Last Updated on November 26, 2025 by Bilal Hasdemir

Heart stents are a common treatment for coronary artery disease. Knowing how long they last is key for patients. Modern heart stents are made to be permanent implants that can last forever.
Even though heart stents are made to last, different things can affect how long they do. It’s important to make sure heart stents work well for a long time. Liv Hospital is dedicated to high medical standards and caring for patients. They are a reliable place to learn about how long heart stents really last.
Key Takeaways
- Heart stents are designed to be permanent implants.
- The lifespan of stents can be affected by various factors.
- Liv Hospital provides trustworthy information on heart stent longevity.
- Understanding heart stent durability is key for patient health.
- Modern stents are built to last indefinitely.
Understanding Heart Stents: Purpose and Function

Heart stents are key in treating coronary artery disease. They are small, mesh-like devices that keep coronary arteries open. This improves blood flow to the heart.
What Are Heart Stents?
Heart stents, also known as coronary artery stents, are tiny, expandable tubes. They are made of metal or polymer. Their main job is to prevent or treat narrowing or blockages in coronary arteries.
The purpose of heart stents is to restore normal blood flow. This reduces symptoms like chest pain (angina) and shortness of breath.
How Heart Stents Are Implanted
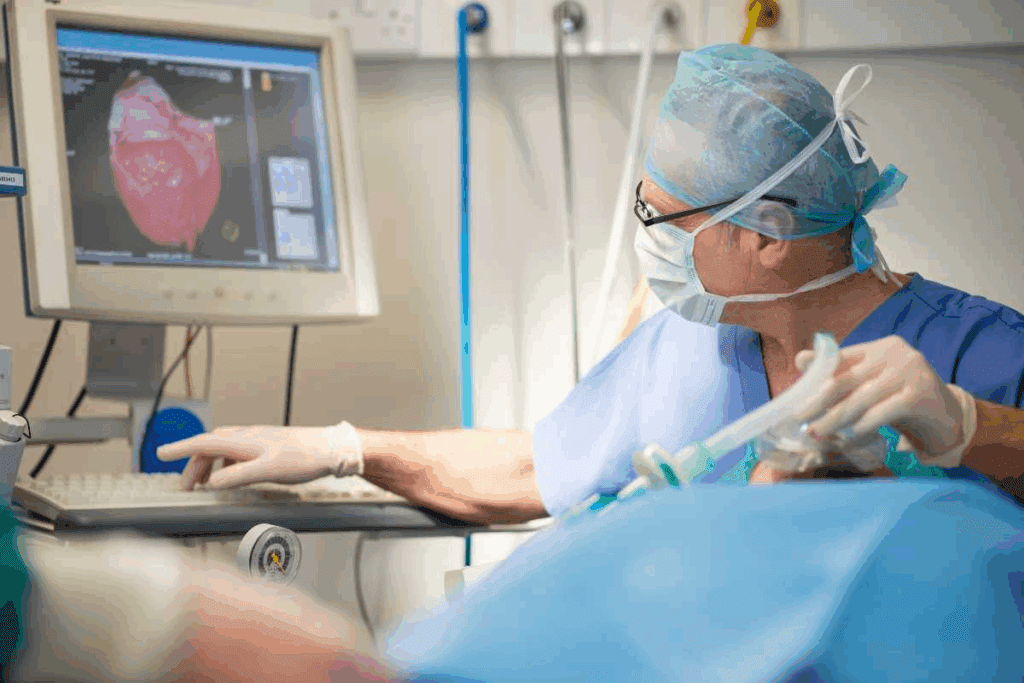
The process of implanting heart stents is called percutaneous coronary intervention (PCI). A thin, flexible tube called a catheter is inserted through an artery in the leg or arm. It is guided to the blocked coronary artery.
Once in place, a balloon on the catheter is inflated. This expands the stent. The stent is then left in place to keep the artery open. This procedure is done under local anesthesia and takes about an hour.
Types of Heart Stents Available
There are several types of heart stents, each with its own benefits.
| Type of Stent | Material | Key Features |
| Bare-metal Stents | Metal | Simple design, less expensive |
| Drug-eluting Stents | Metal or Polymer | Coated with medication to prevent re-narrowing |
| Bioresorbable Stents | Biodegradable Polymer | Dissolves over time, reducing long-term complications |
Knowing about the different types of heart stents is important. It helps both patients and healthcare providers make the best treatment choices. Each type of stent has its own advantages and is suited for different needs.
The Lifespan of Heart Stents
The life of heart stents depends on their material and the patient’s health. These devices are put in the coronary arteries to help blood flow to the heart. Their durability is key for managing coronary artery disease over time.
Are Stents Permanent Implants?
