Last Updated on December 2, 2025 by Bilal Hasdemir
Deep brain stimulation (DBS) has changed lives for over 40,000 people worldwide. They suffer from Parkinson’s disease and essential tremor. This shows how much DBS has impacted lives, growing from its early days.
DBS has come a long way since the 20th century. It’s now a key treatment for many neurological conditions. DBS uses a device like a pacemaker to send electrical signals to the brain. This helps those with movement disorders find relief.
The journey of DBS shows the power of medical innovation. It’s a story of how we’ve worked to help those with neurological issues. As we look back, it’s clear DBS is a vital part of today’s neurological treatments.
Key Takeaways
- DBS has treated over 40,000 people worldwide for Parkinson’s disease and essential tremor.
- The therapy originated in the early 20th century.
- DBS involves a pacemaker-like device delivering electrical impulses to specific brain areas.
- It is a crucial treatment for various neurological conditions.
- DBS has evolved significantly over the years.
The Origins of Neurostimulation
a high-contrast, close-up shot of a human brain, with glowing neural networks and pulsing electrical impulses flowing through its intricate structure. The brain is illuminated from above by a soft, directional light, casting dramatic shadows and highlights that accentuate the organic complexity of the cerebral cortex. The background is dark and hazy, creating a sense of depth and mystery, with subtle hints of medical equipment or laboratory apparatus visible in the periphery. The overall mood is one of scientific wonder and the boundless potential of neurotechnology, capturing the essence of the "Origins of Neurostimulation."
Neurostimulation is a key part of today’s brain treatments. It started with early electrical experiments. Ancient Greeks and Egyptians used electrical discharges to heal.
Early Electrical Stimulation Experiments
Early electrical experiments were vital in neurostimulation. Scientists tested how electricity affects the body. This led to big steps forward.
Luigi Rolando and Gustav Fritsch were leaders in this field. They studied the brain’s electrical responses in the 19th century. Their findings helped create today’s neurostimulation treatments, like Deep Brain Stimulation (DBS).
Pioneering Brain Research in the 19th Century
The 19th century was a breakthrough time for brain studies. Scientists like Luigi Rolando and Gustav Fritsch made big discoveries. They explored the brain’s electrical side.
Their work helped us understand the brain better. It also set the stage for DBS and other treatments. Their research is still important today as we delve deeper into brain science.
The Precursors to Modern Deep Brain Stimulation
A sterile surgical theater bathed in cool, directional lighting. A patient’s head is securely fixed in a specialized frame, exposing the scalp. A neurosurgeon, clad in scrubs and a surgical mask, carefully maneuvers a precision instrument towards the patient’s skull. The foreground is dominated by the intricate, high-tech equipment required for this delicate stereotactic procedure, while the background features the blurred silhouettes of assistants and medical staff. The atmosphere is one of intense focus and meticulous attention to detail, as the team works to map and target specific regions deep within the brain.
Modern deep brain stimulation (DBS) has roots in earlier surgeries. Stereotactic surgery and ablative procedures were key steps. They helped create the advanced DBS methods we use today.
Stereotactic Surgery Development
In the mid-20th century, stereotactic surgery became crucial. It allowed neurosurgeons to operate with more precision. The invention of stereotactic frames was a major breakthrough, enabling accurate targeting of brain areas.
The 1940s and 1950s saw the introduction of these frames. They changed brain surgery by allowing for precise lesions. This was especially helpful in treating movement disorders. The precision of stereotactic surgery was vital for future treatments.
Early Ablative Procedures
Ablative procedures were among the first surgeries for neurological disorders. They involved creating lesions in the brain. These procedures were used to treat Parkinson’s disease and other movement disorders.
The table below highlights early ablative procedures and their link to modern DBS:
Procedure | Purpose | Outcome |
Thalamotomy | Treat tremors and movement disorders | Variable success rates; sometimes resulted in significant side effects |
Pallidotomy | Reduce symptoms of Parkinson’s disease | Improved motor function in some patients; however, outcomes were not consistent |
Early ablative procedures were sometimes effective but had their drawbacks. DBS was developed to address these issues. It offers a more reversible and adjustable treatment option.
