Last Updated on December 1, 2025 by Bilal Hasdemir
Traumatic brain injuries (TBI) are a major cause of disability and death globally. Diffuse axonal injury (DAI) is one of the most severe types. It happens when the brain faces rotational forces, leading to widespread damage.A diffuse axonal injury (DAI) is one of the most severe TBIs. Learn the critical facts about this devastating brain injury and its prognosis.
DAI damages axons, which are key for brain function. This injury can cause big problems with thinking, feeling, and physical abilities. Knowing about DAI helps us find better ways to treat it.
Key Takeaways
- Diffuse axonal injury is a severe form of traumatic brain injury.
- It occurs due to rotational forces causing axonal damage.
- DAI can lead to widespread brain damage and significant impairments.
- Understanding DAI is key for effective treatment.
- DAI diagnosis and treatment need a detailed approach.
Understanding traumatic brain injury involves examining its definition and the mechanisms behind it.

Understanding traumatic brain injury involves examining its definition and the mechanisms behind it. TBI is a serious condition caused by outside forces hitting the brain. This can lead to different levels of damage.
Definition and Basic Mechanisms
Traumatic brain injury happens when something outside the body affects the brain. This can change how the brain works or show signs of damage. The first hit can damage brain parts right away. Then, other changes can make things worse.
The first injury can cause skull fractures, contusions, and lacerations. These can hurt the brain right away and later on. They affect brain function in many ways.
Primary vs. Secondary Brain Injury
TBI has two main types of injury. Primary brain injury is the damage from the first hit. This can include things like fractures, bleeding, and direct harm to brain tissue.
Secondary brain injury happens later, after the first hit. It can come from things like not enough oxygen, low blood pressure, swelling, and high pressure in the skull. Knowing the difference helps doctors find better ways to treat TBI.
The mix of primary and secondary injuries shows why TBI needs careful treatment. Doctors aim to fix the first damage and manage the later changes. This helps lessen the injury’s effects.
Classification of TBI Severity
TBI severity is usually measured with the Glasgow Coma Scale (GCS). This scale helps doctors check how well a person is awake and thinking.
The GCS looks at eye opening, talking, and moving. Scores range from 3 to 15.
Mild TBI
Mild TBI has a GCS score of 14-15. People with mild TBI might feel confused or lose consciousness briefly. But, most symptoms go away in a few weeks.
Moderate TBI
Moderate TBI scores 9-13 on the GCS. Those with moderate TBI face bigger challenges in thinking and moving. They need more medical help and might need special treatments.
Severe TBI
Severe TBI scores 3-8 on the GCS. People with severe TBI need quick and serious medical care. They might face lasting problems with thinking, feeling, and moving.
| TBI Severity | GCS Score | Characteristics |
| Mild | 14-15 | Brief loss of consciousness, confusion, symptoms resolve within weeks |
| Moderate | 9-13 | More pronounced cognitive and physical symptoms, requires closer medical attention |
| Severe | 3-8 | Significant brain damage, potentially long-term impairments, requires intensive care |
Knowing how severe a TBI is helps doctors decide the right treatment. It also helps predict how well a patient will recover.
The Glasgow Coma Scale in Severe TBI Assessment
The Glasgow Coma Scale (GCS) is a key tool in medical settings for TBI evaluation. It offers a standardized way to check a patient’s consciousness level. This is vital for understanding brain injury severity and making treatment plans.
Scoring System Explained
The GCS scoring system looks at three main areas: eye opening, verbal response, and motor response. Each area gets a score, and adding these scores gives a total GCS score from 3 to 15.
- Eye Opening: Scores range from 1 (no eye opening) to 4 (spontaneous eye opening).
- Verbal Response: Scores range from 1 (no verbal response) to 5 (oriented and converses).
- Motor Response: Scores range from 1 (no motor response) to 6 (obeys commands).
Interpretation of Scores for Severe TBI
The total GCS score helps classify TBI severity. Scores are divided into mild TBI (GCS 14-15), moderate TBI (GCS 9-13), and severe TBI (GCS 3-8). Patients with a score of 8 or less are usually considered to have severe TBI. They might be comatose and need urgent, intense medical care.
