Last Updated on December 2, 2025 by Bilal Hasdemir
deep brain stimulation
People with Parkinson’s disease and other movement disorders often struggle with balance. This can really affect their daily life and how independent they feel. Deep Brain Stimulation (DBS) is seen as a hopeful treatment for these balance problems.
We look into how DBS surgery might help with balance for those with Parkinson’s and other movement disorders. Learning about DBS’s effects on balance helps us see its value in improving lives.
Key Takeaways
- DBS is a neurosurgical procedure that treats movement disorders.
- Balance issues are common in Parkinson’s disease and other movement disorders.
- DBS surgery has the potential to improve balance in affected individuals.
- Understanding DBS’s impact on balance can enhance patient care.
- DBS is a promising treatment for managing symptoms of Parkinson’s disease.
Understanding Deep Brain Stimulation (DBS)
A high-resolution, photorealistic image of a human brain cross-section, with a detailed view of the deep brain structures. The image should have a clinical, scientific atmosphere, with a clean, minimalist background that emphasizes the subject. Showcase the intricate neural pathways and the precise placement of the deep brain stimulation electrodes, illuminated by a soft, directional light source. Convey a sense of medical precision and technological advancement, while maintaining a sense of the brain’s organic complexity. The overall composition should be visually striking and informative, suitable for illustrating the "Understanding Deep Brain Stimulation (DBS)" section of the article.
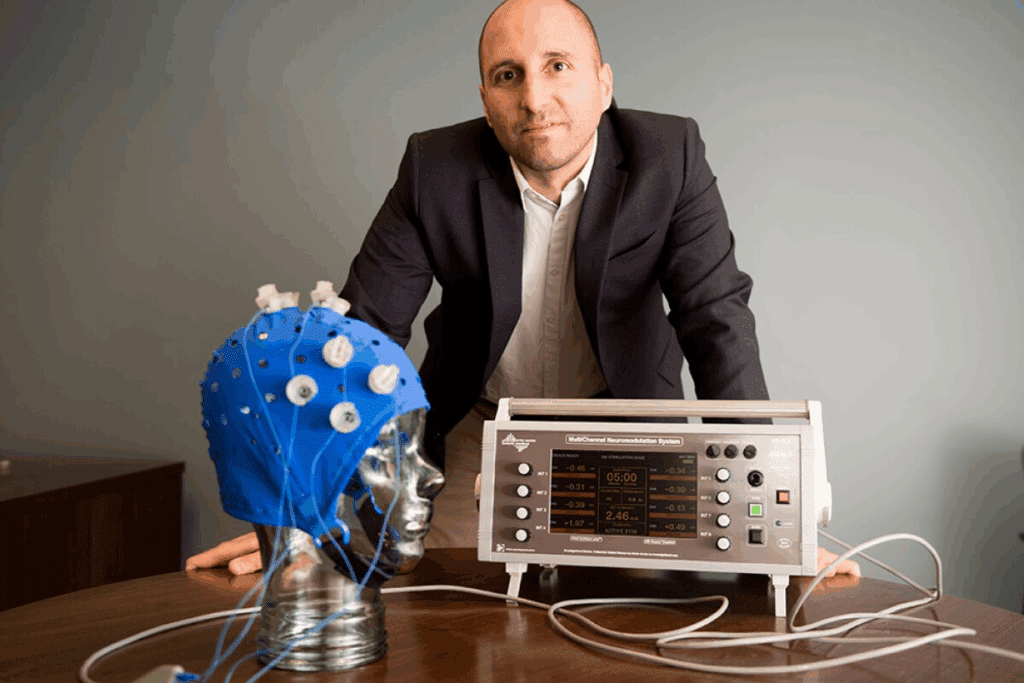
Deep Brain Stimulation (DBS) is a groundbreaking neurosurgical method. It has changed how we treat movement disorders. It involves putting electrodes in the brain and using a neurostimulator to send signals, like a brain pacemaker.
