Last Updated on October 31, 2025 by
Getting a diagnosis of carcinoma in situ can be scary. But knowing what it is is very important. At places like Liv Hospital, we say carcinoma in situ, or stage 0 cancer, means cells look cancerous under a microscope. Yet, they haven’t spread to other areas. If you want to define in situ cancer, it refers to abnormal cells that remain where they first formed and have not invaded nearby tissues.
Unlike invasive cancer that grows into nearby tissues, carcinoma in situ is an early sign. It shows changes in cells that are stuck in one place. This is a key time for doctors to act and stop the problem before it gets worse.

To get what carcinoma in situ means, we first need to know what “in situ” is. “In situ” comes from Latin and means “in its original place.” This is key in cancer talk because it shows cancer cells are there but haven’t spread.
The word “in situ” is important in cancer because it means the cancer is early and hasn’t spread. This is key for picking the right treatment. Carcinoma in situ is called stage 0 cancer, showing it’s not invasive.
Knowing carcinoma in situ stays in one place shows why catching it early is so important. It’s a chance to stop the cancer before it gets worse.
Stage 0 cancer, or carcinoma in situ, means the cancer cells are stuck in one place. They haven’t spread to other tissues. This stage is a warning sign that cancer could become invasive if not treated.
Diagnosing stage 0 cancer shows how vital screening and early detection are. It lets doctors find cancer when it’s easier to treat and less likely to have spread.
In short, knowing about carcinoma in situ means it’s stage 0 cancer that’s not spreading. This knowledge stresses the need for early detection and the right treatment.
How to Define In Situ Cancer and Its Characteristics

In situ cancer, also known as carcinoma in situ, is a key stage in cancer growth. It happens when abnormal cells stay in their original tissue. We call it in situ cancer when cancerous cells are present but haven’t spread to other areas.
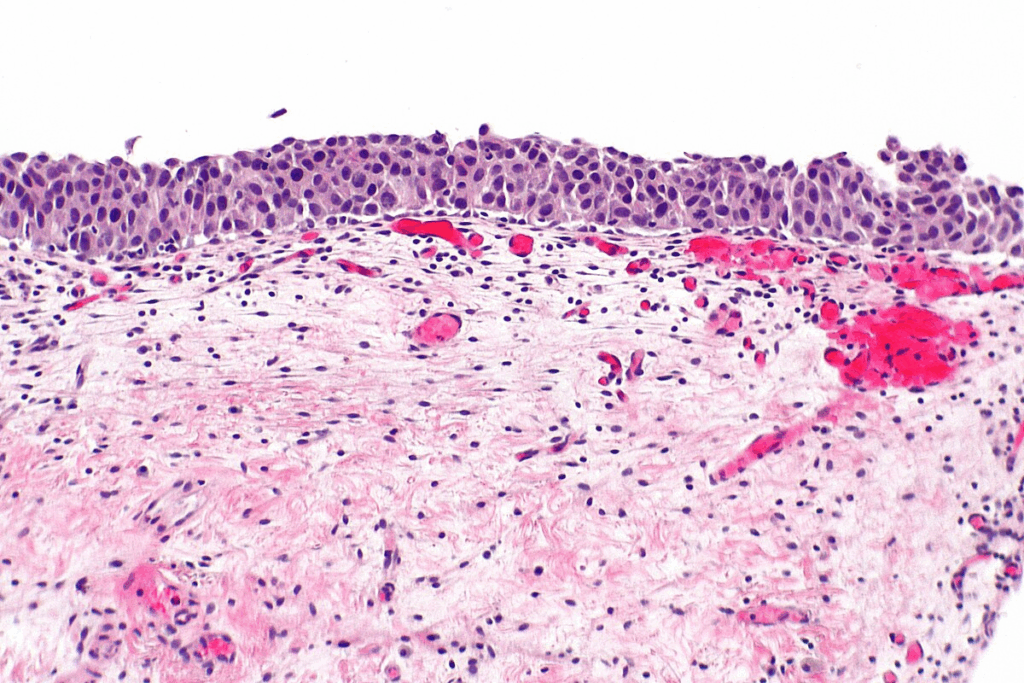
When we look at carcinoma in situ cells under a microscope, they show signs of being cancerous. They have irregular shapes and abnormal nuclei. These signs show they could become cancer, but they’re stuck in their original tissue.
A key trait of carcinoma in situ is that it stays in the tissue where it started. The cancer cells haven’t crossed the basement membrane. This thin layer of tissue keeps them from spreading.
