Does Blood Work Show Cancer? New medical tech has made it easier to find cancer with blood tests. Almost half of people will get cancer at some point. Finding it early is key to treating it well.
We’re on the verge of a big change in finding cancer. Cancer detection through blood tests is getting better. These tests can spot different cancers early, giving us a chance to act fast.
The role of blood tests for cancer screening is huge. Finding cancer early can greatly improve treatment results and survival rates.
Key Takeaways
- Cancer detection through blood tests is becoming increasingly accurate.
- Early detection significantly improves treatment outcomes.
- Blood tests can identify various types of cancer before symptoms appear.
- Advancements in medical technology are continually improving cancer screening.
- Simple blood tests can provide critical information for cancer diagnosis.
The Basics of Blood Tests and Cancer Detection

Blood tests are key in finding cancer early. Knowing how they work is vital for spotting problems. These tests help find cancer before it’s too late.
How Cancer Affects Blood Composition
Cancer changes blood in many ways, making tests very useful. For example, it can mess with bone marrow, affecting blood cell levels. A complete blood count (CBC) checks these levels.
When cancer is there, it can change these counts. Leukemia, for instance, can raise white blood cells too high. Some cancers lower red blood cells, causing anemia.
Types of Blood Tests Used in Cancer Screening
There are many blood tests for cancer screening, each with its own job. The CBC can show many health issues, including cancer. Tumor markers look for proteins or enzymes from cancer cells.
- Leukemia blood tests find abnormal white blood cells or genetic changes linked to leukemia.
- Lymphoma blood tests check for proteins or cells that might mean lymphoma.
- Cancer screening tests, like blood tests, aim to find cancer early, before symptoms show.
It’s important to know about different blood tests and their uses. This helps us screen for cancer better. By picking the right tests for each person, we can catch cancer sooner.
Complete Blood Count (CBC): The First Line of Investigation
The Complete Blood Count (CBC) is a key test for finding cancer. It checks the numbers of different blood cells. These include red blood cells, white blood cells, and platelets.
A CBC shows how healthy your blood is. It can spot problems that might mean cancer. Knowing what a CBC shows helps doctors figure out what to do next.
Red Blood Cell Abnormalities
Red blood cells carry oxygen. If there’s not enough, it’s called anemia. This can mean there’s a health problem, like cancer.
Some cancers, like colon cancer, can cause anemia. Leukemia can also mess with red blood cell making in the bone marrow. So, a CBC can help find anemia and lead to more tests.
White Blood Cell Count Changes
White blood cells fight infections. Changes in their count can mean different health issues, including cancer. A high count, or leukocytosis, might mean infection or leukemia.
A low count, or leukopenia, makes you more likely to get sick. This can happen in people getting chemo or with bone marrow problems, like cancer.
Platelet Level Variations
Platelets help blood clot. Problems with their count can mean health issues, including cancer. A low count, or thrombocytopenia, can make bleeding more likely. This is common in leukemia.
A high count, or thrombocytosis, can happen with inflammation or some cancers. It’s important to know why platelet counts change to decide the best treatment.
Does Blood Work Show Cancer? Understanding Detection Capabilities
Cancer detection through blood tests is a field that’s growing fast. It has both good and bad sides. We need to know what signs blood work can show and its limits.
What Cancer Signs Can Blood Work Reveal
Blood tests can show signs of cancer in some cases. For example, certain proteins or tumor markers in the blood can point to specific cancers. Tumor markers are substances found in higher amounts in the blood, urine, or tissues of some patients with certain types of cancer. These include PSA for prostate cancer and CA-125 for ovarian cancer.
Also, blood cell count changes, like an elevated white blood cell count, can suggest cancer or a precancerous condition.
Changes in blood enzyme or hormone levels can also hint at cancer. For example, an increase in LDH can be linked to various cancers, like lymphoma and leukemia. It’s key to look at both specific markers and the overall clinical picture.
