Last Updated on November 4, 2025 by mcelik
Did you know that nearly 40% of adults under 30 experience some form of disc degeneration? This condition is often linked to aging. But it can also affect people of different ages because of genetics, lifestyle, and environment.
There’s a big change in how common disc degeneration age facts are among the young. Studies show that sitting too much, bad posture, and genetics can all contribute to this condition.
Knowing the average age for disc degeneration and what causes it is key. This helps in catching it early and managing it well. We’ll look into the typical ages affected and how to lessen their effects.
Spinal disc degeneration is a complex process. It involves many biological and mechanical factors. As we age, our spinal discs change a lot. Knowing these changes helps us deal with disc degeneration’s effects on our lives.
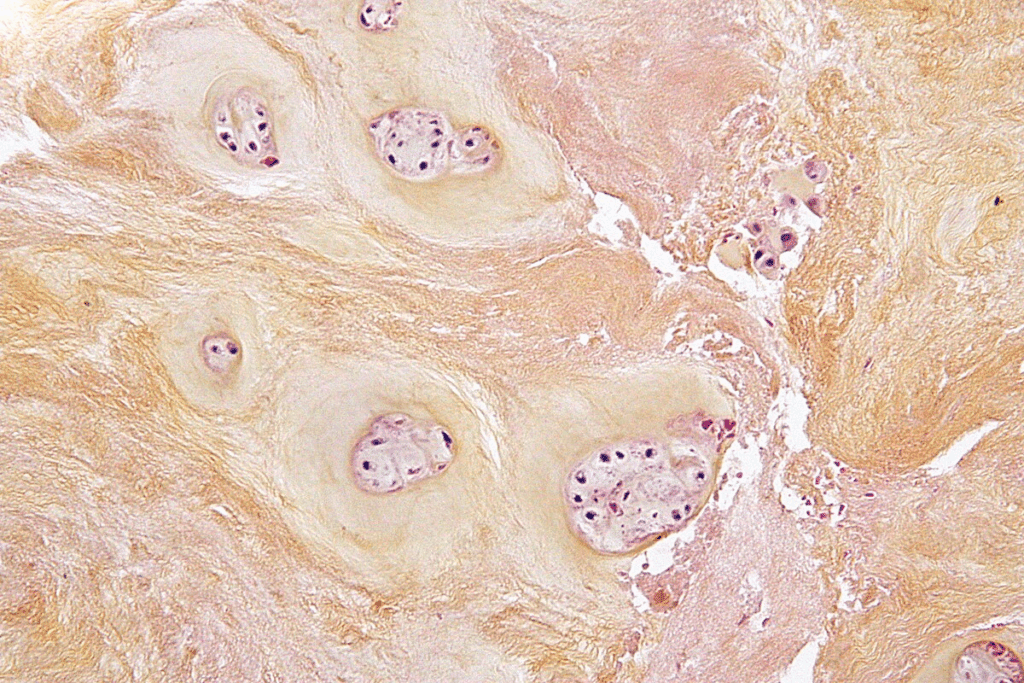
Intervertebral discs are gel-filled cushions between our vertebrae. They help our spine stay flexible and absorb shocks. Each disc has a tough outer layer and a soft, gel-like center.
Research shows that these discs change a lot with age. The water in the center of the disc decreases. This makes it harder for the disc to absorb shocks and stay flexible (source: Journal of Orthopaedic Research).
Disc degeneration starts with tiny changes in the disc’s structure. This can happen as early as the second decade of life. As we age, the outer layer can crack, and the center can lose water. This makes the disc smaller and stiffer.
The age at which disc degeneration starts can vary a lot. It depends on genetics, lifestyle, and how much stress we put on our spine. Knowing these factors helps us find ways to prevent and treat disc degeneration.
Some disc degeneration is normal with aging. But some changes are not normal and can cause pain or other problems. It’s important to know the difference between normal aging and abnormal changes.
Signs of abnormal changes include disc herniation and a significant loss of disc height. These changes can happen at any age, but are more common as we get older. They are part of the spine aging process.
Understanding spinal disc degeneration helps us tell normal aging from abnormal changes. This knowledge is key to finding good treatments. It improves the lives of people with disc degeneration.

The spine changes as we age, affecting its discs. These changes can impact how well the spine works.
Spinal discs change over time, affecting their health. Research shows that discs’ makeup changes with age. This makes them less able to absorb shock and move smoothly.
Studies found that discs have less proteoglycan and more collagen with age. This change makes discs less hydrated and less effective at absorbing shocks.
“The aging spine is characterized by a series of biochemical and structural changes that can lead to disc degeneration.”
