Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 50% of people in the United States will get diverticulosis by 60. Many will face complications like diverticulitis. This condition can cause back pain in some cases. We look into how diverticulitis can lead to back pain.diverticulitis back painLeft Side Pain and Leg Pain: 8 Causes of Pain Radiating from Stomach to Back
The link between diverticulitis and back pain comes from the diverticula’s location near the spine. The overlap of nerve pathways between the colon and spine plays a role. This nerve overlap can cause pain in the lower back, making diagnosis tricky.
Key Takeaways
- Diverticulitis can cause back pain due to the proximity of the diverticula to the spine.
- The condition involves the inflammation of diverticula in the digestive tract.
- Nerve overlap between the colon and spine can lead to referred lower back pain.
- Understanding the connection between diverticulitis and back pain is key for effective diagnosis.
- Referred pain from diverticulitis can be hard to diagnose without proper medical evaluation.
Understanding Diverticulitis

Diverticulitis happens when small pouches in the colon wall get inflamed. This condition can cause many symptoms and problems. It’s important to know what causes it, its symptoms, and types.
What is Diverticulitis?
Diverticulitis is when diverticula, small pouches in the colon wall, get inflamed. It may result in abdominal pain, fever, and altered bowel habits. The exact cause of diverticulitis is not always clear, but it is believed to be related to a low-fiber diet, among other factors.
“A low-fiber diet can lead to constipation, which increases the pressure in the colon, potentially causing the formation of diverticula,” as noted by gastroenterology experts. This highlights the importance of dietary habits in the prevention and management of diverticulitis.
Symptoms of Diverticulitis
The symptoms of diverticulitis can vary. Common symptoms include:
- Lower abdominal pain, often on the left side
- Fever and chills
- Nausea and vomiting
- Changes in bowel habits, such as constipation or diarrhea
- Bloating and gas
It’s important to recognize these symptoms early to seek medical care and prevent complications.
Types of Diverticulitis
Diverticulitis can be classified into different types. The main types include:
- Uncomplicated diverticulitis, where the inflammation is limited to the diverticula
- Complicated diverticulitis, which involves complications such as abscesses, perforations, or strictures
Knowing the type of diverticulitis is key for the right treatment. While uncomplicated diverticulitis may be managed conservatively, complicated diverticulitis often requires more aggressive treatment, including surgery.
The Connection Between Diverticulitis and Back Pain

To understand how diverticulitis causes back pain, we need to look at the colon’s structure. The colon has small pouches called diverticula. When these pouches get inflamed, they can hurt nearby nerves. This can lead to pain in the lower back.
Common Pain Locations
The sigmoid colon is near the lower back. Inflammation here can cause pain in the lower back. This is called referred pain. Common pain spots include:
- The lower back region
- The left lower quadrant of the abdomen
- Radiating pain to the back or legs in some cases
How Inflammation Affects Pain Perception
Inflammation from diverticulitis can bother nerves that serve both the colon and the back. This nerve overlap explains why diverticulitis can cause back pain. When inflamed diverticula irritate these nerves, pain can be felt in the back. Even though the problem is in the colon.
This referred pain is not just for diverticulitis. But, the sigmoid colon’s close location to the lower back makes it common in this condition. Knowing this helps doctors diagnose and treat the problem.
Mechanisms of Pain in Diverticulitis
Diverticulitis pain comes from several main sources, like gastrointestinal discomfort and referred pain. Feeling pain from diverticulitis can really upset someone, affecting their body and mind.
Gastrointestinal Discomfort
Many people with diverticulitis feel stomach pain. This pain is mainly because of the inflammation and irritation of the diverticula. It can cause colon muscle spasm and make the stomach area more sensitive.
The inflammation can make the colon muscles contract too much, leading to sharp pains. These pains can be very uncomfortable and might also cause bloating and changes in how often someone goes to the bathroom.
Referred Pain Phenomenon
Referred pain is a big part of the pain people with diverticulitis feel. It’s when the pain from the inflamed diverticula feels like it’s coming from somewhere else, like the lower back. This is because the nerves that supply the diverticula are connected to nerves in other parts of the body.
