Last Updated on December 3, 2025 by Bilal Hasdemir
Research is increasingly examining how ejaculation impacts prostate health, highlighting why understanding these effects is important for men considering or recovering from a robotic prostatectomy.
For patients undergoing robotic prostatectomy, discussions about sexual function, including ejaculation, are essential. Understanding how a robotic prostatectomy can affect these functions helps set realistic expectations for recovery.
Studies suggest that men who undergo robotic prostatectomy may experience changes in ejaculation patterns, and these changes can have implications for overall prostate health. By understanding the role of ejaculation before and after robotic prostatectomy, patients can make informed decisions and follow proper post-operative care.
Doctors specializing in robotic prostatectomy emphasize the importance of patient education on sexual and urinary health. Knowing how ejaculation affects prostate function can improve outcomes and overall quality of life after robotic prostatectomy.
Key Takeaways
- Frequent ejaculation may reduce the risk of prostate cancer.
- Robotic prostatectomy is a treatment option for an enlarged prostate.
- Understanding prostate health is vital for men’s well-being.
- The connection between ejaculation and prostate health is an area of ongoing research.
- Treatments like robotic prostatectomy can significantly impact prostate health.
The Connection Between Ejaculation and Prostate Health

Research is examining how ejaculation impacts prostate health, emphasizing the importance of understanding its role.
Research is examining how ejaculation impacts prostate health, emphasizing the importance of understanding its role.
Ejaculation involves the prostate gland in a complex way. The prostate gland is key to male health. Studies show that ejaculation might help clear out harmful substances and lower prostate cancer risk.
Mechanisms Behind Ejaculation’s Effect on Prostate Health
- The prostate gland makes fluids for semen, and ejaculation removes them.
- Regular ejaculation might lower harmful substance levels in the prostate.
- It could also reduce prostate inflammation.
Scientific Evidence on Ejaculation Frequency and Prostate Size
Studies have looked at how often ejaculation happens and prostate health. Some say frequent ejaculation might lower prostate cancer risk. But, the proof is not solid yet.
| Study | Ejaculation Frequency | Prostate Cancer Risk |
| Study A | High Frequency | Reduced Risk |
| Study B | Low Frequency | No Significant Reduction |
Limitations of Ejaculation as a Treatment Approach
Ejaculation might have benefits for prostate health, but it’s not a cure-all. Men with prostate problems should talk to their doctor about the best treatment.
It’s important to remember that results can vary. More research is needed to fully understand ejaculation’s impact on prostate health.
Understanding the Prostate Gland and Enlargement

Knowing about the prostate gland is key to dealing with its growth and Benign Prostatic Hyperplasia (BPH).
Anatomy and Function of the Prostate
The prostate gland is a small, walnut-sized organ below the bladder in men. It wraps around the urethra, the tube that carries urine. The prostate’s main job is to make seminal fluid, which helps and protects sperm during ejaculation. The health of the prostate gland is vital for men’s reproductive and urinary health.
The prostate gland has glandular, fibrous, and muscular tissues. The glandular tissue makes prostate fluid, a big part of semen. The fibrous and muscular tissues support the gland and help push semen out during ejaculation.
Causes of Benign Prostatic Hyperplasia (BPH)
BPH is when the prostate gland gets bigger. The exact reasons for BPH are not known, but hormonal changes with age are thought to be a big part. Specifically, the conversion of testosterone to dihydrotestosterone (DHT) is believed to play a significant role in the development of BPH.
- Aging: The risk of developing BPH increases with age.
- Hormonal changes: Changes in testosterone and DHT levels can lead to prostate enlargement.
- Genetics: Family history may play a role in the development of BPH.
Symptoms of an Enlarged Prostate
An enlarged prostate can cause many urinary symptoms because it presses on the urethra. Common symptoms include:
- Weak or interrupted urine flow
- Frequent urination, often at night
- Difficulty starting urination
- Dribbling of urine
The Urology Care Foundation says, “BPH is a common condition that affects many men as they age. Understanding the symptoms and seeking medical care can greatly improve quality of life.”
