Type 1 and Type 2 diabetes are two different conditions. Type 1 diabetes happens when the immune system attacks the pancreas. This attack stops the pancreas from making insulin.
Type 2 diabetes is different. It’s when the body makes insulin but can’t use it well. Knowing the difference is key to managing and treating these conditions.
Both types affect blood sugar levels. But their causes and how to manage them are different. Understanding these differences helps people deal with their diagnosis and treatment better.
Key Takeaways
- Type 1 diabetes is an autoimmune condition that results in little to no insulin production.
- Type 2 diabetes involves insulin resistance and is influenced by lifestyle factors.
- Understanding the differences between Type 1 and Type 2 diabetes is key for effective management.
- Each condition has its own causes and symptoms, needing different management strategies.
- Getting the right diagnosis is vital for the right treatment and better health outcomes.
Understanding Diabetes: A Brief Overview

Diabetes mellitus is a long-term condition where blood sugar levels are too high. It affects how the body uses glucose, a key energy source. To understand diabetes, we need to know how the body controls blood sugar and the role of insulin.
What Is Diabetes Mellitus?
Diabetes mellitus is not one disease but a group of metabolic disorders. It happens when there’s a problem with insulin production or use. Insulin, made by the pancreas, helps glucose enter cells, lowering blood sugar. Without enough insulin or when it’s not used well, glucose builds up in the blood, causing diabetes.
The Role of Insulin in Blood Sugar Regulation
Insulin is key in controlling blood sugar levels. After eating, insulin helps cells take in glucose for energy or storage. This keeps blood sugar levels healthy. In diabetes, this balance is lost, either because of insulin lack or poor use.
Global Impact and Prevalence
Diabetes is a big health problem worldwide. The International Diabetes Federation says about 463 million adults had diabetes in 2019. This number is expected to grow to 578 million by 2030. Diabetes affects different areas more, due to genetics, environment, and lifestyle.
Region | Diabetes Prevalence (2019) | Projected Prevalence (2030) |
North America | 46.4 million | 51.2 million |
Europe | 59.3 million | 67.7 million |
South-East Asia | 88.6 million | 114.1 million |
Knowing the global impact and prevalence of diabetes is key for public health strategies. We must look at these factors when talking about Type 1 and Type 2 diabetes.
The Fundamental Difference Between Diabetes 1 and Diabetes 2
Type 1 and Type 2 diabetes differ in how they start and how the body handles insulin. Both lead to high blood sugar, but they have different causes and effects on insulin.
Autoimmunity vs. Insulin Resistance
Type 1 diabetes happens when the body’s immune system attacks and destroys insulin-making cells in the pancreas. This means people with Type 1 diabetes need insulin to survive. Type 2 diabetes, on the other hand, is caused by the body’s cells not responding well to insulin. This makes it hard for glucose to get into cells, and the pancreas may not make enough insulin.
Understanding the difference between autoimmunity and insulin resistance is key. Type 1 diabetes is managed by replacing insulin. Type 2 diabetes is managed by improving how well the body uses insulin, and sometimes insulin therapy is needed too.
Prevalence Statistics: 5-10% vs. 90-95%
About 5-10% of diabetes cases are Type 1, affecting many people worldwide. In contrast, Type 2 diabetes makes up 90-95% of cases. These numbers show how different these conditions are and why they need different treatments.
- Type 1 diabetes: 5-10% prevalence
- Type 2 diabetes: 90-95% prevalence
Core Metabolic Distinctions
Type 1 diabetes is an autoimmune condition that leads to no insulin production. Type 2 diabetes is caused by insulin resistance and not enough insulin, often due to being overweight or inactive.
- Type 1 Diabetes: No insulin because of immune system attacks on beta cells.
- Type 2 Diabetes: Insulin resistance and not enough insulin, often from lifestyle choices.
Knowing these differences is important for doctors to create good treatment plans. It also helps patients manage their diabetes better.
Type 1 Diabetes: The Autoimmune Condition
Type 1 diabetes is a complex autoimmune condition. It happens when the immune system attacks the insulin-producing beta cells in the pancreas. This leads to a complete lack of insulin production.