The table below lists the main traits of carcinoma in situ:
| Characteristics | Description |
| Cellular Changes | Cells look cancerous under a microscope, with odd shapes and abnormal nuclei. |
| Containment | Cancer cells stay in their original tissue and haven’t spread. |
| Basement Membrane | The cancer cells haven’t crossed the basement membrane. |
Knowing these traits is key to diagnosing and treating carcinoma in situ right. We’ll keep looking at the differences between carcinoma in situ and invasive cancer in the next parts.
Carcinoma in Situ vs. Invasive Cancer: Key Differences
It’s important to know the difference between carcinoma in situ and invasive cancer for treatment. We’ll look at the main differences between these two conditions. We’ll focus on how they behave and what they mean for patient outcomes.
Carcinoma in situ stays in the tissue where it started, without spreading. Invasive cancer, on the other hand, breaks through its original site. It invades nearby tissues and can spread to other parts of the body. This big difference is key for figuring out the prognosis and treatment.
Carcinoma in situ doesn’t have the power to spread to other places yet. But invasive cancer can spread, making it more serious. This means invasive cancer needs stronger treatments.
The metastatic ability of a cancer is how well it can spread. Invasive cancer, having already spread to nearby tissues, is at high risk of spreading further. This risk is a big deal for figuring out how serious the disease is and what treatment is needed.
The risk of spreading for invasive cancer affects treatment choices and outcomes. Knowing this risk helps doctors plan treatments that target the main tumor and any possible spread sites.
In short, carcinoma in situ and invasive cancer differ in how they behave and spread. Carcinoma in situ stays put and doesn’t spread, while invasive cancer invades and can spread. These differences are key for making treatment plans and predicting patient outcomes.
It’s important to know about the different types of carcinoma in situ. This knowledge helps doctors diagnose and treat the condition better. Carcinoma in situ can happen in many parts of the body. We’ll look at ductal carcinoma in situ (DCIS), cervical carcinoma in situ, and melanoma in situ.
Ductal carcinoma in situ (DCIS) is a type of cancer in the breast. It affects the lining of the milk ducts. The good news is that it’s non-invasive, meaning the cancer cells stay in the ducts.
Doctors often find DCIS during mammograms. They treat it with surgery or radiation. This helps stop the cancer from becoming invasive.
Cervical carcinoma in situ is a precancerous condition on the cervix. It can turn into invasive cancer if not treated. Regular Pap smears are key to catching it early.
“Regular screening for cervical cancer can detect precancerous changes, enabling early treatment and preventing the development of invasive cancer.”
Melanoma in situ is a type of skin cancer. It affects the outermost skin layer. It’s considered an early-stage melanoma but hasn’t spread deeper.
It’s important to watch melanocytic lesions closely. Melanoma in situ can turn into invasive melanoma if not treated right.
There are other types of carcinoma in situ, like lobular carcinoma in situ (LCIS) in the breast and carcinoma in situ of the bladder. Each type has its own features and treatment plans.
| Type of Carcinoma in Situ | Location | Key Characteristics |
| Ductal Carcinoma in Situ (DCIS) | Breast milk ducts | Non-invasive, confined to ducts |
| Cervical Carcinoma in Situ | Cervix | Precancerous cells on cervix surface |
| Melanoma in Situ | Skin (epidermis) | Abnormal melanocytes, non-invasive |
It’s key to know about carcinoma in situ to fight it better. We look at new data to share insights on its spread and trends.
The latest numbers for 2025 show a rise in some carcinoma in situ cases. For example, about 59,080 cases of ductal carcinoma in situ (DCIS) in women’s breasts and 107,240 cases of melanoma in situ are forecasted. These figures stress the need for more research and awareness.
| Type of Carcinoma in Situ | Estimated Cases |
| Ductal Carcinoma in Situ (DCIS) | 59,080 |
| Melanoma in Situ | 107,240 |
Demographics and risk factors are vital in studying carcinoma in situ. Studies show some groups face higher risks due to genes, environment, and lifestyle.
Knowing these risk factors helps us focus our screening and prevention efforts.
Diagnosing carcinoma in situ involves several steps. These steps help doctors find cancer early. This is key to treating it well.
Screening is very important for finding carcinoma in situ early. Mammograms help spot ductal carcinoma in situ (DCIS). Pap smears are used for cervical carcinoma in situ. Regular checks can find cancer before symptoms show up, making treatment better.