“Benign prostatic hyperplasia (BPH) is a condition in which the prostate gland is enlarged, causing various urinary symptoms. While the exact cause is unknown, it is believed to be related to hormonal changes with aging.”
Conventional Treatments for Enlarged Prostate
Men with an enlarged prostate have several treatment options. The right choice depends on how bad the symptoms are and how they affect daily life.
Medication Options for BPH
Medicines are often the first treatment for Benign Prostatic Hyperplasia (BPH). There are different types:
- Alpha-blockers: These relax the muscles in the prostate and bladder neck, making it easier to pee.
- 5-alpha-reductase inhibitors: These shrink the prostate gland, improving urine flow and reducing symptoms.
- Combination therapy: Mixing alpha-blockers and 5-alpha-reductase inhibitors can work well for some men.
Talking to a healthcare provider about the good and bad of these medicines is key.
Minimally Invasive Procedures
For those who don’t want to take medicine or it doesn’t work, there are less invasive options. These include:
- Transurethral microwave therapy (TUMT): Uses microwave energy to kill off extra prostate tissue.
- Transurethral needle ablation (TUNA): Uses radiofrequency energy to destroy extra tissue.
- Prostatic urethral lift: A procedure that moves the enlarged prostate away from the urethra.
These methods can greatly reduce symptoms with fewer side effects than surgery.
When Surgery Becomes Necessary
In some cases, surgery is needed for an enlarged prostate. The options are:
- Transurethral resection of the prostate (TURP): A common surgery that removes part of the prostate.
- Open prostatectomy: A more serious surgery, usually for bigger prostates.
Surgery is usually considered when other treatments don’t work or symptoms are very bad.
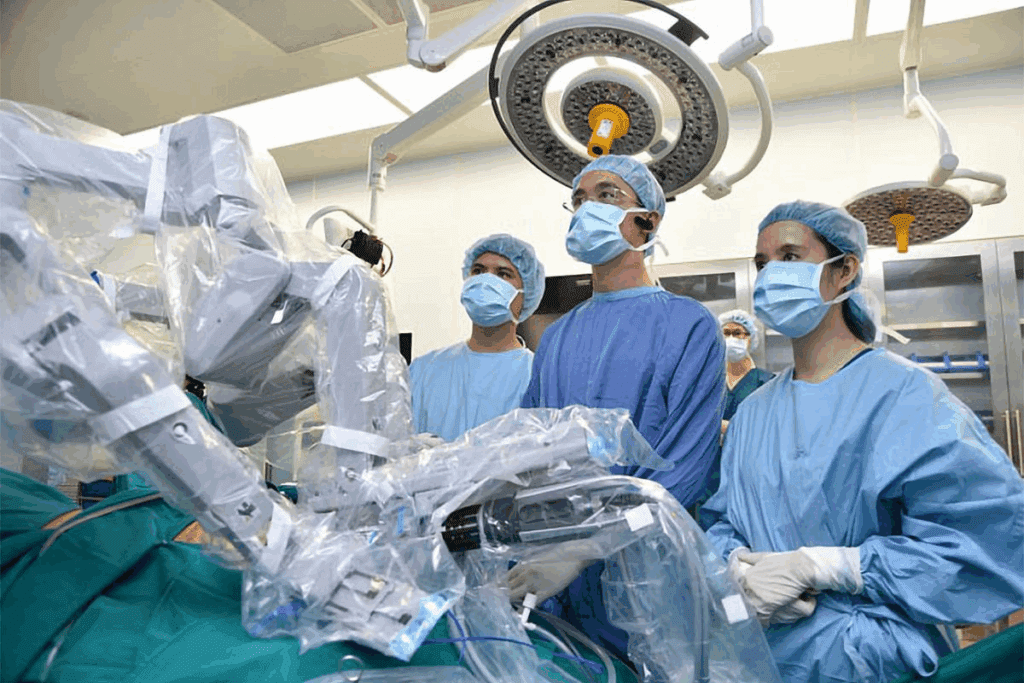
Robotic Prostatectomy: Advanced Surgical Treatment
Robotic prostatectomy is a new way to treat prostate problems. It’s a less invasive option. This method uses a robotic system to remove the prostate gland, giving many benefits over old surgery methods.