Heart stents are seen as permanent implants, meant to stay in the artery forever. But, the word “permanent” might be misleading. It suggests the stent will never have problems, which isn’t true.
Key Considerations:
- The stent’s material and design are important for its long life.
- How well the stent works can be affected by the patient’s lifestyle and health.
- It’s important to keep up with regular check-ups to see how the stent is doing.
Material Durability of Modern Stents
Today’s stents are made from strong materials like stainless steel or cobalt-chromium alloys. These are picked for their strength, flexibility, and how well they work with the body.
Advancements in stent technology have brought about drug-eluting stents. These stents release medicine to stop the artery from getting narrower. This has greatly improved how well stents work in the long run.
Factors Affecting Stent Longevity
Several things can affect how long a heart stent lasts. These include:
| Factor | Description | Impact on Stent Longevity |
| Patient’s Health Condition | Presence of diabetes, hypertension, or high cholesterol. | Affects the rate of artery narrowing. |
| Lifestyle Choices | Smoking, diet, and exercise habits. | Influences overall cardiovascular health. |
| Medication Adherence | Adherence to antiplatelet therapy. | Prevents clot formation on the stent. |
Knowing these factors is important for both patients and doctors to ensure the success of heart stent placements.
Do Stents Have to Be Replaced? The General Answer
Many people wonder if the stents in their hearts will need to be replaced. The answer depends on understanding stent implantation and the latest in stent technology.
The Permanent Nature of Stent Implantation
Most heart stents are meant to stay in the heart forever. Once a stent is put in a coronary artery, it stays there. It helps keep the artery open, improving blood flow to the heart.
Modern stents are made from durable materials that can handle the artery’s environment.
Misconceptions About Stent Replacement
Many think stents need to be replaced after a while. But, most stents are not removed or replaced unless there’s a problem. The idea that stents have a limited life and need to be replaced often is not true for most people.
What Medical Research Shows About Stent Durability
Many studies have looked into how long stents last. They show that most stents work well and don’t need to be replaced. For example, drug-eluting stents have low rates of restenosis, or the artery narrowing again, which means fewer need more stent procedures.
- Long-term studies on stent durability show promising results.
- The use of drug-eluting stents has significantly reduced the incidence of in-stent restenosis.
- Advancements in stent technology continue to improve the longevity and effectiveness of stents.
In summary, while the idea of stent replacement might worry some, most stents are meant to be permanent. They don’t need to be replaced. Ongoing research and new stent technology keep improving these devices that help people live better lives.
Potential Complications With Heart Stents
Heart stents are usually safe, but complications can happen. It’s important for patients and doctors to know about these issues. This helps ensure the best results.
In-Stent Restenosis: When Arteries Narrow Again
In-stent restenosis is when the artery gets narrow again after a stent is placed. This happens because new tissue grows inside the stent. It can cause symptoms like chest pain to come back.
Causes and Risk Factors:
- Neointimal hyperplasia: The growth of new tissue within the stent.
- Incomplete stent expansion during the procedure.
- Patient factors such as diabetes.
Stent Thrombosis: Blood Clot Formation
Stent thrombosis is a serious issue where a blood clot forms inside the stent. It can lead to a heart attack. The risk is highest in the first year after the stent is put in.
Prevention and Management:
- Dual antiplatelet therapy (DAPT) to prevent clot formation.
- Monitoring for signs of thrombosis.
- Lifestyle modifications to reduce cardiovascular risk.
Other Possible Complications
Other complications include:
- Bleeding complications due to antiplatelet therapy.
- Stent fracture or migration.
- Allergic reactions to stent materials.
It’s key for patients to know about these possible problems. Following their doctor’s advice can help lower the risks.
When Additional Stent Procedures May Be Necessary
There are times when more stent procedures are needed. Stents help with coronary artery disease for a long time. But, some situations require extra help.
Recurrent Symptoms Despite Stent Placement
Some patients might feel recurrent symptoms like chest pain or shortness of breath even with a stent. This could be because of in-stent restenosis, where the artery gets narrow again at the stent site.
These symptoms can also mean the disease is getting worse in other parts of the arteries. In such cases, more stent procedures might be needed to fix new blockages.
Progressive Coronary Artery Disease
Progressive coronary artery disease is another reason for more stent procedures. As the disease gets worse, new blockages can form in different parts of the arteries. This means more work is needed to keep the arteries open.
Many things can affect how fast the disease progresses. These include lifestyle choices, how well you take your medicine, and your overall health. It’s important to manage these factors to slow down the disease.
Stent Failure Scenarios
Stent failure can happen in a few ways, like stent thrombosis (blood clot in the stent) or in-stent restenosis. When this happens, more procedures might be needed to get blood flowing right again.