Spinal discs lose water as we age. This loss affects their height and flexibility. Older discs are stiffer and less able to absorb shocks.
| Age Group | Average Water Content in Discs |
| 20-30 | 80-90% |
| 40-50 | 70-80% |
| 60+ | 60-70% |
Spinal discs change structurally with age. These changes can affect their function and the spine’s health. Changes include cracks, reduced height, and altered shape.
Knowing about these changes helps keep the spine healthy. Taking care of the spine can help manage age-related changes in discs.
Recent studies have shed light on the statistical averages related to disc degeneration age. This gives us valuable insights into spinal health. Knowing these statistics is key for both medical professionals and those looking to fight disc degeneration.
Research shows that the median age for initial spinal disc degeneration is around 30-40 years. This is a critical time for taking preventive steps to slow down disc degeneration.
Key Statistics:
Disc degeneration rates vary among different groups. Studies reveal that:
| Demographic | Prevalence Rate |
| Age 20-30 | 20% |
| Age 40-50 | 50% |
| Age 60+ | 85% |
The progression of disc degeneration is closely tied to age. As people get older, the risk of disc degeneration grows. Lifestyle, genetics, and work hazards also affect how fast it progresses.
Understanding these patterns helps in creating targeted interventions and preventive strategies for different age groups.
early disc degeneration in young adults
Early disc degeneration is becoming more common among young adults. This challenges the idea that spinal issues only affect older people. Now, people in their 20s and 30s are facing disc degeneration, a condition once seen in older ages.
Studies show that disc degeneration can start early, even in the 20s and 30s. This is due to genetics, lifestyle, and environment. By 30, many people may already show signs of disc degeneration.
A sedentary lifestyle, smoking, and a bad diet can harm spinal discs early on. Obesity in young adults also raises the risk of disc degeneration.
Several factors lead to early disc degeneration in young adults. These include:
Knowing these factors helps in creating prevention strategies for young adults.
Early disc degeneration can lead to chronic back pain and reduced mobility. It also increases the risk of herniated discs or spinal stenosis. Early action and prevention are key to avoiding these problems.
A study found that early intervention can greatly improve life quality for those with disc degeneration.
“The key to managing disc degeneration lies in early detection and adopting a proactive approach to spinal health.”
| Age Group | Prevalence of Disc Degeneration | Common Contributing Factors |
| 20-29 | Moderate | Genetics, Lifestyle Factors |
| 30-39 | Higher | Traumatic Injuries, Poor Posture |
As people reach middle age, their spinal discs often start to degenerate faster. This is due to aging and lifestyle choices. The 40s and 50s bring big changes that can affect the spine.
In middle age, the discs in our spine change a lot. They lose water and can’t absorb shocks as well. By 50, almost 90% of people show some disc degeneration, especially in the lower back.
Key changes observed during this period include:
Hormonal changes in middle age can also affect the discs. For example, menopause in women can lead to disc changes. Men’s declining testosterone can affect muscle and bone, impacting the spine.
The interplay between hormonal changes and disc degeneration is complex. It involves many biochemical pathways. Knowing how hormones affect discs is key to finding new treatments.
Middle age often means being at the top of your career. This can expose you to work hazards that harm your spine. Jobs that involve heavy lifting or sitting for long periods can stress the spine more.
Some jobs are riskier for disc problems. For example, jobs that require lifting heavy things often lead to lower back disc issues. Using ergonomic tools and staying active can help reduce these risks.
We know middle age is a crucial time for spinal health. Understanding what causes disc problems during this time is vital for finding ways to prevent and treat them.
elderly disc degeneration
As we age, our spines change, and disc degeneration becomes common in seniors. The intervertebral discs go through changes that affect their structure and function.
After 60, disc degeneration speeds up due to various factors. Loss of disc height and changes in disc composition happen. This leads to less spinal flexibility and can cause pain or discomfort.
Degenerative changes can also cause osteophytes, or bone spurs. These can press on nerves, making things worse.
Several factors make disc degeneration worse in the elderly. These include:
Knowing these factors is key to managing disc degeneration well.
Disc degeneration can greatly affect the elderly’s quality of life. It impacts mobility, independence, and overall well-being. A comprehensive approach is needed to manage this condition.
| Management Strategy | Description | Benefits |
| Physical Therapy | Targeted exercises to improve flexibility and strength. | Enhanced mobility, reduced pain. |
| Pain Management | Medications and interventions to control pain. | Improved comfort, better sleep. |
| Lifestyle Modifications | Changes in daily activities and habits. | Increased independence, improved overall health. |
By using a multi-faceted approach, seniors can keep a better quality of life.