Limitations of Standard Blood Tests
Even though blood tests offer useful info, they have big limits in finding cancer. Not all cancers release detectable amounts of tumor markers into the blood. Some markers can also be high for reasons not related to cancer, leading to false positives. This can cause unnecessary worry and more tests.
Early-stage cancers might not produce enough markers for standard blood tests to catch. This means some cancers might not be found early enough. A negative blood test doesn’t mean cancer is ruled out. Doctors often need to do more tests to confirm a diagnosis.
Tumor Markers: Specific Proteins in Cancer Detection
Tumor markers are substances made by cancer cells or in response to cancer. They play a key role in finding and tracking cancer. These markers can be proteins, enzymes, or molecules found in higher amounts in the blood, urine, or tissues of some cancer patients.
How Tumor Markers Work
Tumor markers show the presence of cancer cells or the body’s reaction to cancer. They help with screening, diagnosis, predicting outcomes, and tracking treatment success. For example, the Prostate-Specific Antigen (PSA) test is used for prostate cancer screening. High PSA levels in the blood might mean prostate cancer, but it’s not the only cause.
“The use of tumor markers has changed how we diagnose and manage cancer,” say cancer research experts. “These markers give us vital information for better patient care.”
Common Tumor Markers and Their Associated Cancers
Many tumor markers are linked to specific cancers. For example:
- PSA (Prostate-Specific Antigen): High levels suggest prostate cancer.
- CA-125: High levels often point to ovarian cancer, but can also rise in other conditions.
- CEA (Carcinoembryonic Antigen): This marker is linked to colorectal cancer, among others.
- AFP (Alpha-fetoprotein): High levels may mean liver cancer or certain germ cell tumors.
Reliability and Interpretation Challenges
While tumor markers are useful, they can be tricky to rely on. Not all cancers have specific markers, and some markers can be high in non-cancerous conditions. So, tumor marker tests are often used with other diagnostic tools like imaging and biopsies to confirm a diagnosis.
It’s also key to know that some people might have high tumor marker levels without cancer, known as a false positive. On the other hand, some cancer patients might have normal marker levels, known as a false negative. Understanding these challenges is vital for accurate tumor marker test results.
Blood Tests for Detecting Specific Cancers
Certain cancers can be found through specific blood tests. These tests look for tumor markers in the blood. They are key in finding and managing cancers early.
Prostate Cancer and PSA Testing
The Prostate-Specific Antigen (PSA) test is used to find prostate cancer. It checks the PSA levels in the blood. High levels might mean prostate cancer, but other issues can also raise them.
PSA Test Guidelines:
- Men aged 50 and above should get a PSA test.
- Those with a family history of prostate cancer might start testing earlier.
- The test alone can’t confirm cancer; more tests are needed.
Ovarian Cancer and CA-125 Test
The CA-125 test looks for the CA-125 protein in the blood. It’s often high in women with ovarian cancer. Though not specific, it helps track ovarian cancer in those with a history of it.
“The CA-125 test is not a definitive diagnostic tool but is used in conjunction with other diagnostic methods to monitor ovarian cancer.”
CA-125 Test Considerations:
| CA-125 Level | Interpretation |
| Normal | Less than 35 U/mL |
| Elevated | Above 35 U/mL; may indicate ovarian cancer or other conditions |
Colorectal Cancer and CEA Marker
The Carcinoembryonic Antigen (CEA) test checks for CEA levels. This protein is high in colorectal cancer and some other cancers. It’s mainly used to see how the disease is doing and how it’s responding to treatment.
Liver Cancer and AFP Tumor Marker
The Alpha-Fetoprotein (AFP) test looks at AFP levels. This protein is made by the liver and yolk sac in fetuses. High levels in adults might mean liver cancer or other cancers. It’s used with imaging tests to diagnose liver cancer.
AFP Test Interpretation:
- Normal levels are typically less than 10 ng/mL.
- Levels above 400 ng/mL can indicate liver cancer.