Looking back, the history of DBS shows how important stereotactic surgery and ablative procedures were. They not only led to DBS but also greatly helped us understand and treat neurological disorders.
The Birth of Deep Brain Stimulation in the 1960s
A medical operating room in the 1960s, featuring a patient undergoing deep brain stimulation surgery. The surgeons, dressed in sterile attire, are carefully manipulating a metal device implanted deep within the patient’s brain. The room is dimly lit, with a sense of clinical precision and concentration. Diagnostic monitors and medical equipment surround the operating table, casting a glow on the faces of the medical team as they meticulously perform the delicate procedure. The atmosphere is one of scientific exploration, as this revolutionary technique was just beginning to emerge as a treatment for neurological disorders.
The 1960s were a key time for deep brain stimulation (DBS). It moved from being tested to being used in real treatments. This decade saw big steps forward in how we stimulate the brain, setting the stage for today’s DBS therapy.
First Clinical Applications
In the 1960s, DBS was first used on humans. This was thanks to earlier research and the invention of the first human stereotactic frame by Ernst Spiegel and Henry Wycis in 1947. This tool helped doctors target brain areas more accurately, making DBS a real treatment option.
The first treatments aimed at different neurological problems, like movement disorders. Scientists were looking into how DBS could change brain activity. This brought new hope to those with conditions that didn’t respond to other treatments.
Key Pioneers and Their Contributions
Jose Delgado and Natalia Bekthereva were among the first to make a big impact on DBS. Delgado worked on brain stimulation methods, while Bekthereva studied how DBS helped humans. Their work was crucial for moving DBS forward.
Their efforts led to important breakthroughs:
- Improvements in electrode design and how they’re implanted
- Exploring different brain spots for different conditions
- Learning about DBS’s benefits and possible side effects
These pioneers greatly increased our knowledge of the brain. They also opened the door for DBS to treat many neurological and psychiatric issues today.
Technological Advancements in the 1970s
A technological laboratory filled with intricate medical equipment and machinery, illuminated by soft, directional lighting that casts dramatic shadows. In the foreground, a sleek, state-of-the-art deep brain stimulation device stands prominently, its metallic components and complex circuitry visible. In the middle ground, researchers in white coats examine data on holographic displays, their expressions focused and intent. The background features banks of computer monitors, gleaming medical instruments, and a sense of cutting-edge innovation. The overall atmosphere is one of scientific advancement, precision, and the evolution of DBS technology in the 1970s.
The 1970s were key for DBS, with big steps in hardware and surgery. We saw big leaps in neurotechnology. These changes made DBS better and safer.
Hardware Developments
New devices like implantable pulse generators were big for DBS. They let doctors control the therapy better. This made DBS more effective.
Improved Surgical Techniques
The 1970s also brought better surgical techniques. This made DBS safer and more precise. It opened up DBS for more conditions.
These changes helped DBS grow. They made the procedure safer and more precise. This opened up DBS for treating many neurological disorders.
The 1980s: Expanding Applications of DBS
Detailed cross-sectional diagram of deep brain stimulation target areas, illuminated with precise surgical lighting. Meticulously rendered neuroanatomical structures, including the thalamus, subthalamic nucleus, and globus pallidus, depicted in shades of gray against a clean, minimalist background. Crisp, high-resolution imagery showcases the precise anatomical landmarks essential for accurate DBS electrode placement, reflecting the advancements in neurosurgical techniques during the 1980s. A clinically informative illustration that conveys the expanding applications of this transformative therapeutic approach.
The 1980s were a key time for DBS. This decade saw the exploration of new brain areas for treatment. It was a crucial period for understanding DBS’s full potential in treating various neurological conditions.
New Target Areas in the Brain
In the 1980s, researchers found new targets for DBS. They looked at the subthalamic nucleus for treating Parkinson’s disease and other movement disorders. This area showed great promise in managing symptoms.
Growing Clinical Evidence
DBS kept evolving, and more evidence supported its use. Studies during this time gave insights into DBS’s benefits and side effects. This knowledge helped shape DBS therapy for the future.
