Sickle cell anemia does not only affect people of African descent. It’s a genetic disorder that can affect people of many ethnic backgrounds, including those with European ancestry. In fact, many people ask, “do white people get sickle cell? The answer is yes ” while it is less common, sickle cell disease can still appear in individuals of white or mixed heritage if they inherit the gene from both parents.
Many think sickle cell anemia only affects certain groups, but genetic diversity and mixed heritage have made it present in populations worldwide. Knowing the genetics behind sickle cell anemia helps clear up these myths. It also makes sure everyone understands their risk, no matter their background.
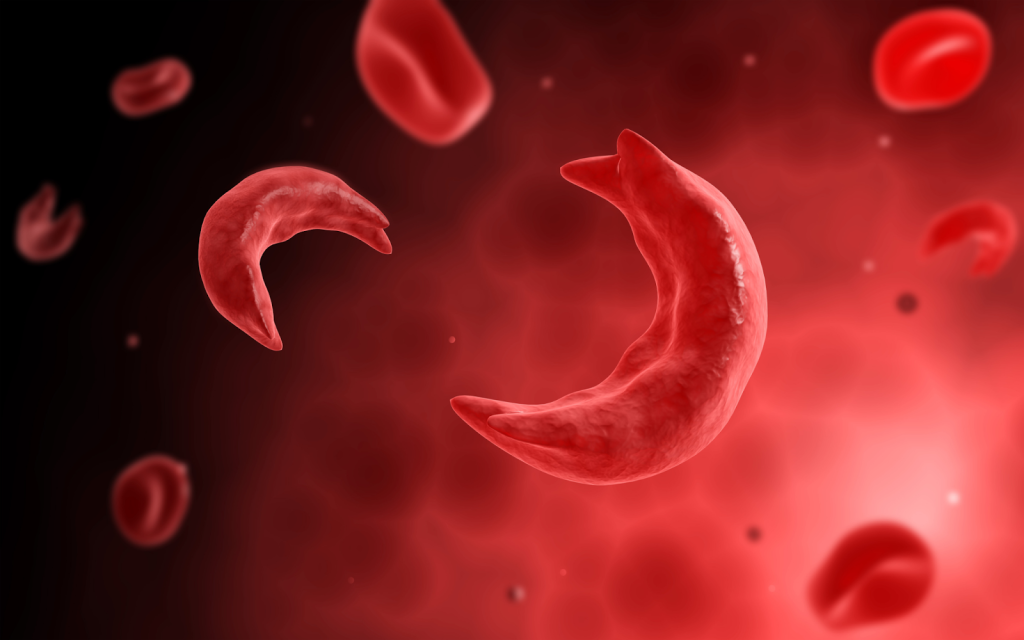
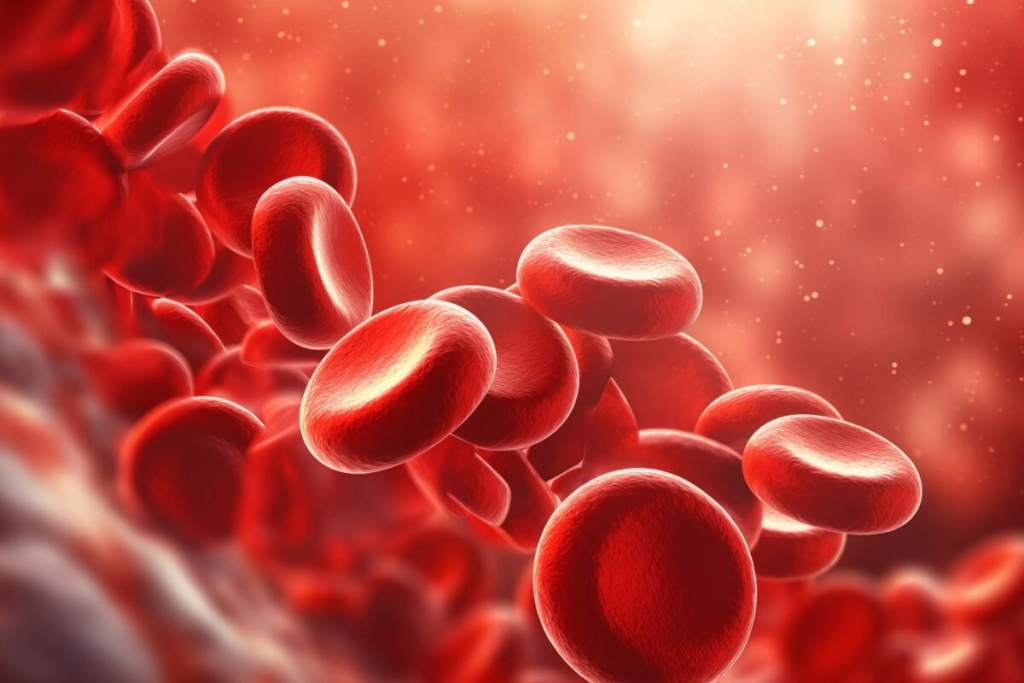
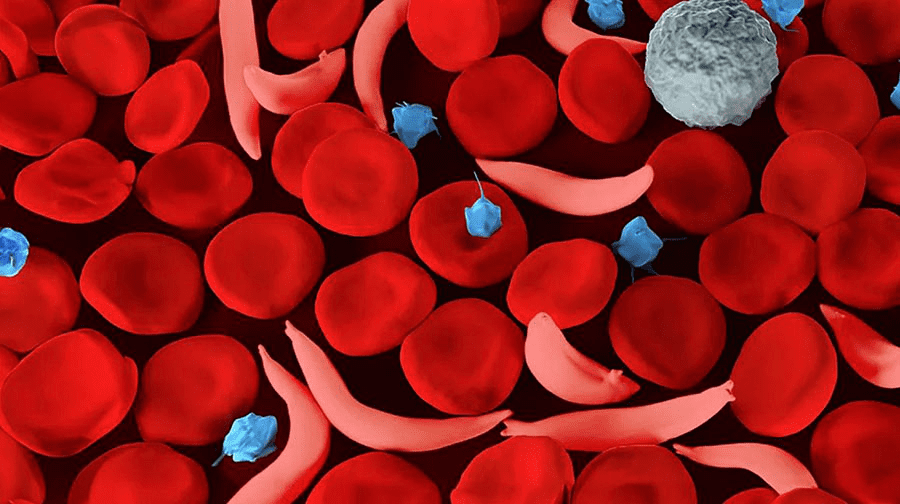
Sickle cell anemia is a genetic disorder that affects how red blood cells are made. It causes these cells to be misshapen. This happens because of abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
The mutation of the HBB gene is what causes sickle-shaped blood cells. This gene codes for a part of hemoglobin. When it mutates, a change in the beta-globin chain happens, leading to sickle hemoglobin.
Under low oxygen levels, this abnormal hemoglobin can join together. This causes red blood cells to bend into a sickle shape. This change is not just about shape; it affects how well the cells work and how long they last.
Normally, red blood cells are flexible and can easily move through blood vessels. But sickled cells are stiff. They can get stuck in small vessels, causing health problems.