What is Deep Brain Stimulation?
DBS is a complex treatment that controls abnormal brain signals. It helps with conditions like Parkinson’s disease, essential tremor, and dystonia. By sending electrical impulses to certain brain areas, it can greatly reduce symptoms, enhancing patients’ lives.
A team of neurosurgeons, neurologists, and other experts work together. They decide if DBS is right for a patient and customize the treatment for their needs.
How DBS Surgery Works
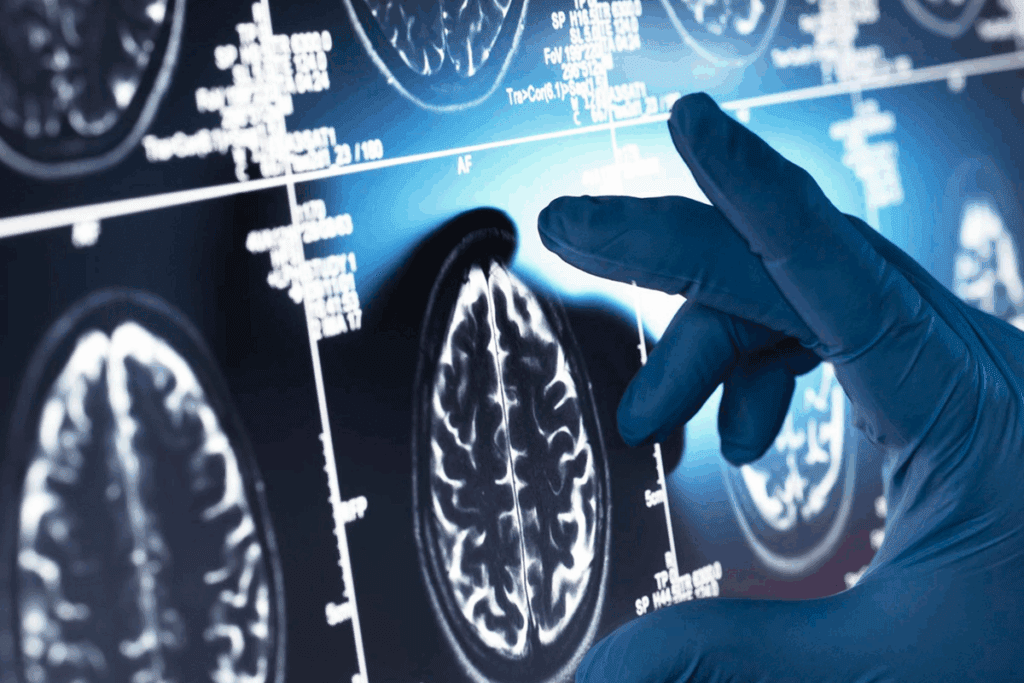
The DBS surgery is detailed and involves several steps. First, patients have a detailed check-up to find the best spot for the electrodes. This includes using MRI and CT scans.
During surgery, a neurosurgeon places the electrodes in the chosen brain area. Then, they connect the electrodes to a neurostimulator, usually in the chest. This device sends the electrical impulses to the brain.
Target Brain Areas for Stimulation
The success of DBS relies on hitting the right brain spots. Common targets are the subthalamic nucleus (STN), globus pallidus interna (GPi), and ventral intermediate nucleus (Vim) of the thalamus. The target depends on the patient’s condition and symptoms.
For example, STN stimulation is often used for Parkinson’s disease. GPi stimulation might be better for dystonia. Finding the exact spot is key to getting the most benefit from DBS while avoiding side effects.
Balance Problems in Neurological Disorders

A person struggling to maintain balance, their posture unsteady, caught in a moment of neurological disorder. The scene is illuminated by a soft, natural light, casting subtle shadows that accentuate the subject’s loss of equilibrium. The background is blurred, drawing the viewer’s attention to the focal point – the individual’s fight against their balance challenges. The composition is carefully crafted, with the subject positioned in the center, conveying a sense of vulnerability and the need for support. The overall atmosphere is one of empathy and understanding, inviting the viewer to consider the daily struggles faced by those living with neurological conditions.