- The test is not diagnostic on its own and requires further investigation.
In conclusion, specific blood tests are key in finding different cancers. Knowing about tumor markers and their tests helps in early detection and management of cancers.
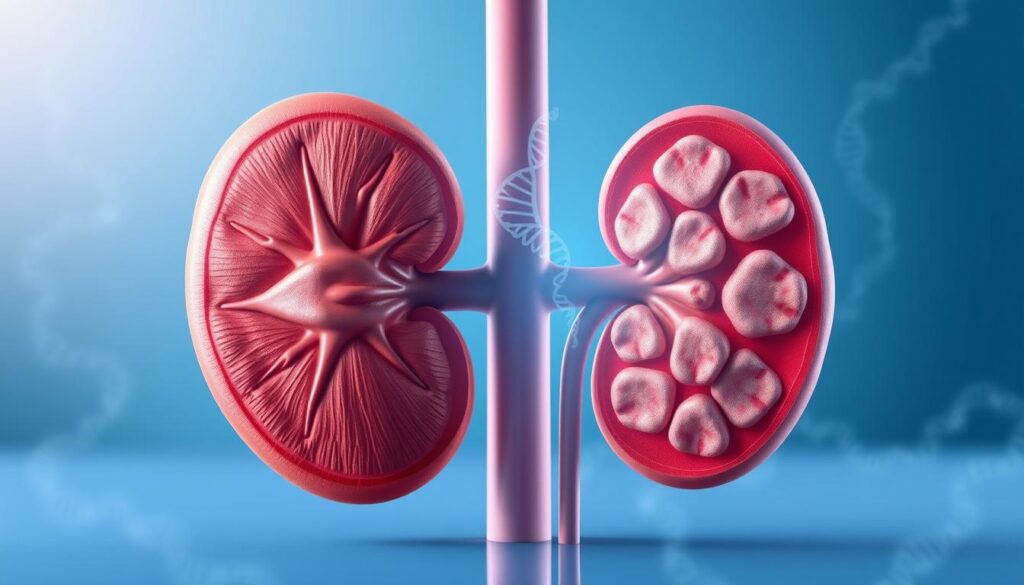
Blood Cancers and Their Diagnostic Indicators
Diagnosing blood cancers like leukemia, lymphoma, and multiple myeloma involves blood tests. These tests look for certain patterns and markers. Blood cancers mess with how blood cells are made and work. Certain signs can be found in blood tests.
Leukemia Blood Test Patterns
Leukemia makes white blood cells grow too much. Blood tests show if there are too many or too few white blood cells. Tests can also find specific markers and genetic changes that point to certain types of leukemia.
Key indicators of leukemia in blood tests include:
- Abnormal white blood cell count
- Presence of blast cells
- Specific genetic markers
Lymphoma Detection Through Blood Work
Diagnosing lymphoma with blood tests looks for odd lymphocytes and markers. While a biopsy is often needed, blood tests can give early clues. For example, high levels of lactate dehydrogenase (LDH) might suggest lymphoma.
Important blood test findings in lymphoma include:
- Elevated LDH levels
- Abnormal lymphocyte counts
- Presence of specific proteins or markers
Multiple Myeloma Protein Markers
Multiple myeloma is when bad plasma cells grow in the bone marrow. Blood tests can spot the odd proteins (M-protein) these cells make. Finding and measuring M-protein is key for diagnosing and tracking multiple myeloma.
Diagnostic indicators for multiple myeloma include:
| Marker | Description | Significance |
| M-protein | Abnormal immunoglobulin protein | Diagnostic hallmark |
| Free light chains | Abnormal light chain proteins | Indicator of disease activity |
| Beta-2 microglobulin | Protein associated with myeloma cells | Prognostic factor |
Blood tests are vital for diagnosing and keeping track of blood cancers. They help doctors spot leukemia, lymphoma, and multiple myeloma. This lets them plan the right treatment.