What Is Robotic Prostatectomy
Robotic prostatectomy is a modern surgery that uses a robotic system. It helps remove the prostate gland. The system has high-definition cameras and precise tools, making the surgery more accurate and less invasive.
Advantages Over Traditional Surgical Approaches
This surgery has many benefits. It leads to less blood loss, less pain after surgery, and faster recovery. The robotic system also helps keep nerves and tissues safe. This can lower the chance of problems like incontinence and erectile issues.
The Robotic-Assisted Surgical Process
In a robotic prostatectomy, the surgeon uses a console to control robotic arms. They use a 3D system to see and guide the instruments. The surgery is done through small cuts in the abdomen, allowing for precise prostate removal.
Candidates for Robotic Prostate Surgery
Not everyone can have robotic prostate surgery. The choice depends on many things like cancer stage, health, and past surgeries. Those with early prostate cancer or severe BPH might be good candidates. A urologist must check each patient to find the best treatment.
Preparing for Robotic Prostatectomy Surgery
To get the best results from robotic prostatectomy, patients need to prepare well. This includes medical checks and personal changes. It’s key for a smooth surgery and recovery.
Pre-Surgical Evaluations and Tests
Before robotic prostatectomy, patients go through many tests. These include blood tests, imaging studies like MRI or CT scans, and cardiovascular assessments. These tests check if the patient is healthy enough for surgery.
Patients also share their medical history. This includes current medications, allergies, and past surgeries. This info helps reduce surgery risks.
Lifestyle Adjustments Before Surgery
Changing your lifestyle before robotic prostatectomy can greatly help. Quitting smoking and cutting down on alcohol are key. These habits can slow healing and raise risks.
Eating a healthy diet and drinking plenty of water is also advised. A diet full of fruits, veggies, and lean proteins helps the body get ready for surgery. Losing weight if you’re overweight is also suggested, as it makes surgery easier.
Mental Preparation for Surgery and Recovery
Mental readiness is as important as physical for robotic prostatectomy. Patients should stay positive and use stress-relief methods like meditation. Knowing what to expect during recovery can also reduce anxiety.
Having a support system is helpful. This could be family, friends, or a support group. Being mentally ready can greatly improve your surgery and recovery experience.
Immediate Recovery After Robotic Prostatectomy
Recovering from robotic prostatectomy is a detailed process. It includes time in the hospital, managing pain, and care at home. Knowing what to expect can make recovery easier.
Hospital Stay Expectations
How long you stay in the hospital after robotic prostatectomy varies. Usually, it’s 1 to 2 days. Advanced robotic technology makes procedures less invasive, leading to shorter stays than traditional surgery.
In the hospital, doctors watch over you closely. They manage your pain and look for any complications. It’s important to mobilize as soon as possible to prevent blood clots and aid healing.
Managing Pain and Discomfort
Managing pain is key to recovery. You’ll be given pain medication to help with discomfort. Pain levels vary, but the right meds can help manage it.
“Effective pain management is critical for a smooth recovery. It’s vital to follow the doctor’s pain medication instructions to avoid unnecessary discomfort.”
Other methods like relaxation techniques and positioning can also help with pain.
Catheter Management After Surgery
A urinary catheter is used during surgery to drain urine. It stays in for about 1 to 2 weeks. Proper catheter care is key to prevent infections and ensure a smooth recovery.
You’ll get instructions on catheter care, including cleaning and watching for infection signs. It’s important to follow these instructions carefully to avoid complications.
First Weeks at Home: What to Expect
The first weeks at home are vital for recovery. You’re advised to take it easy and avoid hard activities, heavy lifting, and bending. As you get more comfortable, you can increase your activity level.
Following the surgeon’s instructions for follow-up care is also important. This includes when to remove the catheter and any necessary appointments. By following these guidelines, you can ensure a successful recovery.
Managing Urinary Incontinence After Prostate Surgery
Managing urinary incontinence is key after prostate surgery. Many men face this issue after a prostatectomy. It’s about losing bladder control.