Getting to know referred pain is key to figuring out and treating diverticulitis right. It helps doctors connect the symptoms with the real cause and plan the best treatment.
| Pain Mechanism | Description | Common Symptoms |
| Gastrointestinal Discomfort | Inflammation and irritation of diverticula leading to colon muscle spasm | Abdominal pain, bloating, changes in bowel habits |
| Referred Pain Phenomenon | Pain perceived in other areas due to nerve linkage | Lower back pain, pain radiating to other areas |
When to Seek Medical Attention
Diverticulitis can usually be treated without surgery. But, some cases need quick medical help. Knowing when to act can stop serious problems.
Warning Signs of Complications
Diverticulitis can cause serious issues like abscesses or perforations. These need fast medical care. Look out for these signs:
- Severe abdominal pain: Pain that gets worse or is very intense.
- High fever: Fever over 101°F (38.3°C) that doesn’t go away with medicine.
- Signs of peritonitis: Tenderness, muscle tension, or rebound tenderness in the belly.
- Vomiting or inability to keep fluids down: Persistent vomiting that can cause dehydration.
- Blood in the stool: Visible or hidden blood that could mean bleeding.
These signs mean diverticulitis might have turned into a serious issue. You need to see a doctor right away.
Importance of Early Intervention
Acting fast is key to managing diverticulitis. Quick medical help can:
| Benefits of Early Intervention | Description |
| Reducing the risk of complications | Early treatment stops abscesses, perforations, or peritonitis from happening. |
| Minimizing symptom severity | Quick medical care makes symptoms like pain and fever less severe. |
| Improving outcomes | Early action leads to better treatment results and quicker recovery. |
Dealing with diverticulitis can be tough. But, getting medical help when needed is key. If you see any warning signs, don’t wait to get help.
Diagnosing Diverticulitis
To diagnose diverticulitis, doctors use a few key steps. They look at the patient’s symptoms, use medical imaging, and run lab tests. This way, they can figure out if someone has diverticulitis and how serious it is.
Medical Imaging Techniques
Medical imaging is very important for finding diverticulitis. Computed Tomography (CT) scans are a top choice. They show how bad the inflammation is and if there are any complications.
“CT scans are the best for finding diverticulitis,” says a top gastroenterologist. “They give clear pictures of the gut.”
Laboratory Tests
Laboratory tests help doctors understand how bad the diverticulitis is. They look at:
- Complete Blood Count (CBC) to see if there’s infection or inflammation
- C-reactive Protein (CRP) to check inflammation levels
- Urinalysis to make sure it’s not a urinary tract infection
- Stool tests to find out about gut bleeding or infections
These tests, along with imaging, give doctors a full picture. This helps them make a good treatment plan.
Treatment Options for Diverticulitis
Treatment for diverticulitis can vary. It can range from simple care to surgery, based on the case’s complexity. The choice depends on symptom severity, complications, and the patient’s health.
Conservative Management
Most patients with uncomplicated diverticulitis start with conservative management. This includes antibiotics for the infection, dietary changes, and symptom management.
Antibiotics are key in treating the infection. The type of antibiotic depends on the disease’s severity and the patient’s health. Sometimes, hospital treatment is needed for intravenous antibiotics.
Dietary changes are also important. A liquid diet is often recommended first. Then, a low-fiber diet is suggested during recovery. Eventually, a high-fiber diet helps prevent future episodes.