Inflammatory Markers and Their Role in Cancer Diagnosis
Inflammation is a complex response that can be linked to cancer. Markers like ESR and CRP help in diagnosing the disease. Cancer can trigger inflammation in the body, leading to the production of proteins and markers detectable through blood tests.
ESR and CRP Inflammation Indicators
ESR and CRP are two common inflammatory markers. ESR measures how fast red blood cells settle in a test tube. CRP is a liver protein produced in response to inflammation. High levels of these markers may suggest inflammation linked to cancer.
In Hodgkin lymphoma, ESR levels are often high. CRP is also elevated in cancers like colorectal, lung, and breast. But, it’s important to remember that high ESR and CRP can also be due to other inflammatory conditions.
When Inflammation Suggests Cancer
Chronic inflammation can lead to cancer. In some cases, inflammation can be an early sign of cancer. For example, chronic pancreatitis increases the risk of pancreatic cancer.
When inflammatory markers are high, it’s key to investigate further, even more so if there’s a family history or exposure to carcinogens. A detailed diagnostic workup, including imaging and biopsies, may be needed to find the cause of inflammation.
Other Inflammatory Conditions That Mimic Cancer
Many non-cancerous conditions can also cause inflammation, making it seem like cancer. Infections, autoimmune diseases like rheumatoid arthritis, and chronic inflammatory conditions can all raise inflammatory markers. A thorough clinical evaluation is needed to tell if the inflammation is cancer-related or not.
In conclusion, markers like ESR and CRP are important in cancer diagnosis by showing inflammation. They are not definitive signs of cancer but can lead to further investigation. This is when they are considered with other clinical factors and diagnostic tests.
Common Abnormal Blood Test Results Associated with Cancer
Abnormal blood test results can signal many health issues, including cancer. Blood tests are key in finding problems in blood composition linked to cancer. We will look at common abnormal blood test results that might point to cancer.
Anemia and Its Connection to Cancer
Anemia means having too few red blood cells or low hemoglobin. It’s often seen in blood tests. It can be linked to cancers like leukemia or lymphoma, which affect the bone marrow. Anemia can also happen due to chronic diseases, including cancer, that cause inflammation and affect red blood cell production.
Key signs of anemia include:
- Fatigue and weakness
- Shortness of breath
- Pale skin
High Calcium Levels as a Warning Sign
High calcium levels in the blood, known as hypercalcemia, can signal cancer. This usually happens when cancers produce a hormone that raises calcium levels. Lung, breast, and multiple myeloma cancers are often linked to high calcium levels.
Abnormal Liver Enzymes and Cancer Risk
Liver enzymes like ALT and AST are tested to check liver health. High levels can mean liver damage or disease, including cancer. Liver cancer or metastasis can also cause these enzymes to rise.
LDH Levels and What They Indicate
Lactate dehydrogenase (LDH) is found in many tissues like the liver, heart, and muscles. High LDH levels can show tissue damage or disease, including cancer. This is often seen in lymphoma and leukemia, as well as heart or liver problems.
It’s important to remember that abnormal blood test results don’t always mean cancer. More tests are needed to find the cause of these results.
Advanced Blood-Based Cancer Detection Technologies
New blood-based technologies are changing how we find and treat cancer. These advanced methods make finding cancer more accurate and quicker. This could lead to catching cancer early and improving treatment results.
Liquid Biopsy: Capturing Cancer DNA in Blood
Liquid biopsy is a new way to test for cancer without surgery. It looks for cancer DNA or biomarkers in the blood. This method could spot cancer early, track how well treatments work, and find out if cancer is resistant to treatment.