Sickle cell anemia has many effects on the body. It mainly happens because sickled red blood cells block small blood vessels. This can cause pain crises and serious problems like stroke and acute chest syndrome.
It also makes infections more likely, mainly in children. This is because the spleen doesn’t work well. The spleen helps fight infections.
People with sickle cell anemia often have anemia. This is because their red blood cells don’t last long. They get destroyed in the spleen. Anemia can make you feel tired, weak, and can cause other problems.
Understanding sickle cell anemia’s genetics is key. It’s caused by a mutation in the HBB gene. This mutation makes abnormal hemoglobin, known as sickle hemoglobin or HbS.
The disease follows an autosomal recessive pattern. This means you need two copies of the mutated gene to have the disease. Carriers have one normal and one mutated gene. They don’t show all symptoms but can pass the mutated gene to their kids.
The inheritance of sickle cell anemia is complex. It involves many genetic factors. When both parents carry the sickle cell trait, there’s a:
This shows why genetic counseling is vital for families with sickle cell history.
Sickle cell anemia is more common in some groups, like those of African descent. But it can happen in anyone. Different groups may have different sickle cell gene mutations or variations.
In some Mediterranean and Middle Eastern groups, the sickle cell gene is more common. This is because it helps protect against malaria. This shows the genetic diversity of sickle cell anemia and why awareness is important across ethnic groups.