Neurological disorders often cause balance problems. This can greatly affect patients’ lives. It increases the risk of falls and injuries, making it a key part of care.
Common Balance Issues in Parkinson’s Disease
Parkinson’s disease causes tremors, stiffness, and slow movements. A big challenge is postural instability, which can lead to falls. Studies say falls in Parkinson’s are due to both motor and non-motor symptoms.
Patients with Parkinson’s may feel like their feet are stuck, leading to falls. Postural instability gets worse with medication changes and disease progression.
Balance Dysfunction in Essential Tremor
Essential tremor mainly affects the hands with action tremors. It’s less common than Parkinson’s but can still cause balance problems. Research shows patients struggle with tandem gait and standing balance.
The causes of balance issues in essential tremor are complex. They involve the cerebellum and possibly other brain areas. Knowing this helps in finding better treatments.
Postural Instability in Dystonia and Other Movement Disorders
Dystonia causes involuntary muscle contractions, leading to repetitive movements or abnormal postures. Postural instability is common, especially in neck and trunk dystonias. Patients face balance challenges due to unpredictable movements.
Other disorders like multiple system atrophy and progressive supranuclear palsy also have balance problems. These conditions progress faster than Parkinson’s and can cause severe instability early on.
Managing balance problems in these disorders requires a comprehensive approach. This includes medical treatment, physical therapy, and sometimes surgery like Deep Brain Stimulation (DBS).
The Neurological Control of Balance
A detailed cross-section of the human brain, with distinct regions highlighted to illustrate the intricate neural systems responsible for balance regulation. The image should convey a sense of scientific precision and visual clarity, with a balanced composition showcasing the frontal lobe, cerebellum, brainstem, and other key structures involved in maintaining postural equilibrium. Realistic lighting and subtle textures should enhance the anatomical realism, allowing the viewer to appreciate the complexity of the brain’s balance control mechanisms. The overall tone should be informative and educational, supporting the article’s discussion of deep brain stimulation and its potential impact on balance disorders.
Balance is more than just standing still. It’s a complex process that involves many parts of our brain. It needs the integration of sensory inputs and motor responses.
Brain Regions Involved in Balance Regulation
The brain has a network for balance. The cerebellum coordinates movement and balance. The vestibular nuclei handle information about spatial orientation and movement.
The basal ganglia and motor cortex also play key roles. They help us move and stay balanced. This teamwork is what keeps us upright and moving smoothly.
How Neurological Disorders Disrupt Balance Control
Neurological disorders can mess with balance by affecting the brain’s balance centers. For example, Parkinson’s disease can cause instability because of its impact on motor control.
Other conditions like essential tremor and dystonia can also disrupt balance. Knowing how these disorders affect balance is key to finding good treatments.
Neurological Disorder | Impact on Balance |
Parkinson’s Disease | Postural instability, gait disturbances |
Essential Tremor | Tremors affecting balance during movement |
Dystonia | Involuntary movements disrupting posture |
The Connection Between Gait and Balance
Gait and balance are closely linked. A person’s gait can greatly affect their balance. Disorders that change how we walk can make balance harder.
On the other hand, balance problems can lead to changes in how we walk. People might change their stride to stay balanced. It’s important to understand this link for diagnosing and treating balance issues.
Deep Brain Stimulation for Movement Disorders
A close-up view of a human brain, with a deep brain stimulation (DBS) device implanted. The brain is rendered in high detail, with intricate neural pathways and blood vessels visible. The DBS device, a small metallic implant, is positioned precisely within the brain, secured by delicate surgical hardware. The image is captured with a professional-grade camera, using soft, directional lighting to accentuate the device’s form and the brain’s intricate structure. The overall mood is one of scientific precision and medical innovation, conveying the complex and transformative nature of DBS therapy for movement disorders.
