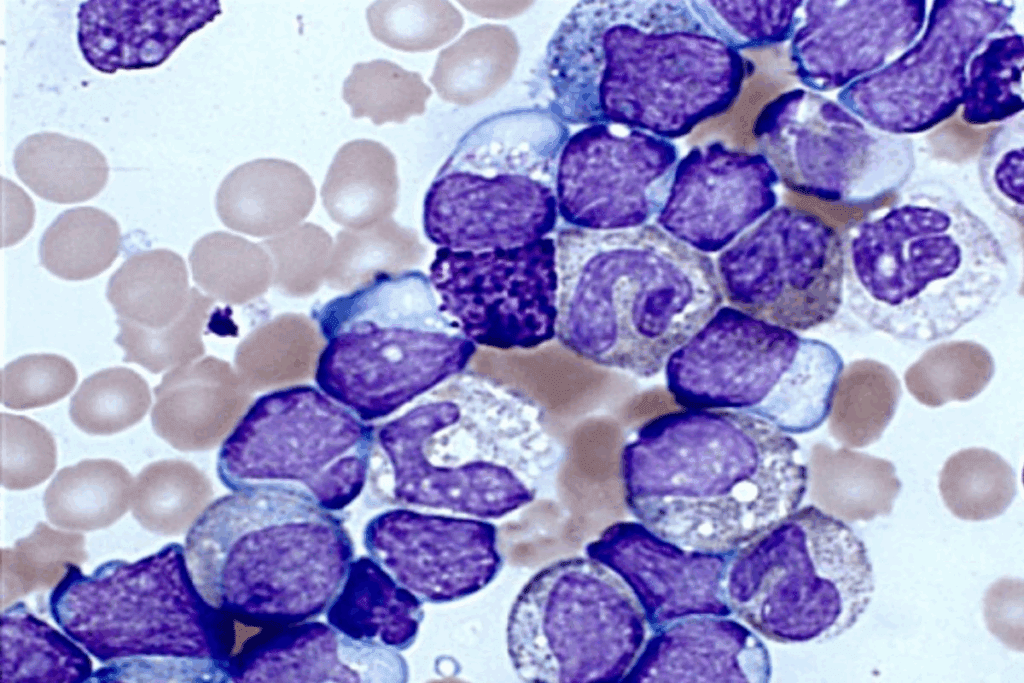
Leukemia starts with a genetic mutation in bone marrow cells. This leads to abnormal white blood cells, crowding out healthy ones. What causes these mutations is often a mystery, but some factors like genetics and environment can raise the risk.
In kids, untreated leukemia can spread fast, causing serious problems or even death.
“Early diagnosis and treatment are critical in improving survival rates and reducing the risk of long-term health consequences.”
Grasping how leukemia starts is vital for creating better treatments and improving outcomes.
The Deadliest Leukemia in Children: Acute Myeloid Leukemia
Acute Myeloid Leukemia (AML) is the deadliest leukemia in kids. It grows fast and doesn’t respond well to treatment. This makes it very hard to cure.
Why AML Has Higher Mortality Rates
AML is deadly because it attacks quickly and is hard to treat. It’s different from other leukemias because it doesn’t get better with common treatments.
Key factors contributing to AML’s high mortality include:
- Rapid disease progression
- Limited response to initial chemotherapy
- Higher risk of relapse
- Presence of high-risk genetic mutations
A top pediatric oncologist says, “Treating AML is a big challenge. We need new ways to help kids get better.”
“The treatment of AML remains one of the most significant challenges in pediatric oncology…”
Subtypes of AML with Poor Prognosis
Some AML types are very hard to treat in kids. These include:
| Subtype | Characteristics | Prognosis |
| AML with t(8;21) | Favorable genetic abnormality | Generally better prognosis |
| Acute Promyelocytic Leukemia (APL) | Characterized by t(15;17) | High cure rate with appropriate treatment |
| AML with complex karyotype | Multiple genetic abnormalities | Poor prognosis |
Knowing about these subtypes helps us find better treatments for kids with AML.
Other High-Risk Childhood Leukemias

Leukemia types like AML, ALL with high-risk features, and rare aggressive variants are big challenges in pediatric oncology. AML has high mortality rates. But, other leukemia types with high-risk features need a deep understanding and specific treatments.
Acute Lymphoblastic Leukemia (ALL) with High-Risk Features
ALL is the most common leukemia in kids, making up 80% of all childhood leukemia cases. But, some high-risk features make it harder to treat. These include high white blood cell counts at diagnosis, presence of certain genetic abnormalities like the Philadelphia chromosome, and poor response to initial therapy.