Why Incontinence Occurs After Prostatectomy
Urinary incontinence happens because of muscle and nerve damage. The prostate gland is removed during surgery. This can harm the muscles and nerves around it.
Pelvic Floor Exercises for Recovery
Pelvic floor exercises, or Kegels, are vital for recovery. They strengthen muscles that support the bladder and urethra. This helps improve continence.
- Identify the correct muscles by stopping the flow of urine mid-stream.
- Perform the exercises by contracting and releasing the pelvic muscles.
- Start with short sessions and gradually increase duration and frequency.
Products and Devices for Incontinence Management
There are many products and devices for managing incontinence after prostate surgery. These include absorbent pads, adult diapers, and penile clamps.
| Product/Device | Description | Benefits |
| Absorbent Pads | Disposable pads designed to absorb urine leakage. | Convenient, discreet, and comfortable. |
| Adult Diapers | Full-coverage diapers for managing incontinence. | High absorbency, secure fit. |
| Penile Clamps | Devices that compress the urethra to prevent leakage. | Effective for stress incontinence, adjustable. |
Timeline for Continence Improvement
The time it takes to improve continence varies. Most men see big improvements in the first few months. Progress continues over the next year.
Continence Recovery Timeline:
- 1-3 months: Initial improvement as swelling reduces and muscles begin to heal.
- 3-6 months: Continued strengthening of pelvic muscles through exercises.
- 6-12 months: Most men achieve significant continence improvement.
Improving continence after prostate surgery takes time and effort. The right exercises and sometimes, specific products or devices, are key. Understanding the causes and using the right strategies can greatly improve a man’s quality of life after surgery.
Sexual Function and Intimacy After Prostate Removal
Removing the prostate gland can change how men feel about sex and closeness. It’s important to understand these changes and how to deal with them.
Changes in Ejaculation and Orgasm
Men often notice changes in how they ejaculate and orgasm after prostate removal. The prostate helps with ejaculation, so its removal can lead to dry orgasms. This might feel different, but it’s usually not a problem.
Some important things to remember:
- Dry orgasms are common after prostate removal.
- The feeling of orgasm might stay the same for some men.
- Others might notice a difference in how intense or felt their orgasm is.
Erectile Dysfunction Following Surgery
Erectile dysfunction (ED) can also happen after prostate removal surgery. The nerves around the prostate are important for getting an erection. Damage to these nerves can cause ED.
Things that can affect the chance of getting ED include:
- How much nerve damage there is during surgery.
- The patient’s age and health.
- How well they were able to get an erection before surgery.
Medical Interventions for Sexual Function
There are many ways to help with erectile dysfunction and other sexual issues after prostate removal. These include:
- Oral medications like PDE5 inhibitors.
- Penile injections and vacuum devices.
- Penile implants for more serious cases.
Talking to a healthcare provider is key to finding the right treatment.
Maintaining Intimacy During Recovery
Keeping intimacy alive after prostate removal surgery is important for emotional and relationship health. Intimacy is more than just sex.
Ways to keep intimacy alive include:
- Talking openly with your partner.
- Trying non-sexual ways to be close, like cuddling or doing things together.
- Getting help from counselors or therapists if needed.
By focusing on these areas, men can face the challenges of prostate removal with a better outlook on sex and closeness.
Long-Term Recovery and Returning to Normal Activities
Knowing how to recover after a prostatectomy is key. It helps manage expectations and makes the transition back to normal life smoother.
Physical Activity Guidelines After Surgery
Physical activity is vital for recovery. At first, avoid heavy lifting and bending. Start with gentle activities to build strength and health.
- Begin with short walks and increase the distance gradually.
- Avoid high-impact activities for at least 6 weeks after surgery.
- Doing pelvic floor exercises, like Kegels, helps with bladder control.
Driving and Travel Considerations
Plan your driving and travel carefully during recovery. Usually, you can drive when you’re off pain meds and can sit and drive comfortably.
- Always check with your doctor before traveling, even for short trips.
- Make sure medical care is available at your destination.
- Travel with someone if you can, for help if needed.