Knowing the GCS score is essential for doctors to talk clearly about a patient’s status. It helps in making treatment choices and predicting patient outcomes.
Diffuse Axonal Injury
Understanding traumatic brain injury involves examining its definition and the mechanisms behind it.
Definition and Pathophysiology
DAI damages axons in the brain due to rotational forces during a traumatic event. This injury stops the brain from working right by harming the axons. Axons are important for sending signals across the brain.
The injury in DAI comes from complex mechanisms. Rotational forces make the brain move inside the skull. This causes shearing forces that hurt the axons. The damage can lead to axons breaking and then degenerating over time.
Mechanisms of Axonal Damage
The ways axons get damaged in DAI are complex. Rotational forces are key in starting the injury. These forces cause:
- Axonal stretching and tearing
- Disruption of axonal transport
- Activation of various pathological processes that contribute to axonal degeneration
DAI’s axonal damage doesn’t stop after the initial injury. It keeps getting worse due to secondary injury mechanisms like inflammation and oxidative stress.
Microscopic vs. Macroscopic Damage
DAI can cause both microscopic and macroscopic damage to the brain. Microscopic damage is not seen with the naked eye and needs a microscope to spot. It affects many parts of the brain.
Macroscopic damage can be seen with the naked eye and includes lesions in areas like the corpus callosum and brainstem. The severity of DAI depends on both microscopic and macroscopic damage.
Grades of Diffuse Axonal Injury
Diffuse axonal injury (DAI) is divided into different grades. These grades show how severe the brain injury is. This helps doctors understand the extent of the damage.
Mild Diffuse Axonal Injury: Grade I
Grade I DAI is the mildest form. It has minimal axonal damage. Symptoms are often mild, like slight memory problems and physical issues.
People with Grade I DAI usually do well with the right treatment. They have a good chance of recovery.
Moderate Diffuse Axonal Injury: Grade II
Grade II DAI means more damage. Symptoms are clearer, like trouble concentrating and memory loss. Patients might also feel mood swings.
Dealing with Grade II DAI needs a strong rehab plan. It helps with both mental and physical challenges.
Severe Diffuse Axonal Injury: Grade III
Grade III DAI has the most damage. It causes big problems with thinking, moving, and emotions. Patients need a lot of care and may face a tough recovery.
The outlook for recovery is not always good. It depends on the injury’s severity and the treatment’s success.
DAI grading is key for doctors to choose the right treatment. It helps predict how well a patient will do. Knowing the differences in grades helps tailor care to each person. This improves their life quality after a brain injury.
Other Types of Severe Traumatic Brain Injuries
Severe traumatic brain injuries include penetrating brain trauma, severe contusions, and fatal intracranial hemorrhages. These injuries can severely harm the brain and overall health.
Penetrating Brain Trauma
Penetrating brain trauma happens when an object goes through the skull and hits the brain. This injury is often caused by fast-moving objects like bullets or sharp objects like knives. The damage’s severity depends on the object’s speed, its path, and the brain areas it hits.
Penetrating brain trauma can cause serious brain damage, like cuts and bleeding. Treating this injury requires quick medical help, often surgery to remove the object and fix damaged areas.
Severe Contusions
Severe contusions are bruises on the brain caused by a hard hit to the head. These injuries can cause bleeding in the brain or around it, leading to swelling and high pressure inside the skull.
Managing severe contusions means watching the brain’s pressure, controlling seizures, and sometimes surgery to relieve pressure or fix blood vessels.