Pathophysiology of Type 1 Diabetes
The pathophysiology of Type 1 diabetes involves genetics and environment. These factors trigger an autoimmune response. This response destroys the pancreatic beta cells, which are key for insulin production.
The loss of these cells makes it hard for the body to control blood glucose levels. This results in high blood sugar, a hallmark of diabetes.
Beta Cell Destruction Process
The destruction of beta cells in Type 1 diabetes is a slow process. It can take years. Autoreactive T cells mistakenly see beta cells as foreign.
This autoimmune destructiongreatly reduces insulin production. Eventually, it leads to Type 1 diabetes.
Is Type 1 Diabetes Hereditary?
Type 1 diabetes has a genetic link, but it’s not just about genes. Environmental factors also trigger the autoimmune response. Having a family history of Type 1 diabetes raises the risk. But it doesn’t mean you’ll definitely get it.
It’s important to understand how genes and environment interact. This knowledge helps in finding ways to prevent and treat Type 1 diabetes.
Type 2 Diabetes: The Insulin Resistance Condition
Type 2 diabetes is a complex condition. It’s caused by the body’s inability to use insulin well. This leads to high blood sugar levels.
How Insulin Resistance Develops
Insulin resistance happens when cells don’t respond well to insulin. This makes it hard for glucose to get into cells. It can be caused by genetics, lifestyle, and environment.
Insulin resistance is a key step towards Type 2 diabetes. Knowing how it starts is important for prevention and management.
Progressive Nature of Type 2 Diabetes
Type 2 diabetes gets worse over time if not managed. The body’s insulin production can decrease as the disease progresses. This makes controlling blood sugar harder.
The disease’s progressive nature shows why early diagnosis and good management are key. They help slow down the disease’s progression.
Pancreatic Beta Cell Dysfunction
Pancreatic beta cell dysfunction is a big part of Type 2 diabetes. As insulin resistance grows, the pancreas makes more insulin. But, the beta cells can get tired and make less insulin over time.
It’s important to understand how insulin resistance and beta cell dysfunction work together. This helps in creating effective treatments for Type 2 diabetes.
Genetic and Environmental Risk Factors
Type 1 and Type 2 diabetes come from a mix of genes and environment. Knowing these factors helps us understand why each type happens.
Hereditary Factors in Type 1 Diabetes
Type 1 diabetes is linked to genes, with some markers raising the risk. Specific human leukocyte antigen (HLA) genes are key. But, genes alone don’t cause it; environment also plays a part.
Studies show viruses can start Type 1 diabetes in people with the right genes. The exact how is being studied, but both genes and environment are involved.
Lifestyle and Genetic Influences in Type 2 Diabetes
Type 2 diabetes comes from genes, lifestyle, and environment. Lifestyle factors like diet and exercise are big risks. Genes also matter, with some groups more at risk.
- Poor diet and lack of exercise lead to insulin resistance.
- Being overweight is a big risk for Type 2 diabetes.
- Genes can affect how well insulin works and is made.
Which Type of Diabetes Are You Born With?
Type 1 diabetes is often linked to genes you’re born with. But, not everyone with these genes gets Type 1. Type 2 diabetes also has a genetic part, but lifestyle choices play a bigger role later in life.
- Type 1 diabetes is present in those with the right genes from birth.
- Environmental factors start the autoimmune response in Type 1 diabetes.
- Type 2 diabetes is more influenced by lifestyle choices.
Knowing how genes and environment work together helps fight both Type 1 and Type 2 diabetes. By understanding these factors, we can improve treatment and prevention.
Age of Onset and Demographic Patterns
Looking at diabetes demographics, we see big differences between Type 1 and Type 2. The age when people get diabetes and who gets it vary a lot.
Typical Age of Diagnosis for Each Type
Type 1 diabetes often starts in kids and young adults, before they turn 20. On the other hand, Type 2 diabetes usually starts in adults, often after 45. But, we’re seeing more Type 2 cases in younger people now.
Type 1 diabetes usually starts early, often during puberty. Type 2 diabetes risk goes up with age, after 45. This is because of insulin resistance and problems with the pancreas.
Changing Demographics in Recent Years
In recent years, the demographics of both Type 1 and Type 2 diabetes have changed. Type 1 diabetes is no longer just for the young. It’s happening more in all age groups. Type 2 diabetes is getting more common in younger people and in different ethnic groups.
