Last Updated on November 20, 2025 by Ugurkan Demir

Polycythemia is a condition where there’s too many red blood cells. This makes blood thicker and increases the risk of blood clots.
Polycythemia vera (PV) is a rare blood cancer. It happens when the bone marrow makes too many red blood cells, and often too many white blood cells and platelets, due to genetic changes like JAK2. Understanding the difference between polycythemia and polycythemia vera is key, as not all cases of high red blood cell counts are caused by cancer.
It’s important to know the difference between primary and secondary polycythemia. This helps doctors diagnose and treat the condition right. Liv Hospital is known for its top-notch care in blood disorders.
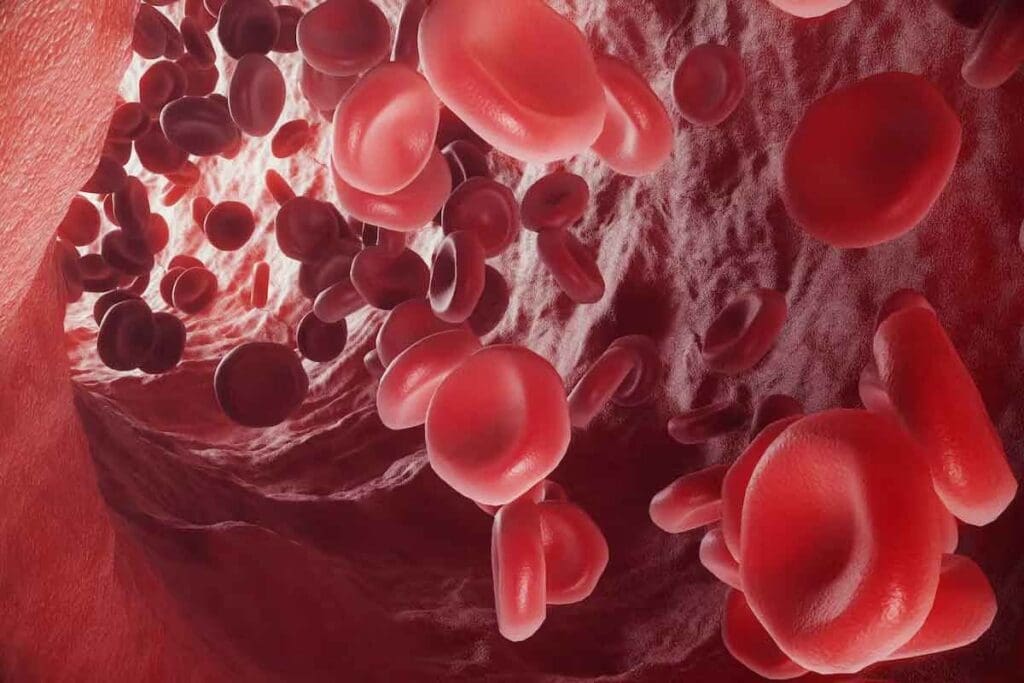
Polycythemia is when there are too many red blood cells, white blood cells, and platelets in the blood. This can happen for two reasons: primary or secondary. It makes the blood thicker, which can cause health problems if not treated.
The blood gets thicker because of more red blood cells. This makes the blood flow slower, leading to circulatory problems. There are two main types: primary polycythemia, linked to polycythemia vera (PV), a rare blood cancer, and secondary polycythemia, caused by outside factors.
The main types of polycythemia are:
Symptoms of polycythemia include:
These symptoms happen because the thick blood can’t flow well. This can cause serious problems if not treated.
Untreated polycythemia can lead to serious issues, such as:
Knowing these risks shows why early diagnosis and treatment are key to managing polycythemia well.

Polycythemia vera and polycythemia are not just different names. They show different ways the body makes blood cells. Polycythemia is when there are more red blood cells in the blood. This can happen for many reasons.
On the other hand, polycythemia vera is a blood cancer. It makes too many blood cells because of a genetic change.
Polycythemia means there are more red blood cells in the blood. It can happen for many reasons, like not enough oxygen or tumors. Secondary polycythemia is when it’s caused by something else.
Symptoms of polycythemia include headaches, dizziness, and feeling tired. If not treated, it can cause blood clots.
Polycythemia vera is a blood cancer. It makes too many red and white blood cells and platelets. This is because of a JAK2 gene mutation in most cases.
This condition needs ongoing care. Symptoms can be similar to polycythemia but also include itching and burning pain in hands and feet.
To tell polycythemia vera apart from polycythemia, look at the cause and symptoms. Here are the main differences:
Knowing these differences is key for the right treatment. Polycythemia vera needs careful treatment because it’s a cancer. Secondary polycythemia is treated by fixing the cause.