Deep Brain Stimulation (DBS) is a new hope for patients with movement disorders. It’s a game-changer that offers relief from symptoms. We’ll look at how DBS helps, its history, and its approved uses in the U.S.
Evolution of DBS as a Treatment Option
DBS has grown a lot since it started. It used to be a last choice, but now it’s considered sooner for the right patients.
Year | Milestone |
1987 | First DBS surgery by Dr. Benabid |
1997 | FDA okayed DBS for essential tremor |
2002 | FDA okayed DBS for Parkinson’s disease |
2003 | FDA okayed DBS for dystonia |
Approved Uses in the United States
In the U.S., DBS is approved for Parkinson’s disease, essential tremor, and dystonia. It’s for those who haven’t gotten better with other treatments or have bad side effects from medicines.
As DBS keeps getting better, we’ll see more ways it can help with movement disorders.
The DBS Surgical Procedure and Recovery
A meticulously detailed surgical scene depicting a deep brain stimulation (DBS) procedure. The foreground features a neurosurgeon’s steady hands performing the intricate operation, with precise incisions and the implantation of electrodes deep within the patient’s brain. The middle ground showcases the surrounding medical equipment, from the advanced imaging systems monitoring neural activity to the specialized tools required for the delicate procedure. The background maintains a clinical atmosphere, with sterile lighting and the hushed focus of the medical team. Capture the gravity and intensity of this life-changing surgery, conveying the hope it offers for improved balance and quality of life for the patient.
The DBS surgery includes steps before, during, and after the procedure. This ensures patients get the most from their Deep Brain Stimulation therapy.
Preoperative Evaluation and Planning
Before DBS surgery, patients go through a preoperative evaluation. This involves tests to see if they’re a good fit for DBS therapy. Our team looks at their medical history and health to find out the surgery’s risks and benefits.
During planning, we use MRI or CT scans to find the right spots in the brain for the electrodes. This careful planning helps make the DBS therapy work better.
The Implantation Process
The DBS implantation process is a detailed surgery. First, the patient gets local anesthesia and a frame is put on their head. This helps guide the surgical tools.
Using imaging, the neurosurgeon finds the exact spot for the DBS electrodes in the brain. The electrodes are then placed carefully. Their position is checked with imaging and tests. After, they’re connected to a pulse generator under the skin in the chest. The whole thing takes a few hours, and the patient is watched closely.
Immediate Post-Surgical Effects on Balance
Right after DBS surgery, patients might see changes in their balance. Some might feel better, while others might struggle due to swelling or the body’s reaction to the device.
Our team keeps a close eye on the patient’s balance and health during recovery. We help with post-surgery care and rehab to improve their DBS therapy results. Sometimes, we need to adjust the DBS device to better its effects and reduce any balance issues.
Research Evidence: DBS and Balance Improvement
A high-resolution, hyper-realistic photographic image of a neurosurgeon performing deep brain stimulation (DBS) surgery on a patient to improve their balance and stability. The patient is lying on an operating table in a bright, sterile medical theater, with the surgeon focused intently on implanting the DBS electrodes. The lighting is crisp and evenly distributed, capturing every minute detail of the procedure. The perspective is from an angle slightly above the patient, providing a clear view of the surgeon’s skilled hands at work. The atmosphere is one of precision, innovation, and the pursuit of medical advancement.
A growing body of research looks into how DBS affects balance in those with movement disorders. This section will cover the clinical evidence supporting DBS for better balance.
Clinical Studies on Balance Outcomes
Many clinical studies have looked into DBS’s impact on balance in Parkinson’s disease and other movement disorders. They use standardized rating scales and posturography to assess balance.