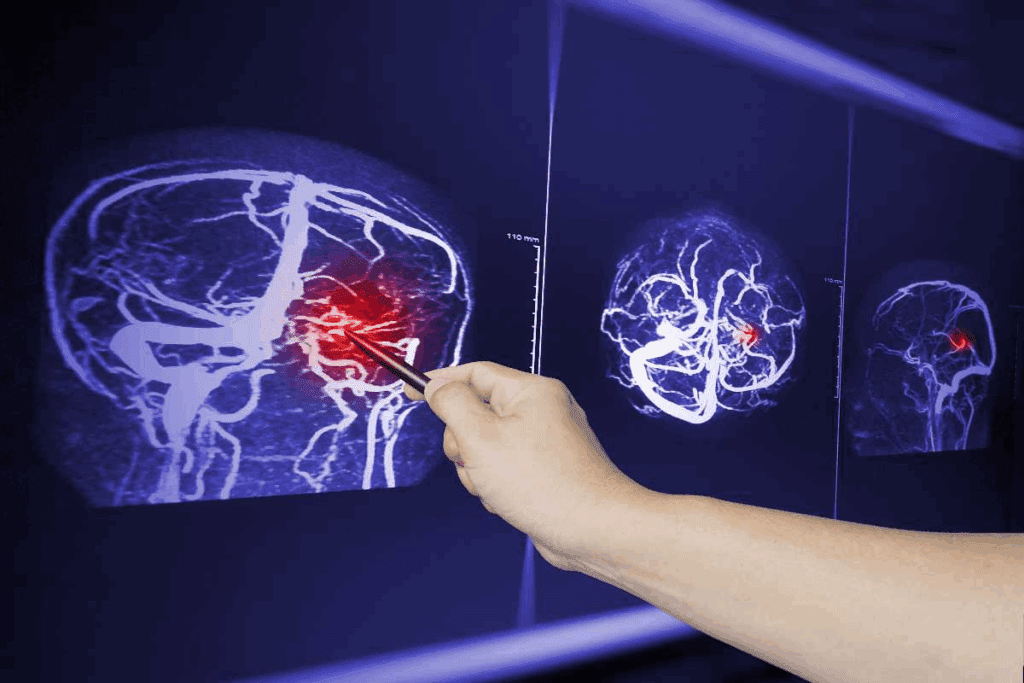
Intracranial Hemorrhages
Intracranial hemorrhages are bleeds inside the skull, which can be deadly. There are different types, like epidural, subdural, and subarachnoid hemorrhages, each with its own effects.
The severity and outcome of intracranial hemorrhages depend on where the bleed is, how much blood there is, and how fast it’s bleeding. Quick diagnosis and treatment, often surgery, are key to preventing more brain damage.
| Type of Injury | Description | Common Causes | Typical Management |
| Penetrating Brain Trauma | Object pierces the skull and damages the brain | Gunshot wounds, stabbings | Surgical removal of object, repair of damaged tissue |
| Severe Contusions | Bruising of brain tissue | Severe head trauma | Monitoring ICP, seizure control, possible surgery |
| Intracranial Hemorrhages | Bleeding within the skull | Trauma, vascular malformations | Surgery to evacuate hematoma, manage pressure |
Brainstem Injuries and Their Consequences
It’s important to know about the brainstem’s role in our body. This helps us understand how injuries affect us.
Anatomy of the Brainstem
The brainstem links the cerebrum to the spinal cord. It has three main parts: the midbrain, pons, and medulla oblongata. It controls vital functions like breathing, heart rate, and blood pressure.
The brainstem has many parts that help signals move between the brain and body. Damage here can cause big neurological impairment.
Impact on Vital Functions
Brainstem injuries can harm vital functions. This can lead to breathing problems, heart issues, and more. The damage’s impact depends on where and how much the injury is.
- Respiratory failure from damage to the medulla oblongata or pons.
- Heart problems from injury to brainstem’s heart centers.
- Changes in consciousness and mental status from damage to the reticular activating system.
Brainstem Reflexes and Prognostic Value
Brainstem reflexes show how well the brainstem is working. They are important for predicting how a patient will do. These reflexes include:
- Pupillary light reflex.
- Corneal reflex.
- Oculovestibular reflex.
- Gag reflex.
Knowing if these reflexes are present helps doctors understand the injury’s severity. It also helps predict the patient’s outcome.
In summary, brainstem injuries can be very serious. They affect vital functions and the patient’s future. It’s key to understand the brainstem’s anatomy, how injuries impact it, and the value of reflexes for proper care.