Returning to Work After Prostatectomy
When you can go back to work depends on your job and how fast you recover. Jobs that don’t require much physical effort might be easier to return to.
Talk to your doctor about when you can go back to work. Consider:
- The physical demands of your job.
- If you need any job changes or help.
- If you’ll need more time to recover.
Exercise Recommendations for Optimal Recovery
Exercise is important for recovery, improving both physical and mental health. A good mix of exercises can help you regain strength and improve bladder control.
Good exercises include:
- Pelvic floor exercises (Kegels).
- Low-impact activities like walking or swimming.
- Stretching to improve flexibility.
By following these tips and talking to your doctor, you can recover well and quickly.
Nutrition and Lifestyle for Prostate Health Recovery
After prostate surgery, the right diet and lifestyle are key for recovery. A balanced diet helps the healing process and supports prostate health.
Foods That Support Healing After Surgery
Some foods are great for recovery after prostate surgery. These include:
- Leafy Greens: Rich in antioxidants, spinach and kale boost overall health.
- Berries: Berries are full of antioxidants and may lower inflammation.
- Fatty Fish: Fatty fish like salmon have omega-3s, which fight inflammation.
- Nuts and Seeds: Almonds and sunflower seeds offer healthy fats and antioxidants.
Foods to Avoid During Recovery
Some foods can slow down recovery. It’s best to limit or avoid:
- Processed Meats: Foods like sausages and bacon have unhealthy fats and sodium.
- Sugary Drinks: Too much sugar can cause inflammation.
- High-Sodium Foods: Too much sodium can cause water retention and discomfort.
Hydration and Its Importance
Drinking enough water is vital for recovery. It helps in:
- Flushing Out Toxins: Water removes toxins from the body.
- Supporting Healing: Hydration is key for the body’s healing.
Supplements for Prostate Health
While a balanced diet is important, some supplements can also help. These include:
| Supplement | Potential Benefits |
| Saw Palmetto | May reduce urinary symptoms from an enlarged prostate. |
| Zinc | Important for prostate health and immune function. |
| Omega-3 Fatty Acids | Can reduce inflammation. |
Always talk to a healthcare provider before taking any supplements.
Psychological Aspects of Prostate Surgery Recovery
Recovering from prostate surgery is more than just healing physically. It also involves dealing with the emotional side. This can affect how a person sees their body and their sexual health.
Coping with Body Image Changes
Prostate surgery can change how a person views their body. It involves removing or changing a gland linked to masculinity and sex. Patients might feel lost or unsure about themselves. It’s important to recognize these feelings and find support. Support can come from loved ones, friends, or groups for those going through similar experiences.
Managing Anxiety About Sexual Function
Sexual function changes are a big worry after prostate surgery. Worrying about not being able to have an erection or changes in ejaculation can be tough. Talking openly with doctors can help. They can suggest treatments and therapies to help with these issues.
Support Groups and Resources
Support groups, both in-person and online, offer a place for patients to share and get support. They are a great resource for dealing with the emotional side of recovery.
| Resource Type | Description | Benefits |
| Support Groups | Groups where patients share their experiences | Emotional support, shared understanding |
| Counseling Services | Professional counseling for emotional challenges | Guidance, coping strategies |
| Online Forums | Online platforms for discussion and support | Accessibility, anonymity |
When to Seek Professional Mental Health Support
If feelings of anxiety, depression, or distress last or really affect daily life, getting help from a mental health professional is key. They can offer strategies and therapies to help manage these issues. This can improve overall well-being during recovery.
By understanding the emotional side of prostate surgery recovery and getting the right support, patients can get through this tough time better. This can lead to a better quality of life.
Follow-up Care and Long-term Monitoring
After prostate surgery, it’s important to keep an eye on your health. Getting the right care is key for your long-term health and happiness.
Post-Surgery Appointment Schedule
After surgery, you’ll see your urologist often. These visits help check how you’re healing and if everything is okay. You might see your doctor more often in the first few months.
PSA Testing After Prostatectomy
The Prostate-Specific Antigen (PSA) test is a big deal after surgery. It checks for prostate health by looking at PSA levels in your blood. If your prostate is gone, your PSA should be very low or not there at all. Watching your PSA levels helps find cancer early if it comes back.