Table: Summary of Clinical Studies on DBS and Balance
Study | Patient Population | Balance Assessment | Outcome |
Study 1 | Parkinson’s Disease | Posturography | Improved postural stability |
Study 2 | Essential Tremor | Balance rating scales | Significant balance improvement |
Study 3 | Dystonia | Gait analysis | Enhanced gait stability |
Measuring Balance Changes After DBS
Balance changes after DBS are measured with clinical rating scales and posturography. These tools give a full picture of a patient’s balance.
Long-term Effects on Postural Stability
Long-term studies show DBS can lead to lasting improvements in postural stability for many. But, results can differ, and ongoing monitoring is key to fine-tune DBS settings.
We see DBS’s potential in improving balance, but more research is needed. We aim to fully grasp its long-term effects and refine who benefits most.
DBS Effects on Gait and Mobility
A middle-aged person walking with a cane, their gait slightly unsteady, in a brightly lit, clinical medical setting. The person’s movements are captured from the side, with a focus on the lower body and legs. The background is clean and minimalist, with a hint of medical equipment or furnishings to suggest a hospital or clinic environment. The lighting is warm and natural, emphasizing the person’s determination and the challenges they face in maintaining mobility. The overall mood is one of exploration and the pursuit of improved quality of life through medical intervention.
DBS therapy has shown promising results in improving gait and mobility for individuals with Parkinson’s disease and other movement disorders. It’s essential to understand the complexities of mobility issues in neurological conditions.
Impact on Walking Speed and Stride Length
Studies have shown that DBS can significantly improve walking speed and stride length in patients with Parkinson’s disease. Increased walking speed and improved stride length are notable benefits. They contribute to enhanced overall mobility.
According to research, “DBS therapy can lead to a significant improvement in gait velocity and stride length. This improves functional mobility.”
Freezing of Gait Improvements
Freezing of gait is a common and debilitating symptom in advanced Parkinson’s disease. DBS has been shown to reduce the frequency and severity of freezing episodes in some patients. As noted by a study, “DBS can significantly reduce freezing of gait in patients with Parkinson’s disease. This improves their overall quality of life.”
Changes in Overall Mobility Patterns
DBS not only affects specific aspects of gait but also influences overall mobility patterns. Patients often experience improved turning ability and reduced postural instability. These changes contribute to a more stable and confident gait.
These changes enhance the patient’s independence and mobility. As we continue to explore the benefits of DBS, it’s clear that its effects on gait and mobility are multifaceted. By understanding these impacts, we can better tailor treatment strategies to individual patient needs. This ultimately improves their quality of life.
Comparing DBS Targets for Balance Enhancement
DBS is getting better, and knowing the differences in stimulation targets is key. Targets like the Subthalamic Nucleus (STN) and Globus Pallidus Interna (GPi) are being studied. They help us understand how to improve balance.
Subthalamic Nucleus (STN) Stimulation
The Subthalamic Nucleus is a common target for DBS in Parkinson’s disease. STN stimulation has been shown to improve motor symptoms, including balance, in many patients. Studies show it can greatly improve how stable patients stand and walk.
But, how well STN DBS works for balance can change from person to person. Some studies say it works best for those with big changes in their symptoms.
Globus Pallidus Interna (GPi) Stimulation
The Globus Pallidus Interna is another important target for DBS, especially for dystonia and Parkinson’s disease. GPi stimulation can improve motor symptoms and sometimes balance. The effects of GPi DBS on balance are generally considered to be more variable than those of STN DBS.
Research comparing STN and GPi DBS shows both can help with balance. But, how much it helps can vary. Choosing between STN and GPi depends on the patient’s symptoms and overall health.
Emerging Alternative Targets
Other brain areas are being looked at for DBS to improve balance. These include the pedunculopontine nucleus (PPN) and the zona incerta. Early research suggests that these alternative targets may offer additional benefits for balance and gait improvement.
There’s growing interest in tailoring DBS to each patient. This could lead to better balance improvement in the future.