Severe Brain Edema and Increased Intracranial Pressure
Mechanisms of Cerebral Edema
Cerebral edema comes from several causes. These include damage to the blood-brain barrier, inflammation, and cell damage. Damage to the blood-brain barrier lets fluid and proteins leak into the brain, causing swelling. Inflammation and cell damage also add to the swelling by increasing the brain’s volume and fluid.
Consequences of Elevated Pressure
High intracranial pressure from cerebral edema can lead to serious problems. These include brain tissue herniation and even brain death. High pressure can also cut off blood flow to the brain, causing more damage. Monitoring and managing ICP is key in treating severe brain injuries.
High ICP’s effects show why early detection and treatment are so important. To manage ICP, doctors use medical treatments to reduce swelling and surgery to relieve pressure.
- Medical management includes using osmotic diuretics and other drugs to reduce swelling.
- Surgery, like decompressive craniectomy, may be needed to relieve pressure in severe cases.
Knowing how cerebral edema works and its effects is key to finding good treatments for severe brain injuries.
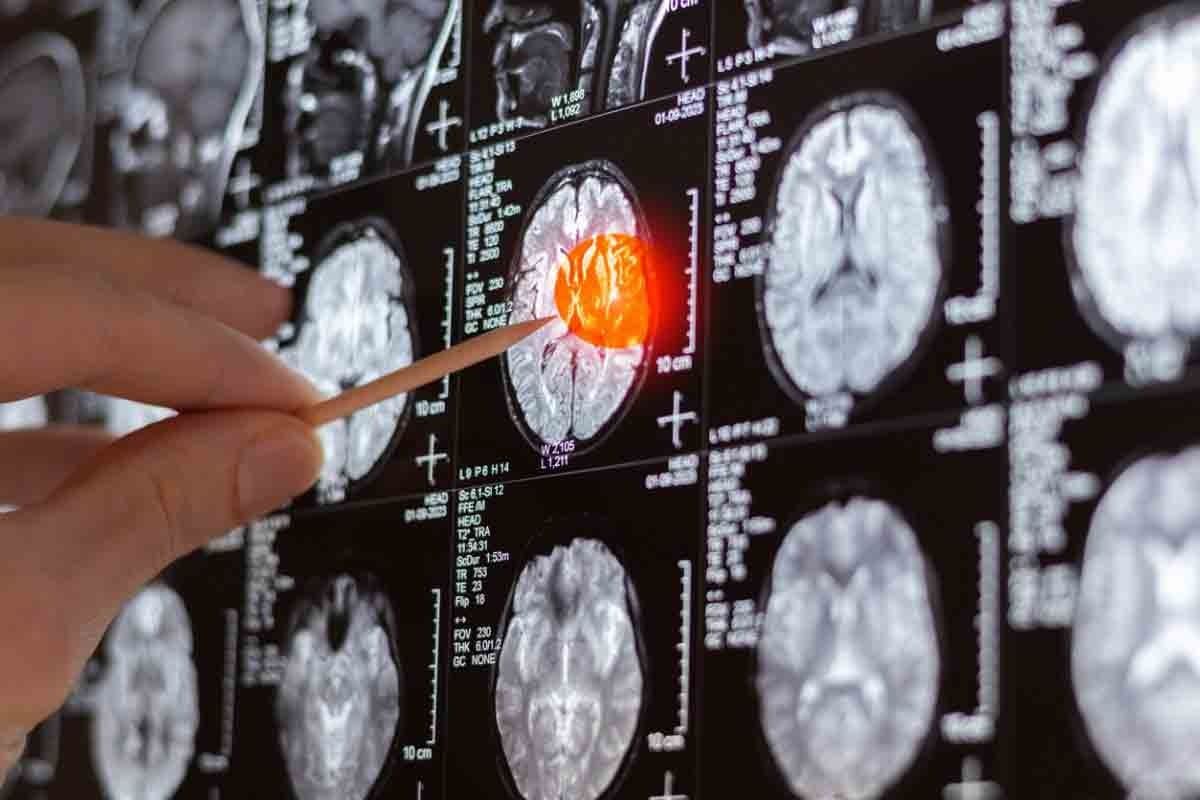
Diagnosis of Severe TBI and Diffuse Axonal Injury
Diagnosing severe traumatic brain injury and diffuse axonal injury requires advanced tools. These include neuroimaging, clinical assessments, and biomarkers. This approach helps understand the injury’s extent and guides treatment.