Warning Signs That Require Medical Attention
Know the signs that mean you need to see a doctor right away. Look out for severe pain, trouble peeing, signs of infection, or any symptoms that worry you. Catching these signs early can help fix problems fast.
- Severe or worsening pain not controlled with medication
- Difficulty starting or stopping urination
- Signs of infection such as fever, chills, or redness around the surgical site
- Blood in the urine or semen
Questions to Ask Your Urologist
Don’t be shy to ask your doctor questions during your visits. Ask about PSA levels, how often you should see them, and what signs of trouble to watch for.
Being active in your care helps you recover well and stay healthy for a long time.
Conclusion: Balancing Prostate Health and Quality of Life
After prostatectomy, it’s key to balance prostate health and quality of life. Knowing about possible complications helps manage them. This way, people can keep a good quality of life.
Prostate health is tied to overall well-being. Managing it well is important for a smooth recovery. By handling urinary incontinence and sexual function well, people can live better.
Regular check-ups are important to catch any problems early. This ensures any issues are quickly fixed.
By focusing on prostate health, people can have a better life after surgery. Making smart treatment choices and living healthy are important. Getting support when needed is also vital.
Managing prostate health well is essential for a good balance between health and quality of life.
FAQ
What is robotic prostatectomy?
Robotic prostatectomy is a surgery that uses a robotic system. It removes the prostate gland. It’s used to treat prostate cancer and other prostate issues.
How does ejaculation affect prostate health?
Ejaculation might help keep the prostate healthy by removing bacteria. But, more research is needed to confirm this.
What are the symptoms of an enlarged prostate?
Signs of an enlarged prostate include trouble starting or stopping urination. You might also have weak or interrupted urine flow, frequent urination, and waking up to urinate at night.
What are the conventional treatments for enlarged prostate?
Treatments for an enlarged prostate include medication, minimally invasive procedures, and surgery. The right treatment depends on your symptoms and health.
How long does it take to recover from robotic prostatectomy?
Recovery time from robotic prostatectomy varies. Most men can get back to normal in a few weeks.
What can I expect during the immediate recovery period after robotic prostatectomy?
Right after surgery, you might feel pain, discomfort, and have trouble controlling your urine. You’ll also have a catheter to drain your bladder.
How can I manage urinary incontinence after prostate surgery?
To manage incontinence, try pelvic floor exercises like Kegels. You can also use incontinence products like pads or adult diapers.
Will I be able to have sex after prostate removal?
Yes, you can have sex after prostate removal. But, you might notice changes in ejaculation and orgasm. Erectile dysfunction is also common.
What are the benefits of robotic prostatectomy?
Robotic prostatectomy has less blood loss, pain, and a shorter hospital stay. It also leads to faster recovery than traditional surgery.
How soon can I drive a car after prostate surgery?
Don’t drive for a few days after surgery. Wait until you’re off narcotic pain meds and feel safe driving.
What foods should I avoid after prostate surgery?
Avoid spicy or acidic foods after surgery. Drink plenty of water to stay hydrated.
When should I seek professional mental health support after prostate surgery?
Seek mental health support if you’re feeling anxious, depressed, or emotionally distressed after surgery.
What is the success rate of robotic prostatectomy?
Success rates vary by case and surgeon. But, robotic prostatectomy is often very effective for prostate cancer.
How often should I follow up with my urologist after prostate surgery?
Follow up with your urologist as recommended. This is usually at regular intervals to check your recovery and for any complications.
Reference
- Rider, J. R., Wilson, K. M., Sinnott, J. A., Kelly, R. S., Mucci, L. A., & Giovannucci, E. L. (2016). Ejaculation frequency and risk of prostate cancer: Updated results with an additional decade of follow-up. European Urology, 70(6), 974-982. https://pubmed.ncbi.nlm.nih.gov/27033442/
- Kokori, E., & Heretis, G. (2024). Ejaculation frequency and prostate cancer risk: A narrative review. Current Urology Reports. https://www.sciencedirect.com/science/article/abs/pii/S1558767324000168