DBS Target | Primary Indication | Balance Improvement |
STN | Parkinson’s Disease | Significant improvement in postural stability and gait |
GPi | Dystonia, Parkinson’s Disease | Variable improvement, generally less consistent than STN |
PPN | Gait and Balance Disorders | Promising early results, further research needed |
DBS Programming and Adjustments for Balance
DBS therapy’s success in improving balance depends on precise programming and adjustments. This process involves adjusting stimulation parameters to enhance therapy effects while reducing side effects.
Initial Programming Strategies
Setting up DBS therapy starts with choosing the right electrode contacts and adjusting stimulation parameters. We aim to improve balance and minimize side effects.
- Selecting optimal electrode contacts based on anatomical targeting and patient response.
- Configuring initial stimulation parameters, including amplitude, pulse width, and frequency.
- Monitoring patient response and adjusting parameters as needed.
Fine-tuning Stimulation Parameters
Fine-tuning DBS settings is an ongoing task. We watch patient outcomes and adjust settings to better improve balance.
Key considerations for fine-tuning include:
- Assessing changes in balance and mobility.
- Monitoring for potential side effects, such as dyskinesia or speech disturbances.
- Adjusting stimulation parameters to achieve the optimal balance between efficacy and side effect management.
Balance-Specific Programming Considerations
When programming DBS for balance, we focus on specific factors. These include the patient’s posture, gait, and mobility. Tailoring DBS programming to these aspects enhances therapy effectiveness.
Balance-specific considerations involve:
- Assessing postural stability and making adjustments to improve it.
- Evaluating gait patterns and optimizing DBS settings to enhance walking ability.
- Monitoring overall mobility and adjusting stimulation parameters accordingly.
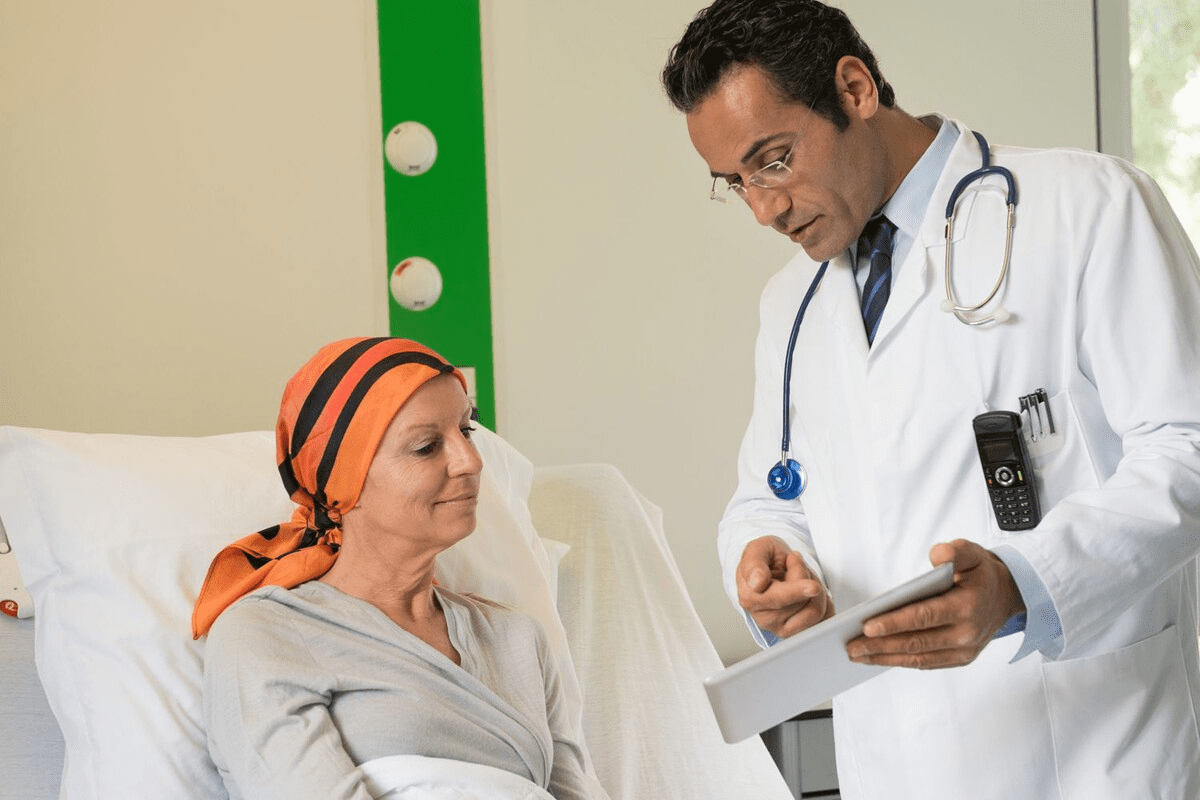
Patient Selection: Who Benefits Most from DBS for Balance Issues?