Neuroimaging Techniques
Neuroimaging is key in diagnosing severe TBI and DAI. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are often used. CT scans are quick and spot hemorrhages and fractures well.
MRI, with its detailed soft tissue view, is great for finding subtle injuries. This includes those from DAI.
Clinical Assessment
Clinical assessment checks the brain’s function and deficits. The Glasgow Coma Scale (GCS) is used to assess and monitor. It shows how severe the TBI is and predicts recovery.
Biomarkers for Severe TBI
Biomarkers are becoming vital in TBI diagnosis and care. Proteins like S100B and GFAP are being studied. They can be found in blood or cerebrospinal fluid, giving insights into injury severity.
Using neuroimaging, clinical checks, and biomarkers offers a full view of severe TBI and DAI. This helps improve patient care and outcomes.
Acute Management of Severe Traumatic Brain Injury
Severe traumatic brain injuries need quick and thorough care. This starts with making sure the patient is stable. Then, the right surgeries and treatments follow. The aim is to prevent more brain damage and help the patient recover as much as possible.
Initial Stabilization
The first step is to make sure the patient’s airway, breathing, and circulation are okay. This is called the ABCs. It’s very important to stop further injury and involves checking the airway, making sure there’s enough oxygen, and keeping blood pressure normal.
Stabilization helps avoid secondary brain injuries. These can happen due to low blood pressure, not enough oxygen, or high pressure inside the skull.
Surgical Interventions
For severe TBI, surgery is often needed. This is true for patients with bleeding in the brain or other serious injuries. Doctors decide if surgery is needed based on what they see and what tests show.
| Surgical Procedure | Indications | Benefits |
| Craniotomy | Removal of hematoma or mass lesion | Reduces intracranial pressure, improves outcomes |
| Decompressive Craniectomy | Refractory intracranial hypertension | Decreases intracranial pressure, potentially improves survival |
Medical Management
Medical care is key in treating severe TBI. It focuses on controlling brain pressure, keeping blood flowing to the brain, and handling other health issues.
- Monitoring and management of ICP and CPP
- Use of sedatives and analgesics to reduce stress and discomfort
- Administration of hyperosmolar therapy to reduce ICP
- Prevention and treatment of seizures and other complications
Good medical management needs a team effort. Neurosurgeons, doctors, nurses, and others work together to care for the patient.
Coma and Vegetative States Following Severe TBI
Severe TBI can lead to coma or vegetative states. These conditions affect a person’s consciousness. They show altered states of awareness and responsiveness.
Defining Different States of Consciousness
“Coma” and “vegetative state” describe different levels of consciousness after severe brain injury. A coma is deep unconsciousness. A person cannot wake up and does not respond to their surroundings.
A vegetative state means wakefulness without awareness. Patients may open their eyes and show reflexes but lack thinking skills.
It’s important to understand these states for patient care and accurate predictions. Moving from coma to vegetative state or other consciousness levels is complex. Careful assessment is needed to find the best treatment.
Prognostic Indicators
Prognostic indicators are key in predicting recovery for those in comatose or vegetative states due to TBI. The injury’s severity, age, and other health conditions matter. Neuroimaging and clinical checks help see brain damage and predict recovery.
For those with severe TBI, knowing the tbi coma prognosis is vital. It helps families and healthcare providers make decisions about care and rehabilitation.
Cognitive impairment often follows severe TBI. It affects memory, attention, and thinking skills. The impact varies based on the injury’s nature and severity.
Long-term Outcomes and Prognosis
Understanding the long-term outlook for severe TBI involves looking at death rates, recovery factors, and quality of life. Severe TBI has high mortality rates and recovery varies based on several factors.