Key benefits of liquid biopsy include:
- It’s less invasive, so you don’t need surgery
- It lets doctors watch cancer changes in real-time
- It might find cancer coming back early
Circulating Tumor DNA Testing
Circulating tumor DNA (ctDNA) testing is a part of liquid biopsy. It looks for DNA bits from tumors in the blood. This helps find specific genetic changes linked to different cancers.
| Cancer Type | ctDNA Marker | Clinical Utility |
| Non-Small Cell Lung Cancer | EGFR mutation | Guiding targeted therapy |
| Colorectal Cancer | KRAS mutation | Predicting treatment response |
| Breast Cancer | PIK3CA mutation | Identifying possible treatment targets |
Emerging Blood Test Technologies
Researchers are also looking into new blood tests for cancer. These include:
- Studying extracellular vesicles and what they carry
- Finding cancer-specific proteins and metabolites
- Using artificial intelligence to analyze blood tests
As these technologies get better, we’ll see big changes in cancer care. The future of fighting cancer looks bright, thanks to these new blood tests. They offer hope for patients and doctors.
Cancer Screening Tests: Who Should Get Them and When
Cancer screening tests help find cancer early, when it’s easier to treat. They are based on age, risk factors, and health. It’s key to know who needs to get tested and when.
Current Screening Recommendations by Age and Risk
Screening guidelines group people by age and risk. For example, women at high risk for breast cancer might start screening at 40 or 45. For colon cancer, screening usually starts at 45 for those with average risk.
It’s important for doctors and patients to understand these guidelines. We’ll look at the current advice for different cancer screenings. We’ll talk about how age and risk affect these recommendations.
Risk-Based Testing Approaches
Risk-based testing looks at your unique risk factors. This includes genetic mutations, family history, and lifestyle. For instance, those with a BRCA1 or BRCA2 gene mutation face higher risks for breast and ovarian cancers. They might need more frequent or earlier screenings.
This approach helps target screenings to those at highest risk. It makes screenings more effective and less stressful for those at lower risk. We’ll see how this works for different cancers.
Cost-Benefit Analysis of Routine Screening
Looking at the cost and benefits of routine cancer screening is important. The benefits include finding cancer early, which can lead to better treatment and survival. But, screening can also cause false positives, anxiety, and extra tests.
We’ll look at the evidence on how effective different screenings are. We’ll talk about how they affect healthcare costs and patient results. This helps shape healthcare policies and personal choices.
False Positives and False Negatives: Understanding Test Accuracy
False positives and false negatives in blood tests can have big effects on patients getting cancer diagnosed. We must know what causes these mistakes and how they affect patients.
Why Blood Tests Sometimes Get It Wrong
Blood tests are not perfect. Many things can lead to false positives and false negatives. False positives mean a test says there’s cancer when there isn’t. False negatives mean a test misses cancer when it’s there.
Lab mistakes, when the test is done too early or too late, and the test’s sensitivity and specificity all play a part. These factors can make the test not as accurate as it should be.
Psychological Impact of False Results
The mental effects of false positives and negatives are big. A false positive can make people very anxious, leading to more tests that might be scary. On the other hand, a false negative can make people feel safe when they’re not, which can delay getting help.
People with false positives might have to go through more tests, which can be hard on their body and mind. False negatives can make people wait too long to get checked again, which can make things worse.
Follow-up Procedures After Inconclusive Results
When blood tests don’t give clear results, more steps are needed. This might include more blood tests, imaging studies, or even biopsies to check for cancer.
We help patients figure out what to do next after unclear results. This could mean more tests, watching them closely, or trying different ways to find out what’s wrong. Our aim is to make sure patients get the right diagnosis and treatment.
When to See a Doctor About Cancer Blood Testing
Knowing when to talk to a doctor about cancer blood tests is key. These tests can spot cancer early. They look for special signs in your blood linked to different cancers.
Symptoms That Warrant Immediate Testing
Some symptoms mean you should get tested right away. These include:
- Unexplained weight loss
- Persistent fatigue
- Changes in skin or moles
- Unusual bleeding or discharge
- Changes in bowel or bladder habits
If you notice any of these signs, see your doctor. They can talk about blood tests for cancer.