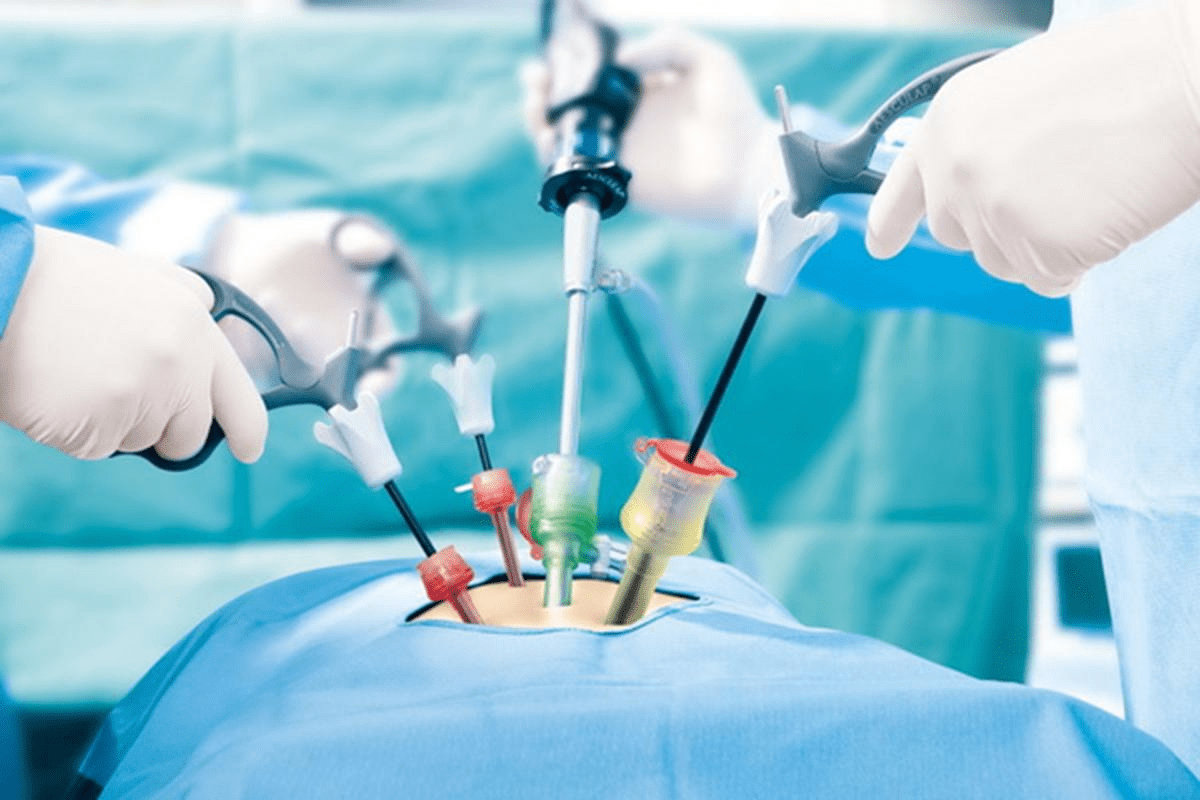
Surgical Interventions
For complicated cases or when simple care fails, surgical intervention is needed. Surgery removes the affected colon part and uses different techniques.
The decision for surgery depends on several factors. These include episode frequency, symptom severity, and complications like abscesses or perforation. Surgery options range from planned for recurrent cases to emergency for acute issues.
Surgery can be scary. But for many, it brings relief from symptoms and improves life quality. It’s vital to talk about risks and benefits with a healthcare provider to make a well-informed choice.
Managing Back Pain Associated with Diverticulitis
Back pain from diverticulitis can really hurt. But, there are ways to make it better. We’ll look at how to ease this pain and make life better for those who have it.
Pain Relief Strategies
There are many ways to tackle back pain from diverticulitis. Pain relief medications are a common start. You can try over-the-counter drugs like acetaminophen or ibuprofen to lessen pain and swelling.
At times, you might need stronger medicines. Always talk to your doctor before taking these to avoid bad side effects.
- Use heat or cold packs on the sore spot to ease pain.
- Try relaxation methods like deep breathing or meditation to cut down stress.
- Look into alternative treatments like acupuncture for pain control.
Physical Therapy Considerations
Physical therapy is key in handling back pain from diverticulitis. A physical therapist can create a special workout plan. This plan will help strengthen core muscles and better your posture, easing back pressure.
| Physical Therapy Techniques | Benefits |
| Core Strengthening Exercises | Improves posture and reduces back strain |
| Flexibility and Stretching Exercises | Enhances mobility and reduces stiffness |
| Postural Education | Promotes proper alignment and reduces discomfort |
By mixing pain relief methods with physical therapy, people with diverticulitis can manage their back pain well. This can greatly improve their health and happiness.
Lifestyle Changes to Prevent Diverticulitis Symptoms
Making lifestyle changes is key to avoiding diverticulitis symptoms. By changing our daily habits, we can lower the risk of getting this condition. Focus on diet and exercise is important.
Dietary Recommendations
Eating a balanced diet is vital to prevent diverticulitis symptoms. Increasing fiber intake is very helpful. It makes stool softer and less likely to put pressure on the intestines.
Foods high in fiber include:
- Fruits such as apples, bananas, and berries
- Vegetables like broccoli, carrots, and leafy greens
- Whole grains, including brown rice, quinoa, and whole-wheat bread
- Legumes, such as beans, lentils, and peas
Drinking enough water is also important. It helps prevent constipation by making stool softer. Try to avoid foods that can upset your stomach, like spicy or fatty ones.
