Getting a cancer diagnosis can be scary and confusing. It’s important to know the terms doctors use. Carcinoma in situ, or stage 0 cancer, is the very first stage of cancer. It means the abnormal cells haven’t spread yet.
The word “in situ” comes from Latin, meaning “in its original place.” This is a non-invasive condition. It’s usually 100 percent curable if caught early. We stress how vital early detection is for a full recovery.
Key Takeaways
- Carcinoma in situ is the earliest stage of cancer, classified as stage 0.
- It is a non-invasive condition where abnormal cells have not spread.
- Early detection of carcinoma in situ is key for effective treatment.
- The condition is typically 100 percent curable if identified early.
- Understanding cancer definitions helps patients make better choices.
The Definition and Meaning of Carcinoma in Situ
The term carcinoma in situ comes from Latin, meaning “cancer in its original place.” This is key to understanding how early cancer starts. It shows that carcinoma in situ is a cancer that hasn’t spread to other tissues yet.
Etymology and Origin of the Term “In Situ”
The word “in situ” comes from Latin, meaning “in its original place.” This is important because it shows carcinoma in situ is a cancer that stays in one place. It hasn’t spread to other parts of the body. Knowing where the term comes from helps us understand why it’s not invasive.
How Carcinoma in Situ Differs from Normal Cells
Carcinoma in situ cells grow differently than normal cells. Normal cells grow, divide, and die in a regular way. But carcinoma in situ cells grow in abnormal patterns. They are stuck in the epithelial layer and haven’t broken through the basement membrane.
These cells look and divide differently than normal cells. This is why finding the difference between them is so important. It helps doctors catch and treat carcinoma in situ early.
Stage 0 Cancer Classification
Carcinoma in situ is called stage 0 cancer. This means it’s not invasive and hasn’t spread. This is different from stages 1 through 4, where cancer has invaded or spread.
Being classified as stage 0 cancer shows it can be treated well. It also shows why finding it early is so important. Treating it before it becomes invasive can greatly improve patient outcomes.
Types of Carcinoma in Situ
It’s important to know about the different types of carcinoma in situ. This knowledge helps doctors create better treatment plans. Carcinoma in situ means abnormal cell growth that hasn’t spread to other tissues yet.
Ductal Carcinoma in Situ (DCIS)
Ductal carcinoma in situ (DCIS) is a non-invasive breast cancer. It happens when abnormal cells stay in the milk ducts. It’s seen as a warning sign because it could turn into invasive cancer if not treated. Early detection with mammograms has greatly helped manage DCIS.
Lobular Carcinoma in Situ (LCIS)
Lobular carcinoma in situ (LCIS) starts in the breast’s lobules. It’s not a true cancer but raises the risk of invasive breast cancer. People with LCIS are more likely to get cancer in either breast. Regular check-ups and monitoring are key for those with LCIS.
Cervical Carcinoma in Situ
Cervical carcinoma in situ means abnormal cells only on the cervix’s surface. It’s caught through Pap smears and is a step before invasive cervical cancer. Getting vaccinated against HPV can lower the risk of cervical carcinoma in situ.
Other Common Types
There are other types of carcinoma in situ, like in the bladder, lung, and skin. Each has its own traits and treatment plans. Doctors need to understand these conditions well to give the right care.
How to Define Carcinoma in Situ in Medical Terms
To define carcinoma in situ, we need to know its unique cell features. These are different from those of invasive cancer. We will see how doctors diagnose it and what they look for under the microscope.