Choosing the right patients is key for Deep Brain Stimulation (DBS) therapy success. As we learn more about DBS, it’s clear that picking the right patients is crucial. This ensures the best results for those with balance problems.
Ideal Candidates for Balance Improvement
Finding the right candidates for DBS therapy requires a detailed evaluation. Patients with movement disorders like Parkinson’s disease or essential tremor might benefit. They should have tried other treatments without success and have a condition DBS can help with.
It’s also important to consider cognitive function and overall health. Those with severe cognitive issues or major health problems might not be good candidates. A team of experts must assess each patient to see if DBS is right for them.
Predictors of Positive Balance Outcomes
Studies have found several signs that DBS will work well for balance issues. Assessing balance before surgery is key, as those with severe problems might see the most improvement. How well a patient responds to levodopa medication also predicts DBS success.
- Severity of balance dysfunction
- Response to levodopa medication
- Presence of comorbidities
- Cognitive function
By looking at these factors, we can guess who will likely see big improvements with DBS therapy.
Contraindications and Risk Factors
DBS is not for everyone. Patients with significant cognitive impairment or dementia might not benefit much. In fact, DBS could make their cognitive problems worse.
Other risks include severe psychiatric conditions, major brain shrinkage, or other health issues that raise surgery risks. It’s vital to carefully weigh the benefits against the risks for each patient.
By carefully choosing patients for DBS therapy, we can make sure it works best for those with balance issues.
Limitations of DBS in Treating Balance Problems
DBS can help with some balance issues, but it has its limits. It’s important to know what this therapy can and can’t do.
Balance Symptoms Resistant to DBS
Not all balance problems get better with DBS. Some people still have trouble balancing even after treatment. Research shows certain factors can predict how well DBS will work.
- Severity of balance impairment
- Presence of other neurological symptoms
- Duration of balance problems
- Specific characteristics of the underlying condition
A study in the Journal of Neurosurgery found that those with severe balance issues at the start might not see as much improvement. 1 This shows why early treatment and choosing the right patients are key.
When DBS May Not Be Appropriate
DBS isn’t always the best choice for balance problems. It might not be right when surgery risks are too high or other treatments are better.
DBS might not be suitable in cases like:
- Significant cognitive impairment
- Severe psychiatric conditions
- Medical conditions that increase surgical risk
In summary, DBS can greatly help with balance in some cases. But, it’s vital to understand its limits and possible downsides. This knowledge helps doctors make better choices for their patients.
Combining DBS with Other Therapies for Optimal Balance
Using DBS with other therapies can really help improve balance and lower fall risks. DBS is great for managing symptoms of neurological disorders. But, it works even better when paired with other treatments.
Physical Therapy and Rehabilitation
Physical therapy is key for patients to regain and keep their balance after DBS surgery. A custom rehab program can boost mobility and cut down on falls. Important parts of physical therapy include:
- Balance Training: Exercises to test and boost balance.