Children with these high-risk features need more intense treatments. This might include targeted therapies and stem cell transplantation.
“The prognosis for children with high-risk ALL has improved a lot with modern treatments,” says a top pediatric oncologist. “But, we need to keep researching to make things even better for these kids.”
Rare and Aggressive Leukemia Variants
There are also rare and aggressive leukemia variants that are tough to handle. These include mixed-phenotype acute leukemia (MPAL) and other leukemias with unclear lineage. MPAL, for example, shows traits of both myeloid and lymphoid leukemias, making diagnosis and treatment very complex.
- Mixed-Phenotype Acute Leukemia (MPAL): This rare subtype lacks clear lineage distinction, complicating treatment decisions.
- Other rare variants: Include leukemias with unusual genetic or immunophenotypic features that don’t fit into standard categories.
Treatment for these rare and aggressive variants often needs a very personalized approach. It might include parts from different treatment plans and sometimes new drugs.
Risk Factors for Developing Deadly Forms of Leukemia
Deadly leukemia in kids is often tied to certain genes and the environment. Knowing these risks helps us find ways to prevent and treat the disease better.
Genetic Predispositions
Genes play a big part in leukemia. Kids with Down syndrome are at higher risk. Also, genes that control cell growth can lead to leukemia.
For example, changes in the TP53 gene, a tumor fighter, raise cancer risk. Families with cancer history might also face higher risks due to inherited genes.
Environmental Factors
Environment also affects leukemia risk. High ionizing radiation from nuclear accidents or some medical treatments increases risk. Chemicals like benzene in industrial settings also raise the risk.
While these factors can up the risk, they don’t mean leukemia is certain. Research is ongoing to understand how genes and environment interact in leukemia.
Recognizing Symptoms of Aggressive Childhood Leukemia
Finding leukemia early in kids is key to better survival rates and fewer complications. Leukemia, like Acute Myeloid Leukemia (AML) and high-risk Acute Lymphoblastic Leukemia (ALL), shows signs that look like other common illnesses in kids.
Early Warning Signs
Look out for signs like unexplained weight loss and pale skin. Kids might also get bruising or spots on their skin from bleeding. Bone or joint pain can also be a sign of leukemia.
“Early detection is key to effective treatment,” say pediatric oncologists. Spotting these signs early can greatly help kids with leukemia.
When to Seek Immediate Medical Attention
If your child has trouble breathing, severe bleeding, or a high fever, get help right away. Also, watch for enlarged lymph nodes, spleen, or liver, and sudden changes in behavior or brain function.
- Severe or persistent fever
- Unexplained bruising or bleeding
- Persistent bone pain
- Swollen lymph nodes or spleen
Seeing a doctor quickly is very important. Early diagnosis and treatment can greatly improve a child’s chances with aggressive leukemia.
Diagnosis and Classification of High-Risk Leukemia
Diagnosing leukemia in children needs advanced tests and expert doctors. It’s key to find the right treatment. Knowing the exact type of leukemia is vital.
Diagnostic Procedures
Tests for leukemia include bone marrow biopsies and genetic analysis. These help find leukemia cells and know the disease’s extent.
The first step is a detailed medical history and physical check-up. If leukemia is thought of, several tests are done:
- Complete Blood Count (CBC) to check for abnormal blood cell counts
- Bone marrow aspiration and biopsy to examine the bone marrow for leukemia cells
- Imaging tests such as X-rays, CT scans, or MRI scans to assess the extent of the disease
- Genetic testing to identify specific genetic mutations associated with leukemia
Risk Stratification in Childhood Leukemia
Risk stratification is key in leukemia diagnosis. It helps find high-risk cases needing intense treatment. The type of leukemia, genetic traits, and initial treatment response are considered.
This approach helps tailor treatment to each child. Risk stratification balances treatment intensity with risks and side effects.
Treatment Challenges and Approaches
Treating leukemia in children is a complex task. It involves many challenges and needs a multi-faceted approach. The disease is aggressive, making treatment hard and requiring targeted therapies.
Standard Treatment Protocols
For childhood leukemia, chemotherapy is the main treatment. The type and length of chemotherapy depend on the leukemia’s type and risk. Risk stratification helps decide the treatment’s intensity.
Chemotherapy is often combined with intrathecal therapy. This is to prevent the disease from spreading to the brain.