Stent failure shows how key ongoing monitoring and follow-up care are after getting a stent. Regular visits to your healthcare provider can catch problems early.
The Process of Stent “Replacement”
Replacing a heart stent is a detailed process. It often means adding new stents, not taking out the old ones. This is because dealing with coronary artery disease is complex. Stent implantation also plays a big role.
Adding New Stents vs. Removing Old Ones
When a stent is seen as a problem or symptoms come back, adding a new stent is usually the best choice. Removing a stent is risky and often not needed. Doctors first check the artery and stent’s condition before deciding what to do next.
Key considerations for adding new stents include:
- The condition of the artery and the existing stent
- The severity of the symptoms or the blockage
- The patient’s overall health and medical history
Why Cardiac Stents Are Rarely Removed
Cardiac stents are rarely taken out because removing them is complex and risky. Over time, stents become part of the artery wall. This makes removal hard without harming the artery.
The reasons for not removing stents include:
- The stent becomes part of the arterial wall
- Removal can cause arterial damage or thrombosis
- The risks associated with removal often outweigh the benefits
Techniques for Managing Problematic Stents
Dealing with problematic stents involves medical therapy and other treatments. Doctors might use drug-eluting balloons, add more stents, or try other catheter-based treatments. These methods help with issues like in-stent restenosis or stent thrombosis.
| Technique | Description | Indications |
| Drug-Eluting Balloons | Balloon angioplasty with drug coating to prevent restenosis | In-stent restenosis, small vessel disease |
| Additional Stenting | Placing a new stent within or alongside the existing one | Stent thrombosis, significant restenosis |
| Catheter-Based Treatments | Various minimally invasive procedures to address stent issues | Stent failure, complex coronary disease |
In conclusion, replacing a stent is a complex process. It usually means adding new stents or using other treatments, not removing the old one. Understanding these steps is key for both doctors and patients to manage coronary artery disease well.
Advancements in Stent Technology and Longevity
Stent technology has changed a lot, making treatments better and safer. New stents last longer and have less chance of failing. This is thanks to recent big steps forward.
Evolution of Stent Materials and Design
Stents used to be made of simple materials. Now, they’re made from better stuff that’s more friendly to the body. They’re also more flexible and strong.
Key advancements include:
- Improved metal alloys for better biocompatibility
- Enhanced stent designs for increased flexibility
- Drug-eluting coatings to reduce restenosis
Drug-Eluting Stents and Reduced Restenosis Rates
Drug-eluting stents (DES) have been a big win. They release medicine that stops cells from growing too much. This makes stented arteries stay open longer.
| Stent Type | Restenosis Rate | Primary Benefit |
| Bare-Metal Stents | 20-30% | Simple design, lower initial cost |
| Drug-Eluting Stents | 5-10% | Significantly reduced restenosis rates |
Future Innovations in Stent Technology
The future of stents is exciting. Scientists are working on new materials, designs, and coatings. Some ideas include:
- Bioresorbable stents that dissolve over time
- Stents with new drug coatings for improved efficacy
- Advanced imaging techniques for better stent placement
As research keeps going, we’ll see even better stents. They’ll help patients more in fighting coronary artery disease.
How Often Should a Heart Stent Be Checked?
Keeping an eye on a heart stent is key to heart health after a procedure. After getting a heart stent, it’s important for patients to stick to a follow-up plan. This ensures the stent works right.
Recommended Follow-up Schedule After Stent Placement
The timing for follow-ups after stent placement can change based on several factors. These include the stent type and the patient’s health. Usually, doctors suggest a first visit within a few months, followed by regular check-ins.
- Initial follow-up: 1-3 months post-stent placement
- Subsequent follow-ups: every 6-12 months
Diagnostic Tests Used to Monitor Stent Function
There are several tests to check how well a heart stent is working. These include:
| Diagnostic Test | Purpose |
| Stress Test | Checks heart function when stressed |
| Coronary Angiography | Looks at the coronary arteries and stent |
| Cardiac CT Scan | Shows detailed images of the heart and stent |
Signs That Warrant Immediate Medical Attention
People with heart stents should know when to get help fast. This includes:
- Chest pain or discomfort
- Shortness of breath
- Dizziness or fainting
Lifestyle Factors That Affect Stent Performance
Heart stents work better when patients manage their lifestyle well. After getting a stent, it’s important to take care of your heart health.
Medication Adherence and Its Importance
Medication adherence is key for stent success. Patients need to take antiplatelet therapy to avoid blood clots. Sticking to the medication plan helps prevent serious problems like in-stent restenosis or stent thrombosis.