Cellular Characteristics
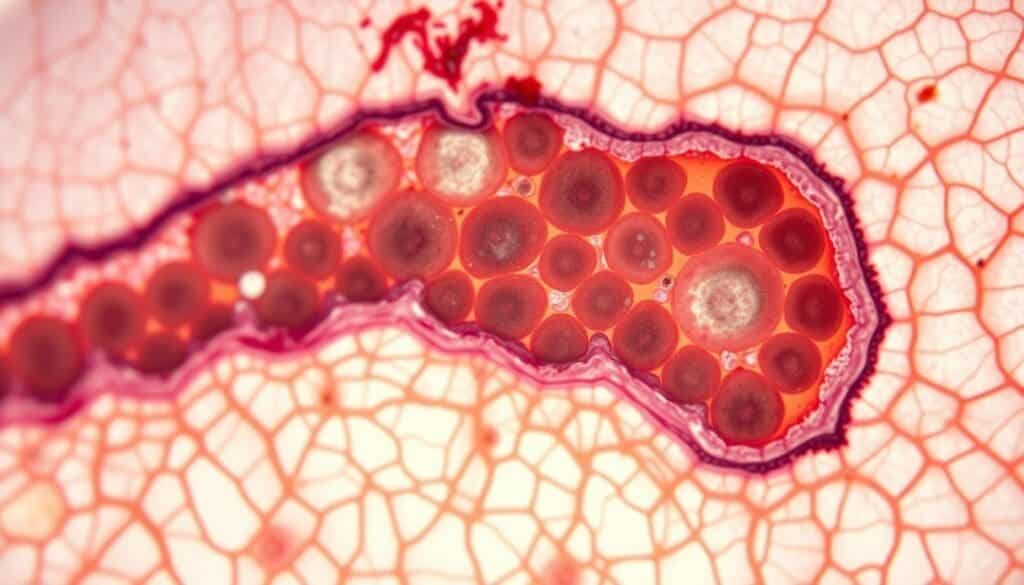
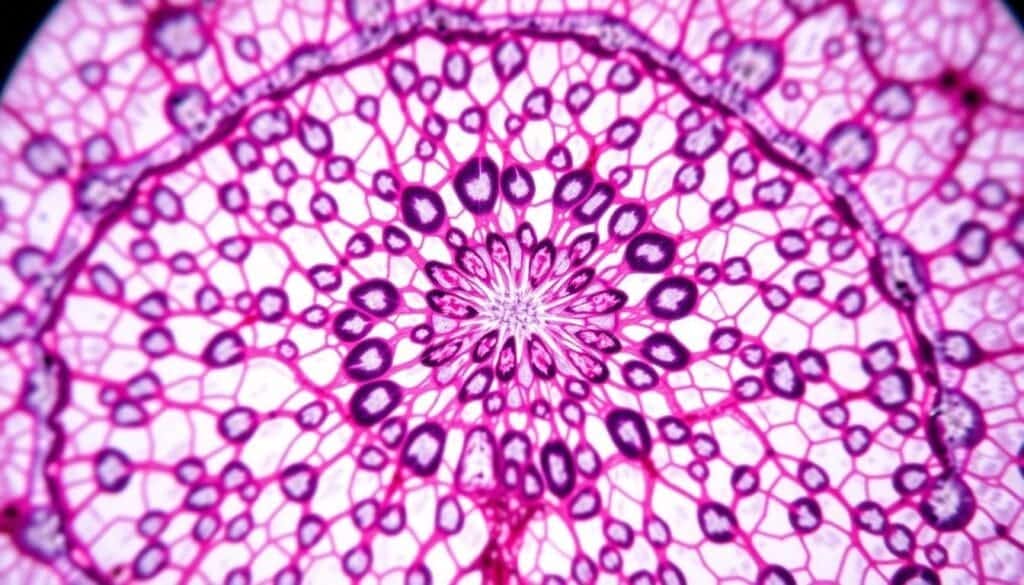
Carcinoma in situ cells look odd under the microscope but stay in the epithelial layer. They are different from normal cells in size, shape, and how they stain. Their nuclei are bigger and more irregular, and they have more DNA, making them darker under certain stains.
These cell traits are key for diagnosis. Doctors look for cells that don’t follow normal patterns. They also check for signs of fast cell division.
Histological Features
The histological features of carcinoma in situ are also vital. It’s defined by malignant cells stuck in the epithelial layer without breaking the basement membrane. Doctors make this diagnosis by looking at cells under the microscope.
Looking at tissue samples helps doctors understand the disease’s extent and risk. They check for signs of abnormal growth and cell changes. This helps them tell carcinoma in situ apart from benign conditions and invasive cancer.
Knowing the histological features of carcinoma in situ is key for treatment. It helps doctors decide on the best treatment, like surgery, watching the condition, or other options.
Carcinoma in Situ vs. Invasive Carcinoma
Understanding the difference between carcinoma in situ and invasive carcinoma is key. Carcinoma in situ is an early stage where abnormal cells are present but haven’t spread. Invasive carcinoma, on the other hand, has spread beyond its original location and can move to other parts of the body.
Key Differences in Cell Behavior
The main difference between these two types of cancer is how the cells behave. In carcinoma in situ, cells are stuck in the epithelial layer and haven’t crossed the basement membrane. Invasive carcinoma cells, though, have broken through the basement membrane and are moving into the surrounding tissue, showing they are more aggressive.
Invasive carcinoma cells are more mobile and can spread to other parts of the body. This change in behavior means the cancer is more serious and needs stronger treatments.