The Rise of Type 2 Diabetes in Youth
Type 2 diabetes in kids and teens is a big worry. It’s linked to more obesity, less activity, and bad diets. This change means younger people with Type 2 diabetes might face more health problems over time.
Diabetes Type | Typical Age of Onset | Demographic Characteristics |
Type 1 | Children and young adults | Autoimmune, often lean body mass |
Type 2 | Adults, increasingly in youth | Insulin resistance, often associated with obesity |
It’s key to understand these changes in diabetes demographics. This helps us create better prevention and treatment plans. As diabetes demographics keep changing, healthcare needs to adapt to help all patients.
Recognizing the Symptoms: Type 1 vs. Type 2
It’s important to know the symptoms of Type 1 and Type 2 diabetes. Both types have some similar signs, but they start and show up differently.
Rapid vs. Gradual Symptom Development
Type 1 diabetes symptoms come on quickly, usually in a few weeks. This fast start is because the body attacks the cells that make insulin. Type 2 diabetes symptoms, on the other hand, take years to show up. This slow start is because the body becomes less responsive to insulin.
Type 1 diabetes symptoms are often very severe. People with Type 1 may lose a lot of weight, feel very tired, and even get diabetic ketoacidosis. Type 2 diabetes symptoms are milder and can be hard to notice at first.
Unique Symptom Patterns in Each Type
Both types of diabetes make you thirsty and need to pee more. But Type 1 diabetes has more severe symptoms like losing weight fast and having ketosis. Type 2 diabetes might not show symptoms for a long time or have mild ones that are easy to ignore.
People with Type 2 diabetes might feel tired, see things less clearly, or heal slowly. These signs can be small and take time to show up. It’s important to watch for changes in your body and see a doctor if they don’t go away.
How to Know What Type of Diabetes You Have
Finding out if you have Type 1 or Type 2 diabetes takes a doctor’s help. They look at your age, weight, family history, and if you have certain antibodies. This helps them figure out which type you have.
Tests like blood sugar levels, HbA1c, and antibody tests are key in making a diagnosis. Knowing your diabetes type is important for the right treatment plan.
Diagnostic Approaches and Testing Methods
Getting a correct diabetes diagnosis is key for managing the disease well. We use a mix of doctor’s checks and lab tests to find out if someone has diabetes mellitus.
Blood Tests and Diagnostic Criteria
Blood tests are the main way to find out if someone has diabetes. The tests we use most are:
- Fasting Plasma Glucose (FPG) test: checks blood sugar after not eating for a night.
- Oral Glucose Tolerance Test (OGTT): checks blood sugar after drinking a sweet drink.
- Hemoglobin A1c (A1C) test: shows average blood sugar levels over 2-3 months.
These tests help figure out if someone has diabetes or prediabetes. The rules for diagnosing diabetes are:
Test | Normal | Prediabetes | Diabetes |
FPG | <100 mg/dL | 100-125 mg/dL | ≥126 mg/dL |
OGTT | <140 mg/dL | 140-199 mg/dL | ≥200 mg/dL |
A1C | <5.7% | 5.7-6.4% | ≥6.5% |
Differentiating Between Types During Diagnosis
Telling Type 1 from Type 2 diabetes can be hard. We look at symptoms, medical history, and lab results to make a correct diagnosis.
Antibody Testing for Type 1 Diabetes
Antibody tests help find Type 1 diabetes. Finding certain antibodies shows the body is attacking itself, which is a sign of Type 1 diabetes.
Treatment Strategies: How Management Differs
Diabetes treatment varies greatly between Type 1 and Type 2. This is because each type has its own unique causes. Type 1 diabetes happens when the body can’t make insulin because of an autoimmune attack. Type 2 diabetes is caused by the body not responding well to insulin and not making enough.
Insulin Dependency in Type 1 Diabetes
Type 1 diabetes needs insulin to control blood sugar. People with Type 1 can’t make insulin, so they need to take it. They might use insulin pens or pumps to get the insulin they need.
The amount and timing of insulin are adjusted based on several factors. These include blood sugar levels, what they eat, and how active they are.