In summary, sickle cell anemia’s genetics are complex. Knowing these genetics is vital for diagnosing, managing, and preventing the disease.
The history of sickle cell anemia is a story of gradual discovery and evolving understanding. This genetic disorder affects how the body makes hemoglobin. It has been studied for over a century.
In 1910, James Herrick first identified the disease. He noticed sickle-shaped red blood cells in a patient. This discovery started the research into the condition.
Key Findings in the Early 20th Century
Over the years, our understanding of sickle cell anemia has grown a lot. Research has looked into its clinical presentation, genetic mutations, and the populations affected.
| Year | Milestone | Significance |
| 1910 | First identification by James Herrick | Marked the beginning of research into sickle cell anemia |
| 1920s | Understanding of genetic basis | Laid the groundwork for future genetic research |
| 1940s-1950s | Development of electrophoresis | Enabled the identification of abnormal hemoglobin |
The history of sickle cell anemia shows how far we’ve come in understanding and managing it. More research is needed to find better treatments and improve patient care.
Sickle cell anemia can happen to anyone, including white people. This might surprise many, as it’s often linked to certain ethnic groups. But, sickle cell anemia’s genetic roots mean it can affect anyone.
The genetics of sickle cell anemia involve a mutation in the HBB gene. This mutation causes abnormal hemoglobin, known as sickle hemoglobin or HbS. If someone has two copies of this mutated gene, they might get sickle cell anemia.
This condition is more common in places where malaria used to be a big problem. The sickle cell trait helps protect against malaria. But, this mutation isn’t limited to any ethnicity.
In white populations, sickle cell anemia is less common. But, it’s important to remember that anyone can carry the sickle cell trait, no matter their ethnicity.
There are cases of sickle cell anemia in Caucasian people, mainly in areas with genetic mixing. For example, in the Mediterranean, like Greece and Turkey, there’s a higher rate of sickle cell anemia. This includes people of Caucasian descent.
Medical records and studies show white individuals with sickle cell anemia. This shows why doctors should consider this diagnosis for anyone, not just based on ethnicity.
Sickle cell anemia is found in different ethnic groups, but its frequency varies. It’s a genetic disorder that affects red blood cells, making them sickle-shaped. This condition is not exclusive to any ethnic group, but it’s more common in some.
In the United States, sickle cell anemia is most common among African and African Americans. About 1 in 500 African Americans has the disease. The sickle cell trait, which can carry the disease, affects about 1 in 12 African Americans.
In Mediterranean countries like Greece and Turkey, sickle cell disease is also prevalent. It’s also found in the Middle East and India, often in specific ethnic or tribal groups. For example, in some Indian communities, the sickle cell trait’s prevalence can reach 30%.
While less common, sickle cell disease can occur in White or Caucasian populations, mainly in those of Mediterranean descent. Though it’s much rarer than in African or African American populations, it’s important to remember that sickle cell disease isn’t exclusive to any ethnic group.
To show how sickle cell disease varies by ethnicity, here’s some data:
| Ethnic Group | Prevalence of Sickle Cell Disease | Prevalence of Sickle Cell Trait |
| African American | 1 in 500 | 1 in 12 |
| Mediterranean | Varied, up to 1 in 100 in some areas | Up to 20% |
| White/Caucasian (non-Mediterranean) | Rare, less than 1 in 1,000 | Rare, less than 1% |
This table shows how sickle cell disease and trait vary by ethnicity. Knowing these differences helps in planning public health efforts and raising awareness about the disease.
The sickle cell trait offers protection against malaria, a big plus in evolution. This is key to why it’s more common in some places.
The sickle cell trait changes red blood cells’ hemoglobin. This makes it hard for malaria parasites to live and grow. Research has shown that people with this trait get less severe malaria. This is why it’s more common in areas where malaria is common.
Studies have demonstrated that malaria parasites, like Plasmodium falciparum, find it harder to invade red blood cells in those with the sickle cell trait. This makes it easier for these people to survive in places where malaria is a big problem.
The sickle cell trait’s spread matches malaria’s history. In places like Africa, the Mediterranean, and the Middle East, it’s more common. Historical migration patterns have also helped spread it to other areas.
The trait isn’t just found in Africans; it’s also in people from other malaria-prone areas. As people moved, they took the sickle cell trait with them. This is why it’s found in many different ethnic groups.