Progression from In Situ to Invasive Cancer
Not every carcinoma in situ turns into invasive cancer, but some do. The chance of this happening depends on the type of cancer, genetic changes, and environmental factors. Knowing these factors helps in managing carcinoma in situ and stopping it from becoming invasive.
Scientists are studying the changes in cells and genes that happen when cancer moves from in situ to invasive. They hope to find markers that can tell us which cancers will spread, so we can act early.
Metastatic Carcinoma Comparison
Metastatic carcinoma is a more advanced stage where cancer cells have moved to other organs. While invasive carcinoma is aggressive and can spread, not all of it has spread at diagnosis.
Looking at carcinoma in situ, invasive carcinoma, and metastatic carcinoma shows how cancer progresses. Knowing these differences helps doctors plan the best treatments and improve patient care.
Epidemiology and Risk Factors
Exploring the epidemiology of carcinoma in situ reveals key information. We learn about its incidence, prevalence, and risk factors. This knowledge is vital for creating effective prevention and treatment plans.
Incidence and Prevalence
Carcinoma in situ is a major health issue because it can turn into invasive cancer. About 20 to 25 percent of breast cancer cases are ductal carcinoma in situ (DCIS). The U.S. sees around 59,080 new DCIS cases each year. The rise in DCIS cases is mainly due to better screening methods.
Lobular carcinoma in situ (LCIS) is less common but risky. Women with LCIS face a 25% to 30% chance of getting breast cancer. This is higher than the 13% risk for all women. This shows why monitoring and follow-up care are key for LCIS patients.
Demographic Patterns
Demographic patterns in carcinoma in situ vary by type and location. DCIS often affects women over 50, making regular mammograms important for them. LCIS, on the other hand, can hit younger women and is often found by chance during biopsies.
Ethnic and racial differences also affect carcinoma in situ rates. Research shows that DCIS rates differ among ethnic groups, with some groups facing higher risks.
Genetic and Environmental Risk Factors
Genetic and environmental factors both raise the risk of carcinoma in situ. Mutations in BRCA1 and BRCA2 genes significantly increase breast cancer risk, including DCIS and LCIS. Family history also plays a big role, with a first-degree relative with breast cancer increasing one’s risk.
Environmental and lifestyle factors, like hormonal influences and reproductive history, also impact risk. For example, early menarche, late menopause, and hormone replacement therapy can raise breast cancer risk.
| Risk Factor | Description | Impact on Risk |
| Genetic Mutations (BRCA1, BRCA2) | Inherited mutations that affect DNA repair | Significantly increased risk |
| Family History | Having a first-degree relative with breast cancer | Increased risk |
| Hormonal Influences | Early menarche, late menopause, hormone replacement therapy | Increased risk |
| Radiation Exposure | Exposure to ionizing radiation, specially at a young age | Increased risk |
“The identification of risk factors for carcinoma in situ is critical for developing targeted prevention strategies and early intervention.”
— Medical Expert, Breast Cancer Specialist
Understanding the epidemiology and risk factors of carcinoma in situ is key to better patient outcomes. By identifying high-risk individuals and using screening and preventive measures, we can lower invasive cancer rates.
Diagnosis of Carcinoma in Situ
Diagnosing carcinoma in situ requires several steps. These include screening and diagnostic tests. Getting the diagnosis right is key for good treatment and outcomes.
Screening Methods
Screening is important for catching carcinoma in situ early. Mammography helps find ductal carcinoma in situ (DCIS). Pap smears are used for cervical carcinoma in situ. The right screening method depends on the type and location of the carcinoma in situ.
Mammography has greatly helped in finding DCIS early. A medical expert said, “Mammography screening has changed how we find breast cancer, including carcinoma in situ.”
“Early detection through screening is key to managing carcinoma in situ effectively.”
Biopsy Procedures
A biopsy is needed to confirm carcinoma in situ. It involves taking tissue from the area in question for a closer look. The tissue is then checked for signs of carcinoma in situ.
Imaging Techniques
Imaging also plays a role in diagnosis. Techniques like ultrasound, MRI, and CT scans are used. They help find the location of the carcinoma in situ.
Molecular and Genetic Testing
Molecular and genetic testing offer more insights. They help identify genetic markers linked to carcinoma in situ. This information guides treatment.
For instance, genetic tests can spot BRCA1 and BRCA2 mutations. These are linked to a higher risk of breast cancer, including DCIS.
Treatment Options for Carcinoma in Situ
Carcinoma in situ treatment aims to stop cancer from spreading. We’ll look at different ways to treat it, like surgery, radiation, medicine, and watching it closely.