Medication Options for Type 2 Diabetes
Type 2 diabetes treatment starts with lifestyle changes. This includes eating right and exercising to improve how well the body uses insulin. If these steps don’t work, doctors might prescribe medications.
Common medications include metformin and sulfonylureas. Metformin helps the body use insulin better. Sulfonylureas make the pancreas produce more insulin. Sometimes, insulin therapy is needed as Type 2 diabetes gets worse.
Lifestyle Modifications for Both Types
Even though treatments differ, lifestyle changes are key for both types. Eating well, staying active, and keeping a healthy weight are important for everyone. These habits help control blood sugar, prevent complications, and improve overall health.
Prevention and Risk Reduction
Type 1 diabetes is a challenge, but Type 2 diabetes can be prevented with lifestyle changes. Knowing the difference is key to effective prevention.
Can Type 1 Diabetes Be Prevented?
Type 1 diabetes is when the body attacks its own insulin-making cells. There’s no known way to stop it yet. Scientists are working hard to find out how to prevent it, but for now, there’s no prevention.
Lifestyle Strategies to Prevent Type 2 Diabetes
Type 2 diabetes can be prevented or delayed with lifestyle changes. Here are some key strategies:
- Maintaining a Healthy Weight: Being overweight increases the risk of Type 2 diabetes. Losing weight and keeping it off can lower this risk.
- Regular Physical Activity: Activities like walking or swimming can improve insulin sensitivity and reduce diabetes risk.
- Balanced Diet: Eating less sugar and saturated fats and more fiber can help manage blood sugar and support health.
These changes not only prevent Type 2 diabetes but also improve overall health.
Prediabetes: The Warning Stage
Prediabetes means blood sugar is higher than normal but not high enough to be diabetes. It’s a sign of increased risk for Type 2 diabetes. People with prediabetes can prevent Type 2 diabetes by making lifestyle changes.
Risk Factor | Description | Prevention Strategy |
Obesity | Being overweight or obese increases the risk of Type 2 diabetes. | Weight loss through diet and exercise |
Physical Inactivity | Lack of regular physical activity contributes to insulin resistance. | Engage in regular physical activity |
Unhealthy Diet | Consuming a diet high in sugars and saturated fats. | Adopt a balanced diet low in sugars and saturated fats |
In conclusion, Type 1 diabetes can’t be prevented yet, but Type 2 diabetes can be prevented or delayed with lifestyle changes. Understanding risk factors and taking action can greatly reduce the risk of Type 2 diabetes.
Living With Diabetes: Daily Management Challenges
Managing diabetes daily is a big task. It’s different for Type 1 and Type 2 diabetes. People with diabetes need to watch their blood sugar and make lifestyle changes. They also use technology to help manage their condition.
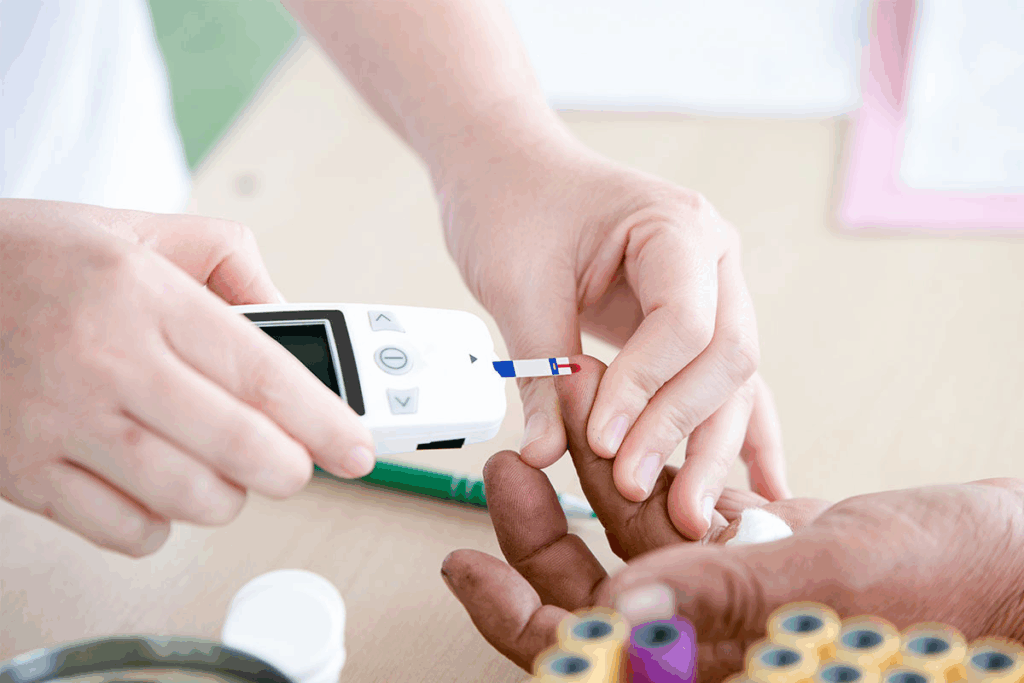
Blood Sugar Monitoring Differences
Checking blood sugar is key for diabetes care. People with Type 1 diabetes check more often because they need insulin. Those with Type 2 might not need to check as much at first, but it can change over time.