Condition | Target Area | Clinical Outcomes |
Parkinson’s Disease | Subthalamic Nucleus | Significant improvement in motor symptoms |
Essential Tremor | Ventral Intermediate Nucleus | Effective tremor control |
Dystonia | Globus Pallidus Internus | Improved muscle tone and reduced spasms |
The 1980s were pivotal for DBS. The evidence gathered helped expand DBS’s uses. It also encouraged more research into its effects and mechanisms.
FDA Approval and Mainstream Adoption in the 1990s
A high-resolution, photorealistic image of a medical device receiving FDA approval in the 1990s. The foreground depicts a silver, sleek deep brain stimulation device, its intricate electrodes and wiring visible. In the middle ground, a panel of doctors and scientists in white coats examine the device, expressions focused and intent. The background showcases an FDA logo and the American flag, suggesting the formal, institutional setting of an official approval process. Warm, directional lighting casts dramatic shadows, conveying the gravity and significance of this milestone in the history of medical technology.
In the 1990s, Deep Brain Stimulation (DBS) became a common treatment for neurological disorders. This was thanks to FDA approval and important regulatory steps. More clinical trials also helped prove DBS’s value for treating various conditions.
Regulatory Milestones
The 1990s were key for DBS. It got FDA approval for treating essential tremor in 1997 and Parkinson’s disease in 2002. These approvals made DBS more accepted by doctors and patients.
The approval process was strict. It included:
- Reviewing all clinical trial data
- Checking if DBS devices were safe and worked well
- Getting approval for specific uses, like for essential tremor
Increased Clinical Trials
As DBS technology improved, more trials were done. These trials were important for:
- Learning more about how DBS works
- Finding new uses for DBS
- Improving who gets DBS
The 1990s were a turning point for DBS. It became a widely accepted treatment. The decade’s regulatory steps and trials set the stage for DBS’s future.
Deep Brain Stimulation for Parkinson’s Disease
A detailed, high-resolution medical illustration depicting deep brain stimulation for the treatment of Parkinson’s disease. The foreground showcases the surgical implantation of the stimulation electrodes deep within the brain, with precise anatomical structures visible. The middle ground features a cross-section of the brain, illustrating the placement of the electrodes and the electrical impulses they emit. The background depicts the external neurostimulator device connected to the implanted electrodes via discreet wiring, all rendered in a clean, technical style with muted colors. The overall scene conveys the complex, delicate nature of this therapeutic intervention in a realistic, informative manner.
Deep brain stimulation (DBS) is a key treatment for Parkinson’s disease symptoms that don’t respond to medication. We’ll look at how DBS works for Parkinson’s, its results, and who can get it.
Mechanism of Action
DBS uses a device called a “brain pacemaker” or “neurostimulator.” It sends electrical signals to parts of the brain. This helps with movement and mental health issues. The exact way it works is complex and involves changing brain circuits.
Clinical Outcomes and Patient Selection
Studies show DBS can greatly improve symptoms like tremors and slow movement in Parkinson’s patients. It can really improve a patient’s quality of life quality. Choosing the right patients is key.
Doctors look at a patient’s history, symptoms, and past treatments. A team of doctors is needed to decide if DBS is right for someone.
Beyond Parkinson’s: Other Applications of DBS
Deep brain stimulation (DBS) is now used for many neurological disorders, not just Parkinson’s disease. It shows great promise in treating other conditions too. This makes DBS a versatile treatment option.
Essential Tremor Treatment
DBS is very effective in treating essential tremor. This condition causes shaking, usually in the hands. Studies have shown that DBS can greatly reduce this shaking.
It works by targeting specific brain areas. This helps control abnormal brain activity. As a result, DBS improves function and reduces disability in essential tremor patients.
Dystonia Management
Dystonia, a disorder of involuntary muscle contractions, can also be treated with DBS. Clinical trials have found that DBS can lessen dystonia symptoms. This improves motor function and overall well-being.