Understanding the sickle cell trait’s benefits is key to knowing why it’s so widespread. It shows how genetics, environment, and disease interact.
Sickle cell anemia is not just a disease of African Americans. It affects people from many ethnic backgrounds. This shows the disease is not limited to one group.
The idea that sickle cell anemia is a “black disease” is wrong. It’s true that it’s common in people of African descent. But it also affects those from Mediterranean, Middle Eastern, and Indian backgrounds.
Genetic diversity is key in sickle cell disease. It’s caused by a mutation in the HBB gene. This mutation is not unique to any ethnic group.
Some think sickle cell disease is always severe. Others believe having the sickle cell trait means you have the disease. But, the disease’s severity varies, and having the trait doesn’t mean you have it.
| Myth | Reality |
| Sickle cell anemia is only found in black people. | While more prevalent in African Americans, it affects diverse ethnic groups. |
| Having sickle cell trait means you have the disease. | Individuals with the trait are carriers but typically do not have the disease. |
| Sickle cell anemia is always severe. | The severity varies among individuals; some experience mild symptoms. |
It’s important to know the truth about sickle cell anemia. This helps clear up myths. It ensures everyone, no matter their ethnicity, gets the right care.
Ethnic misconceptions about sickle cell anemia cause big problems. People think it mainly affects those of African descent. This makes others unaware of its presence in other groups.
One big issue is delayed or missed diagnoses in non-African groups. Doctors might overlook sickle cell anemia in patients from other backgrounds. This can lead to late treatment and serious health problems.
A study found Caucasian patients were often misdiagnosed or faced long delays. This was because they thought sickle cell anemia was a “Black disease.” This not only harms the patient but also keeps the myth alive.
The belief that sickle cell anemia mainly affects Africans also skews research funding. Less money goes to studying it in other groups. This means there are fewer treatments for different patients.
Also, not enough research on non-African populations keeps the myth going. It’s key for researchers to tackle these issues. This way, everyone gets fair healthcare, no matter their ethnicity.
Understanding how to diagnose sickle cell anemia is key for early treatment. It involves both clinical checks and lab tests.
Blood tests are the main way to find sickle cell anemia. These tests look for sickle-shaped red blood cells or the genetic cause of the disease.
Common diagnostic tests include:
Even though sickle cell anemia is common in some groups, testing is important for anyone with symptoms or a family history. It doesn’t matter what ethnicity you are.
| Risk Factors | Symptoms to Watch For |
| Family history of sickle cell anemia | Recurring episodes of pain |
| Belonging to an ethnic group with high prevalence | Anemia and jaundice |
| Presence of sickle cell trait | Frequent infections |
Getting a correct diagnosis is the first step to managing sickle cell anemia. Anyone with symptoms or risk factors should get tested, no matter their ethnicity.
It’s important to know the symptoms and complications of sickle cell disease to manage it well. This genetic disorder affects how red blood cells make hemoglobin. It makes them bend into a sickle shape.
Symptoms of sickle cell disease vary, but some are common across ethnic groups. People often have pain episodes, or crises, when sickled cells block blood vessels. They might also feel tired, have jaundice, and get sick more easily because their spleen doesn’t work right.
Sickle cell disease can cause serious problems like stroke, acute chest syndrome, and spleen issues. Over time, it can harm organs like the kidneys, liver, and heart. This is because of chronic anemia and repeated blockages in blood vessels.
To manage the disease, a team of doctors, nurses, and specialists is needed. They provide regular check-ups, pain management, and sometimes blood transfusions.
Understanding the long-term effects of sickle cell disease helps healthcare teams offer better support. This improves how well patients do in the long run.
The treatment for sickle cell anemia is getting better. New therapies are being added to old ones, aiming for better results.
Today, doctors focus on easing symptoms and preventing problems. Pain management is key, using medicines and other methods to help with pain.
Blood transfusions are also important. They increase normal red blood cells, reducing risks. Regular transfusions help those with severe cases a lot.
| Treatment Approach | Description | Benefits |
| Pain Management | Use of medications and other interventions to manage pain | Reduces frequency and severity of pain crises |
| Blood Transfusions | Transfusion of normal red blood cells to reduce sickled cells | Decreases risk of complications, improves oxygen delivery |
| Hydroxyurea Therapy | Medication that reduces frequency of pain crises and complications | Decreases frequency of painful crises, reduces need for transfusions |
New treatments are being explored for sickle cell anemia. Gene editing technologies, like CRISPR/Cas9, might fix the disease’s cause.