Risk Factors That Influence Testing Decisions
Some things can make your doctor think about blood tests for cancer. These include:
| Risk Factor | Description |
| Family History | A history of cancer in first-degree relatives |
| Genetic Predisposition | Presence of specific genetic mutations (e.g., BRCA1 and BRCA2 for breast and ovarian cancer) |
| Age | Increasing age, specially over 50 |
| Lifestyle Factors | Smoking, too much alcohol, and bad diet |
Talking about these risks with your doctor can help decide if blood tests are right for you.
Having Productive Conversations With Your Doctor
To get the most from your doctor’s visit, do the following:
- Write down your symptoms and when they started
- Share your family’s medical history
- Think about your lifestyle habits
- Make a list of questions for your doctor
Being open and ready can lead to a better talk with your doctor about cancer blood tests.
The Path From Abnormal Blood Test to Diagnosis
When blood tests show something’s off, we get more tests to find out why. Our doctors guide us through these steps. They help figure out what’s going on and what it might mean.
Follow-up Testing Procedures
After an abnormal blood test, additional blood tests are often ordered. These might include more specific tumor marker tests or detailed analyses of blood cell counts. For example, if a Complete Blood Count (CBC) shows abnormal white blood cell counts, further testing might be done to identify the cause of this abnormality.
We may also be asked to undergo other types of tests, such as urine analysis or genetic testing, depending on the initial findings and our overall health profile. These tests provide a more complete picture of our health status, helping healthcare providers narrow down possible causes.
Imaging Studies After Blood Test Results
Imaging studies are key in the diagnostic process after abnormal blood test results. Techniques such as X-rays, CT scans, MRI scans, or PET scans may be used to visualize internal organs and structures. These imaging tests can help identify abnormalities that may not be evident through blood tests alone, such as tumors or other structural changes.
For example, if blood tests indicate elevated liver enzymes, an imaging study like an ultrasound or CT scan might be used to examine the liver for signs of damage or disease. If there’s a suspicion of cancer, imaging tests can help locate tumors and assess their size and spread.
When Biopsies Become Necessary
In some cases, a biopsy may be necessary to obtain a definitive diagnosis. A biopsy involves taking a sample of tissue from the body, which is then examined under a microscope. This procedure can be very important when cancer is suspected, as it allows for the direct examination of cells to determine if they are malignant.
Biopsies can be performed using various techniques, depending on the location of the suspected abnormality. For instance, a needle biopsy might be used for liver or kidney abnormalities, while a surgical biopsy might be necessary for accessing tumors in harder-to-reach areas.
Interpreting Your Blood Test Results for Cancer Indicators
Getting your blood test results is a big moment for your health, like when you’re checking for cancer. Blood tests are key for spotting health issues and can find cancer early. But, it’s important to know what your results mean.
Understanding Reference Ranges
Reference ranges are the normal values for blood tests. They can change a bit between labs. If your results are within these ranges, it usually means everything is okay. But, results outside these ranges don’t always mean cancer.
“A result outside the reference range doesn’t necessarily mean you have cancer, but it may warrant further investigation.” Always talk to your doctor about your results to know what they mean.
Questions to Ask Your Doctor About Results
When you talk to your doctor about your blood test results, ask the right questions. Some important ones are:
- What do my test results indicate about my health?
- Are there any abnormal results that need further investigation?
- What are the next steps if my results suggest possible cancer indicators?
- Are there any lifestyle changes or treatments that I should consider based on my results?
These questions help you understand your results and what to do next.
Online Resources for Understanding Blood Work
There are many online resources to help you understand your blood test results. Health websites and medical groups offer detailed info on blood tests. Some good places to check out are:
- National Cancer Institute (NCI)
- American Cancer Society (ACS)
- Lab Tests Online
These sites can give you useful info on your blood test results and help you understand medical tests better.
The Future of Blood-Based Cancer Detection
The world of cancer detection is changing fast with new blood tests. Researchers keep finding new ways to spot and treat cancer. This is making a big difference in how we fight this disease.