Stem Cell Transplantation
Stem cell transplantation is key for high-risk or relapsed leukemia. It replaces the patient’s bone marrow with healthy stem cells. These can be from the patient (autologous transplant) or a donor (allogeneic transplant).
Choosing between autologous and allogeneic transplant depends on several factors. These include the patient’s health, the leukemia’s characteristics, and donor availability.
Managing Treatment Complications
Managing complications is vital for children with leukemia. Common issues include infections, organ toxicity, and long-term side effects. These can be secondary cancers or developmental problems.
Supportive care is essential. This includes antimicrobial prophylaxis, growth factor support, and monitoring organ function. These steps help reduce complications and improve outcomes.
Recent Advancements in Fighting Deadly Childhood Leukemias
The fight against childhood leukemia is getting a boost from new treatments. Immunotherapy and targeted treatments are showing great promise. They are helping to improve the lives of kids with leukemia.
Immunotherapy and Targeted Treatments
Immunotherapy uses the body’s immune system to fight cancer. “CAR-T cell therapy, a form of immunotherapy, has shown significant efficacy in treating relapsed or refractory leukemia,” studies say. Targeted treatments, by contrast, aim at specific genetic mutations that cause leukemia.
These methods are more precise, harming fewer healthy cells and causing fewer side effects. The use of targeted therapies has led to better survival rates for some leukemia types.
Promising Clinical Trials and Research
Clinical trials are exploring new ways to combine immunotherapy and targeted treatments. A top pediatric oncology researcher, believes in personalized medicine. “Therapies should be tailored to each patient’s unique genetic profile,” she says.
Researchers are also working to understand why some treatments don’t work. A doctor explains, “Knowing the genetic roots of leukemia is key to finding effective treatments.”
These breakthroughs bring hope to kids with leukemia. They offer better survival chances and a better quality of life.
Conclusion: Hope Amid the Challenge
Childhood leukemia is a tough battle, affecting many families and healthcare teams. But, thanks to new research, kids with leukemia have a better chance of beating the disease.
It’s important to understand how leukemia can come back in kids. This knowledge helps doctors find new ways to fight it. Thanks to ongoing studies, we now have better treatments for leukemia.
Even though there’s more to do, the progress we’ve made is promising. We need to keep working on finding better ways to treat leukemia. This will help more kids survive and thrive.
Working together is key to making a difference in leukemia treatment. Researchers, doctors, and families must join forces. This way, we can improve how we treat leukemia and help more kids win their fight against this disease.
FAQ
What is the deadliest form of leukemia in children?
Acute Myeloid Leukemia (AML) is the deadliest form of leukemia in kids. It has higher death rates and is very aggressive.
What are the main differences between AML and ALL?
AML and ALL are two different types of leukemia. AML is more aggressive and has a worse outlook than ALL.
What are the risk factors associated with developing deadly forms of leukemia?
Genetic predispositions, environmental factors, and certain medical conditions can raise the risk of deadly leukemia. Knowing these risk factors is key for prevention and early detection.
What are the early warning signs of aggressive childhood leukemia?
Symptoms include fatigue, pale skin, frequent infections, and easy bleeding or bruising. Parents should get medical help if they notice unusual or ongoing symptoms.
How is leukemia diagnosed and classified?
Diagnosing leukemia involves physical exams, blood tests, bone marrow biopsies, and genetic tests. It’s classified into risk categories to guide treatment.
What are the treatment challenges for leukemia?
Treating leukemia is complex due to its variety, resistance to treatment, and complications. Personalized plans, stem cell transplants, and managing complications are key to better outcomes.
What are the recent advancements in fighting deadly childhood leukemias?
Recent advances include immunotherapy, targeted treatments, and clinical trials. These are improving survival rates for kids with leukemia. Research aims to find more effective and less harmful treatments.
What is the prognosis for children with high-risk leukemia?
The prognosis depends on the leukemia type, subtype, and risk category. Children with high-risk leukemia need aggressive treatment and close monitoring for better survival chances.
Can leukemia be prevented?
While there’s no sure way to prevent leukemia, avoiding environmental toxins can help. Research is ongoing to find prevention strategies.
What is the role of stem cell transplantation in treating leukemia?
Stem cell transplantation is a key treatment for high-risk leukemia. It offers a chance for cure in aggressive or relapsed cases.
References
- Vallet, P., et al. (2024). Infections in children and adolescents with Acute Leukemia. European Journal of Pediatrics. https://www.sciencedirect.com/science/article/pii/S2772610X24000011