The globus pallidus internus is often targeted in dystonia treatment. DBS helps control abnormal neural activity here. This reduces the symptoms of dystonia, making patients more mobile and comfortable.
Emerging Neurological Applications
DBS is also being studied for other neurological disorders. Research is looking into its use for epilepsy, Tourette syndrome, and psychiatric disorders. These areas are still experimental but hold great promise.
As we learn more about DBS, its uses will likely grow. This offers new hope for patients with previously untreatable conditions.
Psychiatric Applications of Deep Brain Stimulation
Neurotechnology has led to new uses for Deep Brain Stimulation (DBS). Now, it’s being looked at for treating psychiatric illnesses. This is a big change from its traditional use in neurological conditions.
Treatment-Resistant Depression
DBS is being studied for Treatment-Resistant Depression (TRD). TRD is hard to treat and leaves patients with few options. Researchers think DBS might help by targeting brain areas that control mood.
How DBS works on depression is still a mystery. But early studies suggest it could help. It might change brain circuits to reduce depression in those who haven’t responded to other treatments.
Obsessive-Compulsive Disorder
DBS is also being tested for Obsessive-Compulsive Disorder (OCD). OCD makes people have unwanted thoughts and do compulsive actions. For those with severe OCD, DBS might offer a new hope.
DBS targets specific brain areas, like the anterior limb of the internal capsule. This can lessen OCD symptoms. Studies and trials have shown DBS can improve life quality for these patients.
DBS is showing great promise for treating mental health issues. More research and evidence are needed to fully understand its role in psychiatric care.
The Science Behind Deep Brain Stimulation
Understanding DBS is key to seeing its role in modern medicine. Deep brain stimulation (DBS) is a complex treatment. It works by changing how our brain’s circuits work to help us feel better.
Neural Circuitry and Neuromodulation
DBS therapy targets specific brain areas to help with various conditions. The brain’s circuits for movement, thinking, and feelings are complex. By focusing on certain parts, DBS can modulate pathological neural activity. This helps reduce symptoms of Parkinson’s disease, essential tremor, and dystonia.
Neuromodulation is how DBS affects the brain. It changes how brain cells work through electrical stimulation. This can alter how neurons fire and release chemicals, affecting brain circuits.
Proposed Mechanisms of Therapeutic Effect
The ways DBS helps us are still being studied. But, it’s thought to mimic the effects of lesioning by stopping bad brain activity. This can make brain circuits work normally again, which is thought to be why DBS helps.
There are a few theories on how DBS works. These include depolarizing neurons, modulating brain waves, and changing neurotransmitter release. It’s likely that DBS uses a mix of these methods to help.
Modern DBS Systems and Technology
DBS systems have seen big improvements, making them more effective and safe. Today’s DBS systems have several parts that work together. They provide precise control over brain signals.
Components of Current DBS Systems
Modern DBS systems include implantable pulse generators (IPGs), leads, and extensions. The implantable pulse generator is a power source in the chest. It controls the therapy. The lead is a thin wire in the brain with electrodes for stimulation. The extension connects the lead to the IPG.
Advancements in Electrode Design
New electrode designs have made DBS therapy better. These designs allow for more precise and flexible treatment. Clinicians can now customize therapy for each patient, leading to better results.
Battery and Programming Innovations
Battery technology has improved a lot, with longer-lasting and rechargeable IPGs. New programming options let doctors make adjustments on the fly. This makes therapy more comfortable for patients and reduces the need for frequent changes.
DBS technology is entering a new phase. Ongoing research aims to make therapy even better, safer, and more comfortable for patients.