Multi-Cancer Early Detection Tests
Multi-cancer early detection tests are a big deal. They can find many types of cancer from just one blood sample. This means catching cancer early, when it’s easier to treat.
These tests look at DNA and proteins in the blood. They can find cancer before symptoms show up. This is a huge step forward in cancer care.
Artificial Intelligence in Blood Test Analysis
Artificial intelligence (AI) is helping a lot with blood tests for cancer. AI can look through lots of data and find patterns humans might miss. This helps doctors make more accurate diagnoses and catch cancer early.
AI makes blood tests for cancer better. It helps cut down on false results. This means patients get more accurate answers and avoid extra tests and worries.
Personalized Blood Testing Based on Genetic Risk
The future also includes personalized testing based on your genes. Doctors can use your genetic info to suggest the right tests for you. This makes screening more targeted and effective.
This approach means catching cancer sooner in people at high risk. It also means less screening for those at lower risk. It’s all about making medicine more precise and effective for each person.
Conclusion: The Promise and Limitations of Blood Work in Cancer Care
Blood work is key in finding cancer, giving clues through different tests and markers. It has become more advanced, thanks to new tech like liquid biopsy and circulating tumor DNA testing.
Even though blood tests are helpful, we must know their downsides. They can sometimes show false results, leading to more tests to be sure. It’s important to see blood test results alongside other tests for a complete picture.
As we keep improving blood tests for cancer, they will stay a big part of cancer care. By knowing both the good and bad of blood work, we can find cancer sooner and treat it better.
FAQ
Can blood tests detect cancer?
Yes, some blood tests can spot cancer. These include tumor marker tests and complete blood counts (CBC). But, blood tests alone can’t confirm cancer. They’re often used with other tests like imaging and biopsies.
What are tumor markers, and how do they relate to cancer?
Tumor markers are substances found in higher amounts in some cancer patients. They can be made by the tumor or by the body’s response to it. This includes both cancer and some benign conditions.
What is a complete blood count (CBC), and how is it used in cancer detection?
A CBC measures different parts of the blood. It looks at red and white blood cell counts and platelet levels. Abnormal counts can hint at cancers like leukemia or lymphoma.
Can a CBC diagnose cancer?
A CBC can’t diagnose cancer on its own. But, it can suggest cancer might be present. For example, an odd white blood cell count could point to leukemia or lymphoma.
What are some common tumor markers used in cancer detection?
Common tumor markers include PSA for prostate cancer and CA-125 for ovarian cancer. CEA is used for colorectal cancer, and AFP for liver cancer. Each marker is linked to specific cancers.
Are tumor marker tests reliable for cancer diagnosis?
Tumor marker tests are useful for tracking treatment and spotting cancer return. But, they’re not always reliable for diagnosing cancer. This is because they can give false positives or negatives.
What is liquid biopsy, and how is it used in cancer detection?
Liquid biopsy is a blood test that finds tumor DNA in the blood. It helps diagnose and monitor cancer. It also offers insights into tumor genetics, helping guide treatment.
Who should undergo cancer screening tests, and when?
Who needs cancer screening tests depends on age, risk factors, and medical history. People at higher risk, due to family history or other factors, might start screening earlier.
What are the psychological impacts of false positive and false negative cancer test results?
False positives can cause worry and stress. False negatives can make people feel safe when they’re not. Both show the need to understand test limits and follow up with doctors.
How should I prepare for a conversation with my doctor about cancer blood testing?
To talk to your doctor well, know your risk factors and any symptoms. Ask about test benefits and limits. Discussing your worries and understanding screening schedules is key.
What are the next steps after receiving abnormal blood test results?
After abnormal results, your doctor might suggest more tests. This could be more blood tests, imaging studies, or a biopsy. These steps help find the cause of the abnormal results.
How can I understand my blood test results and reference ranges?
To get your blood test results, know the reference ranges for each test. Talk about any odd results with your doctor. Online resources can help, but always talk to a healthcare professional for personal advice.