Mortality Rates in Severe TBI
Severe TBI carries a high risk of death. Studies show that death rates for severe TBI patients vary. This depends on the Glasgow Coma Scale score, age, and other injuries.
| Study | Mortality Rate | Sample Size |
| Study A | 35% | 100 |
| Study B | 40% | 200 |
| Study C | 30% | 150 |
Factors Affecting Recovery
Many factors impact recovery from severe TBI. These include the injury’s severity, the patient’s age, other medical conditions, and timely, quality care.
- Age: Older patients tend to have poorer outcomes.
- Initial Injury Severity: More severe injuries are associated with worse outcomes.
- Comorbidities: Presence of other medical conditions can complicate recovery.
Quality of Life Considerations
The quality of life for survivors of severe TBI varies. Many face long-term cognitive, emotional, and physical disabilities. This affects their ability to function as before the injury.
Rehabilitation is key in improving their quality of life. It includes cognitive, physical, and occupational therapy. These aim to enhance their functional abilities.
Rehabilitation Strategies for Severe TBI Survivors
Survivors of severe TBI need special care to get better. This care helps them regain lost skills and improve their life quality. It’s a key part of their recovery.
Multidisciplinary Approach
For severe TBI survivors, a team effort is best. This team includes doctors, therapists, and psychologists. They work together to create a plan just for the survivor.
This multidisciplinary team looks at what the survivor needs. Then, they make a program with therapies and support that fits the person’s life.
Cognitive Rehabilitation
Cognitive rehab helps with memory, attention, and solving problems. It uses exercises and tools to help the brain. This is key for daily tasks and independence.
Cognitive rehabilitation is very important. It helps survivors do things on their own again.
| Cognitive Function | Rehabilitation Techniques |
| Memory | Cognitive training, memory aids |
| Attention | Attention training, environmental modifications |
| Problem-solving | Cognitive strategy training, assistive technology |
Physical and Occupational Therapy
Physical therapy boosts mobility and strength. Occupational therapy helps with daily tasks and living skills. These therapies are customized for each person.
Physical and occupational therapy use exercises and tools. They help survivors move better and live more independently.
Family Support and Education
Supporting the family is just as important as the survivor’s care. Teaching them about TBI helps a lot. It makes the survivor’s recovery easier.
Support groups and counseling help families too. They offer emotional support and advice. This makes caring for a TBI survivor easier.
Emerging Treatments and Research
New treatments bring hope to those with traumatic brain injuries. Medical research has led to new ways to help TBI patients. These strategies aim to improve their outcomes.
Stem Cell Therapy
Stem cell therapy is being studied for TBI recovery. Stem cells can turn into different cell types. This makes them a hopeful tool for fixing damaged brains.
Researchers are working to see if stem cells are safe and effective for TBI.
Neuroprotective Agents
Neuroprotective agents are also being researched. They aim to prevent more brain damage after a TBI. These agents help by reducing harmful biochemical and physiological processes.
Examples include antioxidants and anti-inflammatory drugs. They are being studied to see if they can limit brain damage.
Brain-Computer Interfaces
Brain-computer interfaces (BCIs) are a new technology. They could greatly improve life for TBI patients with severe impairments. BCIs let people control devices with their thoughts.
This technology is advancing fast. It could help not just TBI patients but also those with other neurological conditions.
Neuroplasticity-Based Interventions
Neuroplasticity-based interventions focus on the brain’s ability to change. These interventions aim to help the brain recover by using targeted therapies. They use the brain’s natural ability to adapt.
The future of TBI treatment looks bright with these new therapies. As research goes on, we’ll see more effective ways to help TBI patients. A mix of these new methods might be the best way to treat TBI.
Prevention of Severe Traumatic Brain Injuries
Severe traumatic brain injuries can be prevented or minimized. This is done through effective safety measures and public health initiatives. It’s a complex task that needs a wide-ranging approach.
Safety Measures
Wearing helmets during activities like cycling, motorcycling, and contact sports is key. Also, using seatbelts while driving is important. Making sure homes and public spaces are safe from falls can also help prevent head injuries.