To follow your medication plan well, you should:
- Know why you’re taking your meds and what side effects they might have
- Take your meds at the same time every day
- Use reminders like pill boxes or apps to stay on schedule
- Talk to your doctor about any issues or questions you have
Diet and Exercise Recommendations
Eating right and exercising are important for stent patients. A diet full of fruits, veggies, whole grains, and lean proteins helps with weight, blood pressure, and cholesterol.
Here are some diet tips:
- Stay away from bad fats and cholesterol
- Don’t eat too much sodium, aim for less than 2,300 milligrams a day
- Eat more omega-3s from fish and nuts
- Avoid too much sugar and refined carbs
Exercise like walking, cycling, or swimming is good for your heart. Talk to your doctor to create a workout plan that’s right for you.
Risk Factor Management for Stent Patients
Managing risk factors is key to keeping your stent working well. Important risk factors include:
| Risk Factor | Management Strategy |
| High Blood Pressure | Check your blood pressure often, take your meds, stay at a healthy weight, and watch your sodium. |
| High Cholesterol | Eat healthy, exercise, and take meds for cholesterol as told. |
| Smoking | Try to quit with help from groups, counseling, and nicotine therapy if needed. |
| Diabetes | Control your blood sugar with diet, exercise, and meds, and check it often. |
Controlling these risk factors can make your stent last longer and work better.
Special Considerations for Different Patient Populations
Managing heart stents isn’t a one-size-fits-all job. It needs a look at each patient’s special needs. Different groups face unique challenges, so a custom plan is key for the best results.
Elderly Patients with Stents
Elderly patients often have more health issues and a higher risk of problems. Careful medication management is very important. This is because older adults can be more affected by certain medicines.
A study in the Journal of the American College of Cardiology showed a benefit. Older adults with heart disease and stents did better with a detailed geriatric assessment.
Patients with Multiple Stents
Those with multiple stents need closer monitoring. They face a higher risk of issues like restenosis and thrombosis. This might mean more check-ups and tests.
| Risk Factor | Management Strategy |
| In-stent restenosis | Regular angiographic follow-up, medication adherence |
| Stent thrombosis | Dual antiplatelet therapy, lifestyle modifications |
Stents in Patients with Other Medical Conditions
Patients with other health issues, like diabetes or kidney disease, need a team effort. Coordination between cardiologists and other specialists is vital for their care.
For example, those with diabetes might need tighter control of their blood sugar. This can help prevent stent problems.
In summary, handling heart stents for various patient groups needs a deep understanding of their specific needs. A patient-focused approach helps improve care and life quality for these patients.
Conclusion: The Lifetime Commitment of Heart Stents
Managing heart stents is a lifelong journey that needs constant care and following doctor’s advice. Heart stents are not just a quick fix but a long-term effort to keep the heart healthy.
The life of a heart stent depends on many things. These include the type of stent, the patient’s health, and their lifestyle. By knowing these factors and working with doctors, people can make their stents work better and avoid problems.
Staying committed to heart health means regular check-ups, tests, and healthy living. This means eating right, exercising often, and taking medicines as told. By focusing on heart health, those with stents can live full and active lives.
In the end, managing heart stents is a team effort. It needs patients, doctors, and a dedication to long-term care. By making this commitment, people can improve their heart health and feel better overall.
FAQ
Does a stent have to be replaced?
Stents are usually meant to stay in the body forever. But, sometimes, more stents are needed because of problems or if the disease gets worse.
How long do stents last in arteries?
Stents are made to last a long time, often for life. But, how long they last can change based on the person’s lifestyle and health.
Can stents be removed and replaced?
Taking out stents is rare because it’s a tricky and risky procedure. Instead, doctors might put in more stents to fix issues or if the disease gets worse.
What is the lifespan of a stent?
Stents are made to last a long time. Newer stents are even better and less likely to cause problems.
How often should a heart stent be checked?
How often you need to see a doctor depends on your health and history. But, people with stents usually need to visit their cardiologist often.
Can heart stents be removed?
Taking out a heart stent is rare and only done in special cases. It’s usually when the stent is causing big problems.
Are stents permanent?
Yes, stents are meant to stay in the body forever. They are designed to be there for the rest of your life.
Can cardiac stents be removed?
Removing cardiac stents is rare because of the risks. Usually, doctors deal with problems by adding more stents or other treatments.
How long are heart stents good for?
Heart stents are made to last a long time. With the right care and management, they can keep working well.
How long will a stent last?
How long a stent lasts depends on many things. The type of stent, your health, and lifestyle all play a part. Most stents are made to last for years.
Can stents be replaced?
Stents aren’t usually “replaced” in the usual sense. But, doctors might put in more stents to handle complications or disease growth.
References
- Gada, H., et al. (2024). Sex and age-specific 10-year mortality after coronary stenting. European Heart Journal Open. https://academic.oup.com/ehjopen/article/5/1/oeaf006/7986101