The American Cancer Society says early detection is key. Regular screenings can find carcinoma in situ early. This makes it easier to treat than invasive cancer.
After screening shows possible carcinoma in situ, doctors use more tests to confirm it. Biopsy and histopathological examination are the best ways to diagnose it.
| Diagnostic Technique | Accuracy | Application |
| Biopsy | High | Confirms presence of carcinoma in situ |
| Histopathological Examination | High | Provides detailed cellular analysis |
These tests not only confirm the cancer but also tell doctors more about it. This helps decide the best treatment.
We stress how important accurate diagnosis and early detection are. They help manage carcinoma in situ well.
The treatment for carcinoma in situ varies based on several factors. These include the type and location of the cancer. Each patient’s situation is unique, so treatments are tailored to fit their needs.
Surgical excision is a common and effective treatment for carcinoma in situ. The goal is to remove the cancerous cells completely. Surgical options often provide a high success rate, which is important when cancer is detected early.
In some cases, surgical procedures are minimally invasive. This reduces recovery time and scarring. The choice of surgical technique depends on the location and extent of the carcinoma in situ.
Not all cases of carcinoma in situ require surgery. Non-surgical interventions, such as topical treatments, may be recommended. This is often for superficial or sensitive area cancers.
These treatments can manage the condition and prevent invasive cancer. The choice of non-surgical intervention depends on the patient’s health and preferences.
In some instances, watchful waiting is considered a viable approach. This involves regular monitoring with diagnostic tests. It ensures the cancer does not progress.
Watchful waiting is typically reserved for low-risk cases where progression risk is minimal. This approach helps patients avoid or delay more invasive treatments. It helps maintain quality of life.
We work closely with our patients to determine the best treatment plan. We consider all available options and individual circumstances.
To prevent carcinoma in situ, we need to make lifestyle changes and get regular health checks. Knowing the risks and acting early can lower the chance of getting this condition.
Making lifestyle changes is key to stopping carcinoma in situ. Avoiding too much sun is important because UV rays can cause cancer. Eating a healthy diet with lots of fruits, veggies, and whole grains also helps keep you healthy and might lower cancer risk.
Other good changes include not smoking and drinking less alcohol. These steps help prevent carcinoma in situ and improve your overall health.
Regular screenings are vital for catching carcinoma in situ early. Screening tests can spot abnormal cells before they turn into cancer, so we can act fast.
| Screening Type | Frequency | Benefit |
| Mammography | Annual | Early detection of breast abnormalities |
| Pap Smear | Every 3 years | Detection of cervical cell abnormalities |
| Skin Examination | Annual | Identification of suspicious skin lesions |
Understanding carcinoma in situ is key for early detection and treatment. This stage is critical because cancer cells are present but haven’t spread.
We’ve looked at what carcinoma in situ is, its types, how it’s diagnosed, and treatment options. Early detection and treatment can greatly improve health outcomes. Types like ductal carcinoma in situ (DCIS), cervical carcinoma in situ, and melanoma in situ need quick action.
In short, knowing about carcinoma in situ is vital for managing it well. Awareness and regular screening are essential. By understanding this, we can prevent and treat it early, leading to better health.
Regular screening and awareness are vital for managing carcinoma in situ. We stress the importance of staying informed and proactive in health care.
“In situ” is Latin for “in its original place.” It means the cancer cells haven’t moved from where they started.
Carcinoma in situ is when cancer cells are present but haven’t spread. It’s often called stage 0 cancer.
The main difference is how the cancer cells behave. Carcinoma in situ stays in its original place. Invasive cancer spreads beyond its starting point.
There are several types. Ductal carcinoma in situ (DCIS) affects the breast milk ducts. Cervical carcinoma in situ impacts the cervix. Melanoma in situ affects the skin.
Doctors use tests like mammograms and Pap smears for screening. Then, they do biopsies and histopathology to confirm the diagnosis.
Treatment choices depend on the type, location, and what the patient wants. Options include surgery, non-surgical treatments, or watching and waiting.
While it’s not fully preventable, making lifestyle changes and getting regular screenings can lower the risk. It can also improve treatment results.
Finding cancer early through screenings and quick action can greatly improve patient outcomes. It makes treatments more effective.
Stage 0 cancer, or carcinoma in situ, means cancer cells are present but haven’t spread to surrounding tissues.
The spreading ability of invasive cancer greatly affects treatment choices and outcomes. It shows a higher risk of cancer spreading.
National Center for Biotechnology Information. (2025). What Is Carcinoma in Situ and How Does. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7270677
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!