Surgical Approaches
Surgery is a common way to treat carcinoma in situ. You might have lumpectomy or mastectomy. The choice depends on where the cancer is and what you prefer.
Radiation Therapy
After surgery, radiation might be suggested. It helps kill any cancer cells left behind. This is good for lowering the chance of cancer coming back.
Medication and Hormonal Treatments
For some types of carcinoma in situ, like DCIS, hormone treatments can help. Medicines like tamoxifen are used for hormone-positive cases.
Active Surveillance
In some cases, watching the condition closely is advised. This means regular check-ups and tests, but no immediate treatment.
Prevention and Management Strategies
Managing carcinoma in situ requires a mix of lifestyle changes, regular check-ups, and emotional support. This approach helps patients improve their health and lower the chance of cancer spreading.
Lifestyle Modifications
Healthy eating and staying active are key in managing carcinoma in situ. Eating lots of fruits, veggies, and whole grains keeps you healthy. Exercise also boosts your mood and helps manage stress.
Important lifestyle changes include:
- Keeping a healthy weight
- Staying away from tobacco and drinking less alcohol
- Doing regular exercise
- Eating a balanced diet
Follow-up Care and Monitoring
Regular check-ups are vital for keeping an eye on your condition. They help catch any problems early. This care includes:
- Visits to your healthcare provider
- Tests like mammograms or ultrasounds
- Biopsies if needed
Early detection is key for managing the condition well. A good follow-up plan is essential for this.
| Follow-up Procedure | Frequency | Purpose |
| Mammogram | Annually | To monitor for any changes in breast tissue |
| Clinical Breast Exam | Every 6 months | To check for any abnormalities |
Psychological Support
Psychological support is a big part of managing carcinoma in situ. Patients often find help in:
- Counseling or therapy sessions
- Support groups
- Stress management techniques
Emotional support helps patients deal with their diagnosis and treatment. It improves their life quality.
Conclusion
Carcinoma in situ is a key stage in cancer development. It needs quick diagnosis and the right treatment to stop it from becoming invasive cancer. We’ve looked into what it is, its types, how to diagnose it, and treatment options.
This condition is marked by abnormal cell growth that hasn’t spread to nearby tissues. Knowing about carcinoma in situ is key for catching it early and managing it well. This helps lower the chance of it turning into invasive cancer.
By understanding the risks, symptoms, and how to diagnose it, we can help patients better. Our talk has shown how important carcinoma in situ is in fighting cancer. It highlights the need for more research and awareness.
FAQ
What does carcinoma in situ mean?
Carcinoma in situ is an early stage of cancer. It hasn’t spread to other tissues yet. It’s considered stage 0 cancer.
What is the difference between carcinoma in situ and invasive carcinoma?
Carcinoma in situ is non-invasive and stays in one place. Invasive carcinoma spreads to other tissues and can reach other parts of the body.
What are the types of carcinoma in situ?
There are several types, including ductal carcinoma in situ (DCIS), lobular carcinoma in situ (LCIS), and cervical carcinoma in situ.
How is carcinoma in situ diagnosed?
Doctors use screening tests, biopsies, imaging, and genetic tests to find and check how far the cancer has spread.
What are the treatment options for carcinoma in situ?
Treatments include surgery, radiation, medicine, hormonal therapy, and watching the cancer closely. The choice depends on the cancer’s type and where it is.
Can carcinoma in situ be prevented?
Not all cases can be prevented, but healthy habits and avoiding risks may lower the chance of getting it.
What is the significance of early detection of carcinoma in situ?
Finding it early is key. It means doctors can treat it quickly, possibly curing it before it spreads.
How does carcinoma in situ progress to invasive cancer?
If not treated, it can turn into invasive cancer. This happens when cancer cells spread to other tissues and possibly to other parts of the body.
What is the role of genetic and environmental risk factors in carcinoma in situ?
Genetic and environmental factors can lead to carcinoma in situ. Knowing these can help in preventing and catching it early.
What is the importance of follow-up care for carcinoma in situ?
Follow-up care is vital. It helps watch for any signs of cancer coming back or getting worse and deals with treatment side effects.
What does “in situ” mean in the context of cancer?
“In situ” means the cancer cells are in their original place. They haven’t spread to other tissues yet.
Is carcinoma in situ considered cancer?
Yes, it is a type of cancer, stage 0. If not treated, it can become invasive cancer.
References
National Center for Biotechnology Information. (2025). What Is Carcinoma in Situ Understanding Cancer Definitions. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK567766/