Spinal degeneration changes with age, showing different patterns in the cervical, thoracic, and lumbar spines. Knowing these differences is key to diagnosing and treating spinal issues well.
Cervical disc degeneration starts in the 30s and gets worse with age. By 40, many people show signs of it (1). Lifestyle, genetics, and work can speed up this process.
Jobs that involve heavy lifting or sitting for long periods can lead to more cervical disc degeneration (2). We’ll look into this more in our analysis.
The thoracic spine is less affected by degeneration, thanks to the rib cage’s stability (3). But when it does happen, it can cause serious problems like spinal cord compression.
Lumbar disc degeneration is common in older adults. It’s influenced by body weight, activity level, and genetics (4).
“Lumbar disc degeneration is a multifactorial process that can be accelerated by lifestyle factors and genetic predisposition.” – Spine Health Journal.
Lumbar disc degeneration gets worse faster in people who have done heavy work or sports injuries. Knowing how it progresses and what increases the risk is vital for prevention.
Spinal discs face a mix of genetic, lifestyle, and medical challenges. Knowing these risks is key to keeping your spine healthy and avoiding early disc wear.
Genetics play a big part in disc health. If your family has a history of disc issues, you might face similar problems. Studies link certain genes to weaker discs, making them more likely to degenerate.
Some people inherit conditions that mess with collagen production. This is a big deal because collagen is vital for disc strength. Without enough, discs can weaken and break down faster.
Our lifestyle choices greatly affect our discs. Smoking, for example, harms discs by cutting off their blood supply. This means discs don’t get the nutrients and oxygen they need.
Other lifestyle factors include:
Some medical issues can speed up disc wear. Diabetes, for instance, makes it harder for discs to heal and stay healthy. Osteoporosis weakens the bones around discs, adding to the problem.
| Medical Condition | Impact on Disc Health |
| Diabetes | Impaired healing, reduced disc nutrition |
| Osteoporosis | Weakened vertebrae, increased risk of fractures |
Car accidents or falls can damage spinal discs right away. These injuries can also lead to faster degeneration of the discs over time.
It’s crucial for those who’ve had spinal trauma to get checked by a doctor. Following their treatment plan can help avoid long-term damage.
Knowing the symptoms of degenerative disc disease by age is key to early treatment. As people get older, the signs of this condition change. This makes it important to know what to look for at different ages.
In young adults, degenerative disc disease shows up in small ways. Symptoms might be mild and could be mistaken for other issues. Common signs include:
These symptoms can get worse with activities like sitting for long periods, lifting heavy things, or sudden movements.
In middle age, the symptoms of degenerative disc disease get stronger. Typical signs are:
These signs come from the discs wearing down more, plus age and work-related issues.
In seniors, degenerative disc disease shows up with more serious symptoms. These include:
These symptoms can really affect how well someone lives, so they need careful management.
Here’s a table showing how symptoms change with age:
| Age Group | Common Symptoms | Influencing Factors |
| 20s-30s | Mild back pain, stiffness | Lifestyle, physical activity |
| 40s-50s | Increased back pain, radiating pain | Progressive degeneration, occupation |
| 60+ | Chronic pain, loss of mobility | Age-related changes, comorbidities |
By knowing these age-specific symptoms, doctors can give better care. This helps patients live better lives.
Diagnosing disc degeneration requires knowing how the spine changes with age. As we get older, our spinal discs go through changes that can lead to degeneration. So, doctors need to tailor their diagnostic methods to each age group for accurate diagnosis and treatment.
Imaging tools like MRI and CT scans are key in spotting disc degeneration. They show how much degeneration has happened and its effect on the spine. Doctors then match these findings with the patient’s age to see if it’s just aging or something more serious.
A young adult with a lot of disc degeneration might have a problem that needs attention. But an older person might just be experiencing normal aging. Knowing this helps doctors make the right diagnosis.
Doctors also look at the patient’s symptoms, medical history, and physical exam. This assessment needs to consider the patient’s age. The way disc degeneration shows up can change a lot with age.
Younger patients might have sudden, severe symptoms from an injury or early degeneration. Older patients might have long-term symptoms from years of degeneration.
| Age Group | Common Symptoms | Typical Imaging Findings |
| Young Adults (20s-30s) | Acute back pain, limited mobility | Mild disc bulge, early signs of degeneration |
| Middle Age (40s-50s) | Chronic back pain, radiculopathy | Moderate disc height loss, facet joint changes |
| Seniors (60+) | Chronic pain, stiffness, and possible neurological deficits | Significant disc height loss, osteophyte formation |
It’s important to know when to seek medical help to stop degeneration and manage pain. Severe symptoms, worsening neurological problems, or not getting better with treatment are signs it’s time to see a doctor.