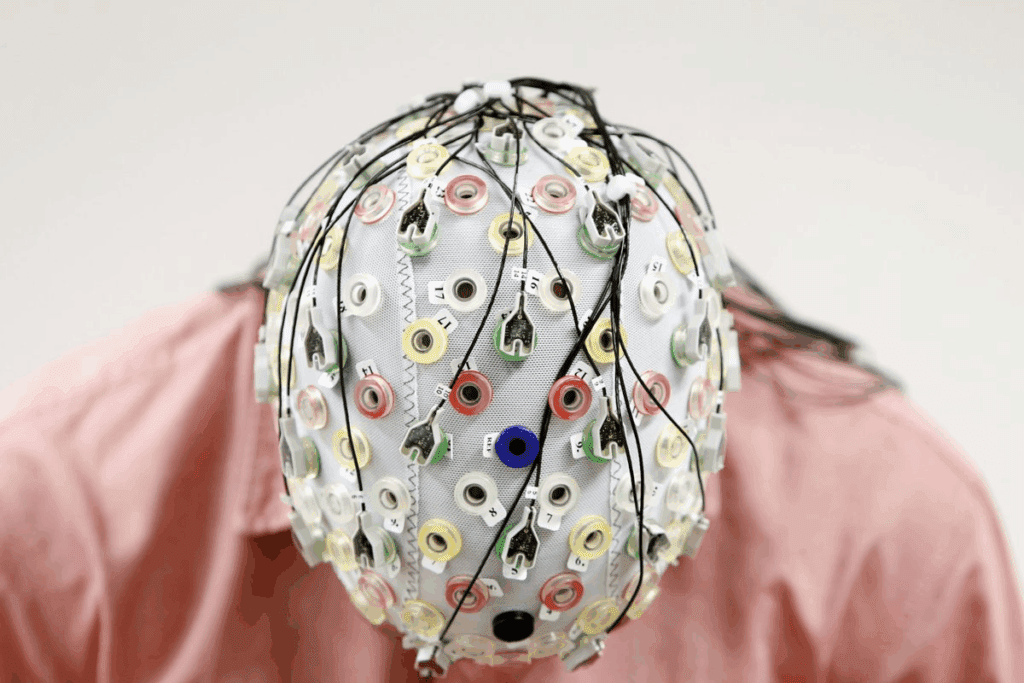
The DBS Surgical Procedure Today
Deep brain stimulation surgery is a detailed process. It needs careful planning and precise execution. The surgery involves placing electrodes in the brain. These electrodes are then linked to a pulse generator, usually hidden under the skin near the collarbone.
Patient Preparation and Selection
Before DBS surgery, patients go through a detailed evaluation. This includes looking at their medical history, doing neurological tests, and using MRI or CT scans. We also check their overall health and any surgery risks.
Choosing the right patient is key for DBS success. The best candidates are those who haven’t gotten better with other treatments or have had bad side effects. Our team talks with patients to see if DBS is the best choice for them.
Implantation Techniques
The DBS surgery has several important steps. First, the patient gets local anesthesia, and a special frame is put on their head. This helps guide the surgical tools. Then, we use advanced imaging to find the exact brain area to target.
The electrodes are placed carefully to avoid harming nearby brain tissue. We plan and execute this step with great care to get the best placement. The pulse generator is then put in the chest, and the electrodes are connected to it with a wire.
Post-Operative Care and Programming
After surgery, patients are watched for any complications. We manage side effects and make sure the DBS system works right.
Programming the DBS device is a key part of treatment. We adjust the device settings with patients to get the best results. This means fine-tuning the settings to control symptoms and improve quality of life.
We schedule follow-up visits to check on patients and adjust the DBS device if needed. Our team is dedicated to helping patients get the most from their DBS therapy.
Challenges and Limitations of Deep Brain Stimulation
Deep Brain Stimulation is a major breakthrough in treating neurological conditions. Yet, it comes with its own set of challenges. These issues affect how well DBS works and who can get it.
Side Effects and Complications
DBS can lead to side effects and complications. These might include hardware problems like broken leads or faulty devices. There are also neurological side effects like changes in thinking, mood, or speech.
There’s also a risk of infection, like with any surgery. To lower these risks, it’s key to choose the right patients carefully. Newer DBS technologies aim to reduce these problems.
Patient Selection Difficulties
Finding the right patients for DBS is hard. Doctors must check the patient’s condition, health, and if they’ll likely benefit. Complex diagnostic criteria and a team of experts make this task even harder.
Also, how patients react to DBS can vary a lot. This makes it tough to guess how well it will work. Research on better diagnostic tools is underway to help choose patients better.