Researchers are also looking at new medicines to lessen pain and improve health. Clinical trials are underway to check if these treatments work well.
As research moves forward, sickle cell anemia treatment will likely get even better. This brings new hope to those dealing with this condition.
Genetic counseling is key in helping people grasp their sickle cell disease risk. It looks at family history and genetics. This way, counselors give parents-to-be the info they need for family planning.
To grasp the risk of passing on sickle cell disease, knowing the genetics is vital. Sickle cell disease comes from a gene mutation in the HBB gene. If both parents carry this mutated gene, there’s a 25% chance with each pregnancy that the child will have sickle cell disease. Genetic counseling helps spot carriers and figure out disease passing risk.
The process includes:
Parents-to-be with sickle cell gene can look at several choices:
Genetic counseling offers a place for parents-to-be to talk about their choices. They can make decisions that fit their needs.
By knowing their risk and looking at options, families can handle sickle cell disease better. They can make smart choices about their reproductive health.
The fight against sickle cell anemia is not just about medical treatment. It also involves awareness and advocacy. This genetic disorder affects millions worldwide. Understanding and addressing its needs requires a broad approach.
Many organizations focus on raising awareness and supporting those with sickle cell anemia. For example, the Sickle Cell Disease Association of America advocates for those affected. They provide resources and support to families and individuals.
Support groups, both online and in-person, offer a community for those affected. They can share their experiences and find solidarity.
“Support groups have been a lifeline for our family,” says a parent of a child with sickle cell anemia. “We’ve connected with others who understand what we’re going through, and it’s been incredibly helpful.”
“The power of community is vital in the fight against sickle cell anemia.”
September is Sickle Cell Awareness Month. During this time, organizations and communities come together to educate the public. They run awareness campaigns, fundraising events, and educational programs.
Social media campaigns are also used to spread awareness. Hashtags like #SickleCellAwarenessMonth help reach more people. These efforts are key in dispelling myths and highlighting the need for research and support.
By raising awareness and supporting advocacy, we can work towards a better future. A future where individuals with sickle cell anemia get the understanding, care, and support they deserve.
Understanding sickle cell anemia needs a full approach. It shows it’s not just in certain groups. It can affect people from many backgrounds.
To break down barriers, we must see the disease’s genetic roots. It’s found in many ethnic groups. This knowledge helps us be more inclusive in awareness and support.
In the end, sickle cell disease knows no ethnic bounds. We must keep researching and educating. This ensures everyone gets the care they need, no matter their background.
By understanding sickle cell anemia better, we help those affected. This creates a supportive space. It’s a step towards better lives for those with the condition.
Yes, white people can get sickle cell anemia. It’s more common in certain groups, like African Americans.
No, sickle cell anemia isn’t just for black people. It’s more common in people of African descent. But, it can also be found in people of Mediterranean, Middle Eastern, and Indian descent, as well as in white people.
Sickle cell anemia comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation leads to sickle hemoglobin or HbS.
Sickle cell anemia is inherited in an autosomal recessive way. This means you need two copies of the mutated HBB gene to have the disease. You get one from each parent.
Yes, a white person can carry the sickle cell trait. This happens if they have one copy of the mutated HBB gene.
Sickle cell anemia is most common in people of African descent. It affects about 1 in 500 African Americans. It’s also found in people of Mediterranean, Middle Eastern, and Indian descent. And it can occur in white people, but much less often.
Sickle cell anemia is more common in certain groups because of an evolutionary advantage. The sickle cell trait helps protect against malaria in areas where it’s common.
Doctors use blood tests to diagnose sickle cell anemia. These include hemoglobin electrophoresis and genetic testing.
Symptoms of sickle cell anemia vary. They can include pain episodes, anemia, infections, and a higher risk of stroke.
Yes, new treatments are being researched for sickle cell anemia. These include gene therapy and medications to manage the disease.
Yes, genetic counseling can help people understand their risk. It guides them on reproductive choices and family planning.
Advocacy groups are key in raising awareness about sickle cell anemia. They promote education and support individuals and families affected by the disease.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us