Primary polycythemia starts in the bone marrow. Here, problems lead to too many red blood cells. It’s linked to polycythemia vera, where the marrow can’t control blood cell making.
Polycythemia vera is caused by bone marrow problems. These issues make too many red and white blood cells and platelets. The marrow’s failure is key in primary polycythemia.
Key characteristics of intrinsic bone marrow disorders include:
Studies show over 90 percent of polycythemia vera cases have JAK2 mutations. The JAK2 V617F mutation causes too many blood cells. It’s a key sign of polycythemia vera.
JAK2 mutations are vital in diagnosing primary polycythemia. They also help in choosing treatments.
While JAK2 is common, other genes like MPL and CALR can also play a part. These genes have mutations that affect blood cell production.
| Gene | Mutation Type | Frequency in PV |
| JAK2 | V617F | >90% |
| MPL | Various | 5-10% |
| CALR | Various | 5% |
Knowing about these genes is key for diagnosing and treating primary polycythemia. The type of mutation can change how the disease shows up and how it’s treated.
Secondary polycythemia happens when the body reacts to low oxygen or certain diseases. It’s not caused by problems in the bone marrow. Instead, it’s due to external factors.
This condition is different from primary polycythemia vera. It’s not a cancer but a body reaction. Triggers include low oxygen, tumors, and other factors that make the body produce too much erythropoietin.
People with COPD, sleep apnea, or living at high altitudes often get secondary polycythemia. Their bodies make more erythropoietin to fight low oxygen. This leads to more red blood cells.
Smoking also causes low oxygen levels. This increases the risk of secondary polycythemia. Smokers often have higher hematocrit levels because of the oxygen shortage.
Some tumors can cause secondary polycythemia by making erythropoietin. Renal cell carcinoma, hepatocellular carcinoma, and cerebellar hemangioblastoma are examples. These tumors make substances that increase red blood cells.
The tumors produce erythropoietin or other factors. This leads to more red blood cells in the body.
Other causes include conditions that cause tissue hypoxia or wrong erythropoietin levels. For example, heart diseases or high altitudes can lead to it. Genetic conditions that affect hemoglobin also play a role.
| Causes | Mechanisms | Characteristics |
| Chronic Low Oxygen States | Increased erythropoietin production due to hypoxia | Seen in COPD, sleep apnea, high altitudes |
| Tumor-Induced | Erythropoietin production by tumors | Associated with renal cell carcinoma, hepatocellular carcinoma |
| Other Causes | Tissue hypoxia or inappropriate erythropoietin secretion | Includes cardiovascular diseases, genetic conditions affecting hemoglobin |
It’s important to know the difference between polycythemia vera and secondary polycythemia. Both involve more red blood cells, but they have different causes and treatments. This knowledge helps doctors diagnose and treat patients better.
Polycythemia vera (PV) is a disease where bone marrow makes too many blood cells. Secondary polycythemia happens when the body reacts to low oxygen or tumors. It mainly makes more red blood cells.
PV is caused by problems in the bone marrow, like the JAK2 V617F mutation. Secondary polycythemia is triggered by outside factors.
Both PV and secondary polycythemia can cause headaches, dizziness, and fatigue. But PV patients often have more problems like blood clots and big spleens.
Lab tests can tell PV and secondary polycythemia apart. Here are the main differences:
| Laboratory Finding | Polycythemia Vera | Secondary Polycythemia |
| JAK2 Mutation | Present in majority of cases | Typically absent |
| Erythropoietin Level | Low | Normal or elevated |
| White Blood Cell Count | Often elevated | Usually normal |
PV and secondary polycythemia have different long-term outlooks. PV can lead to serious blood diseases and blood clots. Secondary polycythemia usually has a better outlook if the cause is treated.
PV patients need careful monitoring and treatment. This includes blood removal, aspirin, and sometimes medicines to control the disease.
In summary, knowing the difference between PV and secondary polycythemia is key. It helps doctors give the right treatment and improve patient outcomes.
Diagnosing polycythemia requires a detailed approach. This includes blood tests, genetic testing, and examining the bone marrow. Getting the diagnosis right is key to choosing the right treatment and managing the condition well.
Blood tests are vital in diagnosing polycythemia. They look for high levels of hemoglobin, hematocrit, or red blood cells. These tests help tell if it’s a primary or secondary polycythemia.
The complete blood count (CBC) is a basic test that checks different parts of the blood. In polycythemia, the CBC shows more red blood cells. Other tests, like serum erythropoietin (EPO) levels, help figure out the cause.
Genetic testing is key in diagnosing polycythemia vera (PV). The JAK2 V617F mutation is found in most PV cases. This mutation is a key marker for PV, helping to tell it apart from secondary polycythemia.