In summary, Deep Brain Stimulation is a powerful treatment but has its challenges. By understanding these, we can make DBS therapy better for everyone.
The Future of Deep Brain Stimulation
The future of deep brain stimulation looks bright. It promises to improve neurotechnology and help patients more. New technologies and techniques are being developed, set to change the field.
Next-Generation Devices
New DBS devices are being made to work better and feel more comfortable for patients. These improvements include:
- Enhanced battery life: Longer battery life means less need for replacements, cutting down on surgeries.
- Smarter stimulation: New algorithms allow for more precise and flexible stimulation, aiming for better results.
- Miniaturization: Smaller devices can make patients feel less burdened and look better.
Closed-Loop Systems
Closed-loop DBS systems are a big step forward. They adjust in real-time based on the patient’s brain activity. This technology could:
- Make stimulation more effective by adjusting it on the fly.
- Lessen side effects by adapting to the patient’s changing needs.
- Save battery life by only using energy when needed.
Expanding Indications
As we learn more about DBS, it’s being considered for more conditions. New uses include:
- Treatment-resistant depression: DBS is being looked at as a possible treatment for severe depression that doesn’t respond to other treatments.
- Obsessive-compulsive disorder: Studies are exploring if DBS can help with severe OCD.
- Other neurological disorders: DBS is being studied for conditions like epilepsy, Tourette’s syndrome, and Alzheimer’s disease.
Deep brain stimulation will remain crucial for treating complex neurological disorders. Ongoing research and new technologies are key to unlocking DBS’s full potential.
Conclusion: The Evolution and Impact of DBS Therapy
Deep brain stimulation (DBS) has grown a lot since it started. It’s now a key treatment for many neurological problems. We’ve looked at how DBS has changed from its early days to being a common therapy today.
DBS has made a big difference in treating neurological disorders. It has helped many patients with Parkinson’s disease, essential tremor, dystonia, and more. As we keep improving in treating the brain, DBS stays a leading therapy.
DBS technology has gotten better, with new designs, surgical methods, and who gets treated. These changes have made DBS more effective for brain disorders. With ongoing research, we’ll see even more improvements in DBS therapy, helping more patients.
The future of DBS is bright, with new devices and systems coming. It’s important to keep watching how DBS works and make it even better. This will help it reach its full potential in treating the brain.
FAQ
What is deep brain stimulation (DBS) and how does it work?
Deep brain stimulation (DBS) is a treatment that uses a device like a pacemaker. It sends electrical impulses to the brain. This helps manage symptoms of conditions like Parkinson’s disease and essential tremor.
What are the origins of deep brain stimulation?
The idea of using electricity to stimulate the brain has been around for a long time. The modern version of DBS started in the 1940s and 1950s. The first uses of DBS in patients were in the 1960s.
What conditions is DBS used to treat?
DBS helps with Parkinson’s disease, essential tremor, and dystonia. It’s also being studied for treating depression and obsessive-compulsive disorder.
How has DBS technology evolved over the years?
DBS technology has improved a lot. New devices and better batteries have made it more precise. This has opened up more ways to use DBS to help patients.
What are the potential side effects and complications of DBS?
DBS is usually safe, but side effects can happen. These include infections, problems with the device, and changes in mood or thinking. Choosing the right patients and watching them closely helps avoid these issues.
How is DBS surgery performed, and what is the recovery process like?
DBS surgery is done under anesthesia. It requires careful targeting of brain areas. After surgery, the device is programmed to manage symptoms. Most people can get back to normal in a few weeks.
What is the future of DBS, and what advancements can we expect?
DBS is getting even better. New devices and research are on the horizon. These advancements will make DBS more effective and help more people.
Is DBS a reversible treatment, and can it be adjusted or turned off?
Yes, DBS can be adjusted or turned off. The device can be programmed to manage symptoms. This flexibility is important for patients.
What are the benefits of DBS for patients with Parkinson’s disease?
DBS greatly improves motor control for Parkinson’s patients. It can also reduce the need for medication. This improves their quality of life.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41582-018-0128-2