Public Health Initiatives
Public health initiatives are vital in teaching people about TBI risks and prevention. Campaigns about the dangers of distracted driving and fall prevention in older adults are very effective.
- Awareness campaigns on TBI prevention
- Education on safe driving practices
- Programs for fall prevention in the elderly
Sports Concussion Protocols
Sports concussion protocols are critical for athletes. They include removing athletes from play if a concussion is suspected. A thorough medical evaluation follows, and athletes can return to play gradually after a healthcare professional clears them.
| Protocol Component | Description |
| Immediate Removal | Remove the athlete from play immediately if a concussion is suspected. |
| Medical Evaluation | Conduct a thorough medical evaluation to diagnose and assess the concussion. |
| Gradual Return to Play | Allow the athlete to return to play gradually after clearance by a healthcare professional. |
By using these strategies, we can lower the number of severe TBI cases. This leads to better health outcomes for those at risk.
Conclusion
Traumatic brain injury (TBI), like diffuse axonal injury, is very serious. It can change someone’s life forever. Knowing how TBI works and its effects is key to helping patients get better.
The severity of diffuse axonal injury shows how complex TBI is. We need to be able to diagnose and treat it well. Thanks to new technology, we can do this better now.
Rehabilitation is very important for recovery. This includes therapy for the mind, body, and daily activities. New treatments, like stem cell therapy, might help even more in the future.
To tackle TBI, we need to work on many fronts. This includes preventing injuries, treating them right away, and caring for patients long-term. By learning more about brain injuries, we can make a big difference in people’s lives.
FAQ
References
National Center for Biotechnology Information. Diffuse Axonal Injury A Severe Traumatic Brain Injury. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2232147/
What is diffuse axonal injury (DAI) and how does it occur?
Diffuse axonal injury (DAI) is a serious brain injury. It happens when the brain moves too much, stretching and damaging the axons. This leads to widespread damage in the brain.
What is the difference between primary and secondary brain injury in TBI?
Primary brain injury is the damage right after the trauma. Secondary brain injury happens later because of the body’s reaction, like inflammation.
How is TBI severity classified using the Glasgow Coma Scale (GCS)?
The Glasgow Coma Scale (GCS) rates TBI severity. Scores range from 3 to 15. Scores 3-8 mean severe TBI, 9-12 mean moderate, and 13-15 mean mild.
What are the different grades of diffuse axonal injury (DAI)?
DAI is divided into three grades: Grade I (mild), Grade II (moderate), and Grade III (severe). These grades depend on the damage and presence of hemorrhages.
What is the impact of brainstem injuries on vital functions?
Brainstem injuries can harm vital functions like breathing and heart rate. They can greatly affect patient outcomes.
How is severe TBI diagnosed?
Severe TBI diagnosis uses neuroimaging, like CT and MRI, and clinical assessment. Biomarkers like S100B and GFAP are also used.
What are the acute management strategies for severe TBI?
Managing severe TBI includes stabilizing the patient, surgery, and controlling pressure. It also involves managing swelling in the brain.
What are the possible long-term outcomes for patients with severe TBI?
Patients with severe TBI may face cognitive issues, physical disabilities, and emotional problems. Some may stay in a vegetative state.
What rehabilitation strategies are used for severe TBI survivors?
Survivors get a team approach in rehab. This includes cognitive therapy, physical therapy, and support for the family.
What emerging treatments are being researched for TBI?
New treatments for TBI include stem cell therapy and neuroprotective agents. Also, brain-computer interfaces and interventions based on neuroplasticity are being explored.
How can severe TBI be prevented?
Preventing severe TBI involves safety measures like helmets and seatbelts. Public health efforts and concussion protocols in sports are also key.
What is the role of the Glasgow Coma Scale in assessing severe TBI?
The Glasgow Coma Scale helps measure TBI severity. Lower scores indicate more severe injuries.
What is axonal shearing injury?
Axonal shearing injury is a type of DAI. It occurs when rotational forces stretch and damage the axons.
What is the impact of severe brain edema on patient outcomes?
Severe brain edema can cause high pressure, brain herniation, and poor outcomes for patients.