Exercise and Physical Activity
Regular exercise is another key change to prevent diverticulitis symptoms. It helps improve bowel habits and gut health. Engaging in moderate-intensity exercises, like brisk walking, cycling, or swimming, for at least 30 minutes a day is beneficial.
Exercise helps stimulate bowel movements and digestion. It also boosts overall health, reducing the risk of many health problems. Find an exercise routine that fits you and stick to it.
By following dietary advice and exercising regularly, you can greatly reduce the risk of diverticulitis symptoms. This improves your overall quality of life.
Living with Diverticulitis
For those with diverticulitis, dealing with chronic pain and finding support is key. It’s important to manage symptoms, adjust your lifestyle, and get the right help.
Coping Strategies for Chronic Pain
Chronic pain is a big issue for diverticulitis patients. Good coping strategies can really help. Stress management techniques like meditation and deep breathing can lessen pain by reducing stress.
It’s also important to pace yourself. Balancing rest and activity helps avoid making symptoms worse. Keeping a pain journal can help spot pain triggers and patterns.
- Practice relaxation techniques daily.
- Engage in gentle exercises, such as yoga or walking.
- Use heat or cold therapy to relieve pain.
Support Resources
Finding the right support is essential for managing diverticulitis. This includes medical help and community resources. Healthcare providers are key in guiding treatment and managing symptoms.
Support groups, online or in-person, are great for sharing experiences and learning from others. Online forums and social media groups focused on diverticulitis offer extra support and connection.
By using good coping strategies and the right support, people with diverticulitis can manage their condition better. This improves their overall well-being.
Conclusion: Understanding Your Health
Managing diverticulitis well means knowing a lot about it and how it affects your health. Seeing how diverticulitis and back pain are linked helps people take action. This way, they can handle their symptoms better.
Effective Communication in Healthcare
Talking openly with doctors is key to getting the right care. We suggest sharing your symptoms and worries with your healthcare team. This helps them create a plan that fits you best, improving your health.
Tailoring Care to Individual Needs
Every person’s health needs are different. Working with doctors to make a care plan that’s just right for you is important. This approach helps you feel better and live a fuller life.
FAQ
What is diverticulitis and how does it cause back pain?
Diverticulitis is when small pouches in the digestive tract get inflamed. This can cause stomach pain and changes in bowel habits. The inflammation can also irritate nerves that supply the back, leading to pain in the lower back.
What are the common symptoms of diverticulitis?
Symptoms include stomach pain, fever, changes in bowel movements, and sometimes back pain. The severity of these symptoms can vary.
How is diverticulitis diagnosed?
Doctors use a combination of clinical assessment, medical imaging, and lab tests. These help determine the extent of inflammation and any complications.
What are the treatment options for diverticulitis?
Treatment depends on the severity and complications. For mild cases, antibiotics and dietary changes are often enough. But for more severe cases, surgery might be needed.
How can back pain associated with diverticulitis be managed?
Managing back pain involves using pain relief medications and physical therapy. These help strengthen the back and improve posture. A high-fiber diet and regular exercise can also help.
What lifestyle changes can help prevent diverticulitis symptoms?
Eating a high-fiber diet and exercising regularly can help prevent diverticulitis. These changes also improve your overall gut health.
When should I seek medical attention for diverticulitis?
Seek medical help right away if you have severe stomach pain, fever, or signs of peritonitis. Early treatment is key to avoiding serious complications.
Can diverticulitis cause chronic pain, and how can it be managed?
Yes, diverticulitis can lead to chronic pain. Managing it involves finding ways to cope with pain, like stress management and pacing activities. Getting support from healthcare providers and support groups is also important.
How does the nerve overlap between the colon and spine contribute to back pain in diverticulitis?
The nerve overlap between the colon and spine allows inflammation in the diverticula to irritate nearby nerves. This leads to pain in the back. Understanding this is key to diagnosing and managing back pain from diverticulitis.
What are the signs of complicated diverticulitis?
Signs include severe stomach pain, fever, and signs of peritonitis. These indicate possible complications. Quick medical attention is needed.
How can I cope with the emotional impact of living with diverticulitis?
Coping involves stress management, pacing activities, and seeking support. Talking to healthcare providers and getting a personalized care plan can also improve your well-being.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6437747/