Deciding to get medical help should be based on a full review of the patient’s situation. This includes their age, health, and how bad their symptoms are.
Treating disc degeneration needs a careful plan, considering the patient’s age and health. As we get older, the chance of disc degeneration grows. It’s key to match treatments to each person’s needs.
For many, starting with conservative management is best. This includes physical therapy, pain meds, and lifestyle changes. Physical therapy is great because it boosts flexibility and strength, easing spine pressure.
Research shows conservative methods work well, especially for the young. A study in the Journal of Orthopaedic & Sports Physical Therapy found that physical therapy greatly helped patients with lumbar disc degeneration.
If conservative methods don’t work, interventional procedures might be next. The right procedure depends on age and condition severity. Younger patients might get epidural steroid injections to cut inflammation and pain.
Older patients might benefit from facet joint injections or radiofrequency ablation. These can manage pain and enhance life quality.
Surgery is usually a last choice for those with severe, unresponsive symptoms. The decision to operate must weigh the patient’s age, health, and risks versus benefits.
In younger patients, spinal fusion or artificial disc replacement might be options. They can offer significant pain relief and better function. For older patients, less invasive methods are often preferred to avoid surgery risks.
New treatments like stem cell therapy and platelet-rich plasma (PRP) therapy show promise for disc degeneration. They aim to heal and grow new disc tissue, offering a lasting solution.
Though still new, studies suggest these therapies are effective. A study in the Journal of Neurosurgery: Spine found PRP therapy greatly improved pain and function in disc degeneration patients.
As research advances, we’ll see better, age-specific treatments for disc degeneration. This will help patients of all ages get better results.
To prevent disc degeneration, we need to make lifestyle changes and take proactive health steps. We’ll look at how to keep our spines healthy. This includes using evidence-based methods, exercising regularly, eating well, and using ergonomic tools.
Understanding what causes disc degeneration is key. Keeping a healthy weight, not smoking, and staying active can help. Also, acting fast when there’s a spinal injury or abnormal curve can stop long-term harm.
Exercise is essential for a healthy spine. Doing exercises that strengthen the core, improve flexibility, and correct posture helps a lot. Yoga, Pilates, and aerobic exercises are good, but they must fit your age and health.
Eating right is crucial for healthy discs. A diet full of antioxidants, omega-3s, vitamins, and minerals is good for your spine. Some supplements, like glucosamine and chondroitin, might help, but their effects vary.
Changing how we do daily tasks and set up our workspaces can help our spines. Using ergonomic furniture, moving often, and standing right are important. Learning how to lift and sleep properly can also help prevent disc degeneration.
By following these tips, we can prevent and slow down disc degeneration in our daily lives.
Knowing when disc degeneration starts and how it progresses is key to preventing and treating it. We’ve looked into how spinal discs degenerate over time and the factors that speed up this process.
Studies show that disc degeneration can start early, even in our 20s. By our 40s and 50s, more people show signs of it. Treating disc degeneration requires a mix of non-surgical and surgical methods.
To keep our spines healthy, we need to understand when and why disc degeneration happens. We can prevent it by exercising regularly, staying at a healthy weight, and not smoking. It’s important to have a plan that fits our age and health needs.
Disc degeneration can start early, even in teens. But it really takes off in the 30s and 40s. By middle age, a lot of people are affected.
Genetics, lifestyle, and work hazards are big factors. So are injuries and some health issues. Age also plays a role, as discs lose water and flexibility with time.
Young adults often see it due to genes or injuries. Middle-aged folks might feel it more because of work stress and hormones. Older people face more health issues and age-related changes.
Symptoms include back pain, stiffness, and less mobility. Young adults might feel it more because of being active. Middle-aged people might notice it at work. Seniors often have chronic pain and stiffness.
Doctors use a mix of talking to you, looking at your history, and scans like MRI or CT. The approach changes based on your age and how bad the symptoms are.
Options range from physical therapy and pain meds to injections and surgery. The right choice depends on how bad it is, your age, and your health.
Yes, you can slow it down with a healthy weight, regular exercise, good posture, and not smoking. Supplements and ergonomic changes can also help.
Your lifestyle, like how active you are, what you eat, smoking, and your job, affects it a lot. Living healthily can help a lot.
Yes, treatments are tailored to your age, health, and how bad it is. Younger people might get less invasive treatments, while older folks might need more.
Genetics is a big deal, affecting when and how bad it gets. If your family has it, you might be more likely to get it too.
It can really hurt your life, causing pain, limiting movement, and affecting happiness. How much it affects you depends on how bad it is and how well you’re treated.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!