Continuous glucose monitoring systems (CGMS) are popular for both types. They give real-time data and trends. This helps people make better care choices.
Technology Advancements in Diabetes Care
Technology has changed diabetes care a lot. Insulin pumps and CGMS are just a few examples. These tools give real-time data and alerts for blood sugar levels.
Mobile apps and online platforms also help. They let people track their blood sugar, medication, and lifestyle. This integrated approach can lead to better health and a better life.
Psychological Impact of Each Type
The mental side of diabetes is important. Both Type 1 and Type 2 can affect your mind. Managing diabetes can cause anxiety and burnout.
Type 1 diabetes can hit young people hard. It can affect their identity and independence. Type 2 diabetes, more common in older adults, can carry a stigma. Support from healthcare providers, family, and peers is key. It helps people deal with diabetes and stay positive.
Conclusion: Living Well With Either Type of Diabetes
It’s key to know the differences between Type 1 and Type 2 diabetes to manage them well. By using the right treatments and making lifestyle changes, people with either type can live well. They can also manage their diabetes effectively.
People with diabetes can have active and happy lives with the right care. We stress the need for a complete diabetes care plan. This includes regular checks, sticking to medication, and making healthy lifestyle choices.
To live well with diabetes, you need a plan that includes medical care, lifestyle changes, and support. Working with healthcare providers and using available resources helps. This way, people with diabetes can get the best health results and enjoy a better life.
FAQ
What is the difference between Type 1 and Type 2 diabetes?
Type 1 diabetes is when your body attacks insulin-making cells. This means you don’t make much insulin. Type 2 diabetes is when your body makes insulin but can’t use it well.
Which type of diabetes are you born with?
Type 1 diabetes often runs in families and can be present at birth. But symptoms usually show up in kids or teens.
How to know what type of diabetes you have?
Doctors use blood tests to find out. These include fasting plasma glucose and A1C tests. Antibody tests can also tell the difference between Type 1 and Type 2.
What is the difference between diabetes 1 and 2 in terms of symptoms?
Type 1 diabetes starts quickly with symptoms. Type 2 diabetes develops slowly over time.
Can Type 1 diabetes be prevented?
No, Type 1 diabetes can’t be prevented. It’s an autoimmune disease.
How does Type 2 diabetes differ from Type 1 diabetes in terms of management?
Type 1 diabetes needs insulin because your body can’t make it. Type 2 diabetes might be managed with diet, exercise, or medication, or insulin.
What are the lifestyle strategies to prevent Type 2 diabetes?
To prevent Type 2 diabetes, stay at a healthy weight, exercise regularly, and eat well.
What is prediabetes, and how is it related to Type 2 diabetes?
Prediabetes means your blood sugar is higher than normal but not high enough to be diabetes. It’s a sign you might get Type 2 diabetes.
How do technology advancements impact diabetes care?
New tech, like continuous glucose monitors, helps manage diabetes better. They make tracking easier and more accurate.
What is the psychological impact of living with diabetes?
Diabetes can affect your mind, causing stress, anxiety, and depression. It’s important to have support and mental health help.
References
National Center for Biotechnology Information. Type 1 vs. Type 2 Diabetes: Key Differences Explained. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5723935/