The JAK2 mutation is found in 96–99% of PV cases, as per the WHO classification. Testing for this mutation is vital for accurate diagnosis and planning treatment.
A bone marrow biopsy is a critical tool, mainly for diagnosing polycythemia vera. It looks at the bone marrow to check its cell count and for any oddities.
Other tests, like imaging studies, might be used to check for secondary causes of polycythemia. These could include tumors or chronic hypoxia. These tests help doctors fully understand the patient’s situation.
Diagnosing polycythemia can be tricky because symptoms and lab results can look similar across different types. Doctors must carefully review test results to find the real cause of polycythemia.
A detailed diagnostic process is needed to tell primary from secondary polycythemia. It also helps find any underlying conditions that might be causing the disorder.
Choosing the right treatment depends on whether you have primary or secondary polycythemia. Both involve more red blood cells, but the reasons and how to treat them are different.
Primary polycythemia, like polycythemia vera (PV), needs a detailed treatment plan. Phlebotomy is key for PV. It helps keep the hematocrit (HCT) under 45% to lower the risk of blood clots.
Patients with PV might also take low-dose aspirin to cut down on blood clot risks. For high-risk patients, treatments to reduce red blood cell production might be used.
For secondary polycythemia, the goal is to fix the underlying cause. For example, treating chronic hypoxia can help balance red blood cell levels.
If it’s caused by living at high altitudes or certain medicines, changing these factors can help manage the condition.
New treatments for polycythemia are being researched. JAK inhibitors are being looked at for PV. They might be an option for those who can’t use traditional treatments.
Future research might lead to more targeted treatments. This could improve care for both primary and secondary polycythemia patients.
People with polycythemia need to live a healthy lifestyle and follow their treatment plans. This helps them keep a good quality of life. Liv Hospital stresses the need for the latest medical care and care that focuses on the patient.
Managing polycythemia well means taking a few steps. Eating right and exercising regularly can help lessen symptoms and boost health.
It’s key to keep an eye on blood counts and other health signs. Patients should work with their doctors to change their treatment plans if needed.
To avoid problems linked to polycythemia, stay proactive about your health. Don’t smoke, drink plenty of water, and know the risks of blood clots.
Knowing when to get medical help is important. Signs like tiredness, bone pain, or infections need quick action.
People with polycythemia vera should watch for signs of getting worse. This includes a higher white blood cell count or new bone pain.
Getting support from doctors, family, and groups is key in managing polycythemia. Educational materials and counseling help deal with the emotional side of the condition.
Liv Hospital aims to offer full care. This includes the newest treatments and support services.
It’s important to know the difference between polycythemia and polycythemia vera. Polycythemia vera is a rare blood cancer that needs proper care. This care helps manage symptoms and prevent complications.
Polycythemia vera causes too many red and white blood cells and platelets. It’s often linked to the JAK2 V617F mutation. On the other hand, secondary polycythemia happens due to low oxygen or tumors. Knowing the cause helps doctors choose the right treatment.
It offers detailed insights into the condition. Knowing the difference between polycythemia vera and other forms is key for both doctors and patients.
Polycythemia is when you have too many red blood cells in your blood. It can happen for two reasons. Either it’s because of a problem in your bone marrow, or it’s caused by not enough oxygen in your body.
Polycythemia is a broad term for having too many red blood cells. Polycythemia vera, on the other hand, is a specific blood cancer. It makes your bone marrow produce too many red blood cells.
Symptoms include headaches, dizziness, feeling tired, and shortness of breath. If not treated, it can cause serious problems like blood clots, stroke, and heart attacks.
Primary polycythemia is often due to problems in the bone marrow. JAK2 mutations are a common cause. Other genetic issues can also play a role.
Secondary polycythemia can be caused by not enough oxygen in the body. This can happen with diseases like COPD. Tumors that make erythropoietin can also trigger it.
Doctors use blood tests to check red blood cell counts. They also do genetic tests for JAK2 mutations. A bone marrow biopsy is used to look at the bone marrow’s cells.
Treatment depends on the type of polycythemia. For primary and polycythemia vera, treatments include phlebotomy and medicines. Secondary polycythemia is treated by fixing the underlying cause.
Patients can manage it by drinking plenty of water and avoiding extreme temperatures. They should also keep an eye on their condition. Regular doctor visits are key to prevent problems and adjust treatments.
If not treated, polycythemia can lead to serious issues. These include blood clots, stroke, heart attack, and damage to organs because of thick blood.
Yes, new treatments are being researched. These include targeted therapies and drugs that change the immune system. They aim to help patients with polycythemia, like those with polycythemia vera.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!