- Gait Training: Ways to better walking and reduce freezing.
- Strengthening Exercises: Building muscle for better posture and balance.
- Flexibility and Range of Motion Exercises: Making movement easier and more flexible.
Adding physical therapy to their care plan can lead to big improvements in balance and life quality.
Medication Adjustments After DBS
After DBS surgery, changing medications is often needed to get the best results. Healthcare teams can tweak medication plans to enhance balance and reduce side effects. Key points for adjusting medications include:
- Reducing Medication Dosages: Lowering doses to lessen side effects while keeping symptoms in check.
- Changing Medication Timing: Adjusting when to take medications to work better with DBS.
- Switching Medications: Trying different medications that might work better with DBS.
Always have a healthcare expert guide medication changes to ensure safety and effectiveness.
Emerging Complementary Approaches
New methods are being explored to boost balance for DBS patients. These include:
- Virtual Reality Therapy: Using virtual reality to challenge balance and improve mobility.
- Exergaming: Playing video games that require physical activity to enhance balance and coordination.
- Non-Invasive Brain Stimulation: Techniques like TMS or tDCS that might add to DBS benefits.
Though still in research, these methods could offer new ways to improve balance and life quality for DBS patients.
Conclusion: Weighing the Evidence on DBS for Balance
We’ve looked into how Deep Brain Stimulation (DBS) affects balance. We’ve seen studies and research that show DBS can help with balance issues. This is true for conditions like Parkinson’s disease and essential tremor.
The success of DBS for balance depends on a few things. These include the area of the brain targeted, who gets the treatment, and how it’s set up after surgery. The subthalamic nucleus (STN) and globus pallidus interna (GPi) are often chosen for DBS. But, how well it works for balance can vary.
Knowing about DBS for balance helps doctors choose the best treatment for patients. DBS is a good option for balance issues, but it works best when chosen carefully. Each patient needs a treatment plan that’s just right for them.
FAQ
What is Deep Brain Stimulation (DBS) and how does it work?
Deep Brain Stimulation (DBS) is a surgery that implants electrodes in the brain. It helps control abnormal brain activity. It treats conditions like Parkinson’s disease and essential tremor.
How does DBS surgery impact balance in patients with movement disorders?
DBS’s effect on balance varies. It depends on the person, their condition, and the brain area targeted. Some see better balance, while others might not notice a change or could see it worsen.
What are the common balance issues associated with Parkinson’s disease?
Parkinson’s disease often causes problems with balance and walking. It can lead to a higher risk of falls.
Can DBS improve gait and mobility in patients with neurological disorders?
Yes, DBS can help with walking speed and stride length in some. But results vary based on the individual and their condition.
What are the different DBS targets used for balance enhancement?
The Subthalamic Nucleus (STN) and Globus Pallidus Interna (GPi) are common targets for balance. New targets are also being looked into.
How is DBS programming adjusted for balance-specific considerations?
Adjusting DBS for balance involves fine-tuning settings. This might include changing electrode placement, pulse width, and frequency.
Who are ideal candidates for DBS to improve balance?
Good candidates have balance issues that don’t respond to medication. They should have significant mobility problems and a condition that DBS can help with, like Parkinson’s disease.
Are there any limitations to DBS in treating balance problems?
Yes, DBS might not work for all balance issues. Some may experience balance problems or other side effects. It’s not for everyone, especially those with certain health conditions.
Can DBS be combined with other therapies to optimize balance?
Yes, combining DBS with physical therapy and medication can improve balance. New methods, like non-invasive brain stimulation, are also being explored.
What are the potential long-term effects of DBS on postural stability?
DBS can lead to long-term balance improvements in some. But outcomes depend on individual factors and the condition being treated.
How does the DBS surgical procedure impact balance immediately after surgery?
Post-surgery, balance effects can vary. Some might see balance worsen temporarily, while others might see improvements.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/38608807/