Last Updated on December 2, 2025 by Bilal Hasdemir

Varicose veins affect millions of Americans, causing discomfort and potentially leading to more serious health issues. For those suffering from this condition, understanding the available treatment options and their coverage under Medicare is key.
Laser ablation is a minimally invasive procedure used to treat varicose veins. Medicare coverage for this treatment is available under specific conditions, making it an important option for those eligible.
Understanding the criteria for coverage can help individuals navigate the process and access necessary care. This article will explore the conditions under which Medicare covers laser ablation for varicose vein treatment.
Get the definitive answer: does medicare cover varicose vein treatment? Understand the coverage rules clearly.
Key Takeaways
- Medicare covers varicose vein treatments deemed medically necessary.
- Laser ablation is a covered treatment under specific conditions.
- Understanding Medicare coverage criteria is essential for accessing care.
- Eligibility for coverage depends on the severity of varicose veins.
- Documentation of medical necessity is required for coverage.
Understanding Varicose Veins and Laser Ablation

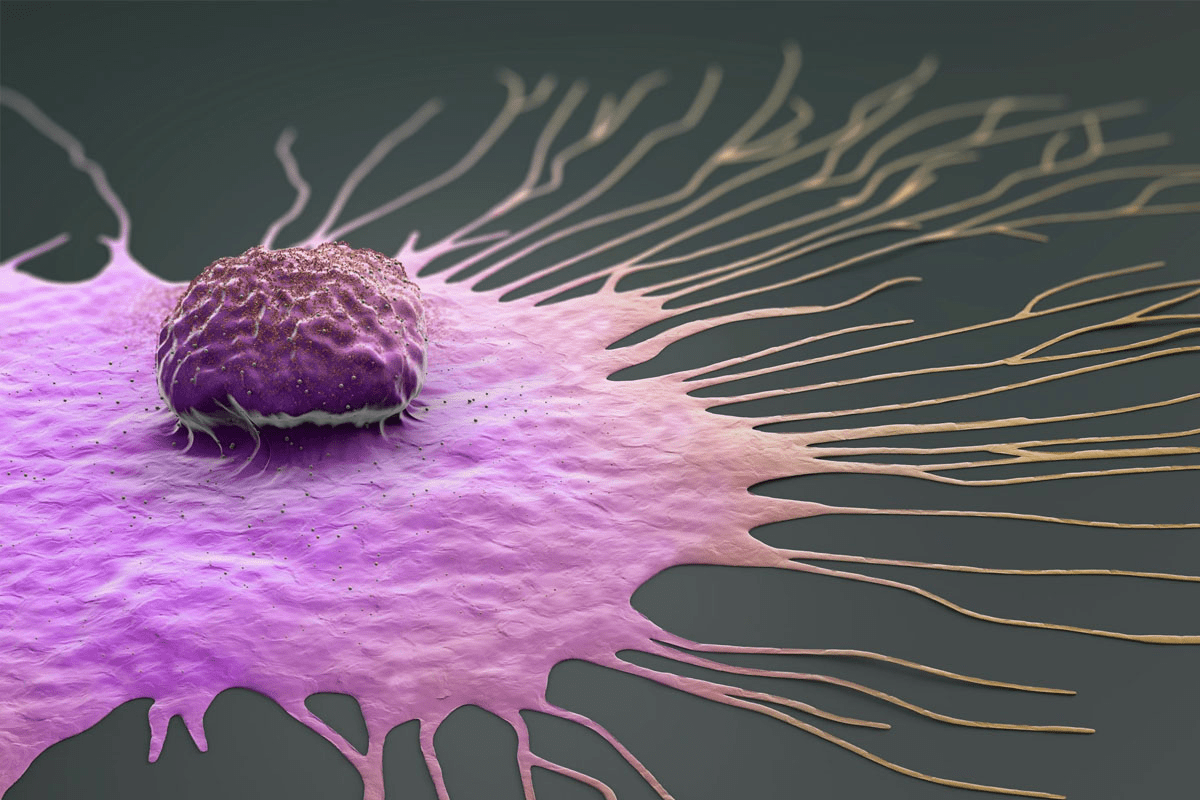
It’s important to know what causes varicose veins and their complications. This knowledge helps find the best treatment, like laser ablation. Varicose veins are enlarged and twisted veins, often causing pain and serious health problems if not treated.
What Are Varicose Veins and Their Causes
Varicose veins look twisted and enlarged, mainly in the legs. They happen when vein valves get weak or damaged. This leads to blood pooling and vein growth. Genetics, age, obesity, and standing for long periods can cause them.
Medical Complications of Untreated Varicose Veins
Untreated varicose veins can cause serious health issues. These include:
- Leg heaviness and swelling
- Restless leg syndrome
- Skin ulcers
- Pain and discomfort
These problems can really affect your life, making it important to get medical help.
How Laser Ablation Works as a Treatment Option
Laser ablation is a treatment for varicose veins. It works by closing off the bad vein. Here’s how it’s done:
- A laser fiber is put into the vein.
- The laser heats the vein, making it close.
- Blood then flows to healthier veins.
This procedure is done under local anesthesia and works well to ease symptoms and improve vein health.
| Benefits of Laser Ablation | Characteristics |
| Minimally invasive | Performed under local anesthesia |
| High success rate | Effective in alleviating symptoms |
| Quick recovery | Patients can resume normal activities shortly after |
Medicare Basics: Coverage Categories and Plans
To understand Medicare coverage for varicose vein treatments, knowing its parts is key.
Medicare has several parts, each covering different healthcare aspects. Knowing what each part covers is vital for varicose vein treatment coverage.
Medicare Part A, B, C, and D
Many patients wonder if Medicare will cover varicose vein treatment. Medicare’s rules can be tricky. It’s important to know the details to get relief from varicose vein symptoms.
General Coverage Guidelines for Vein Treatments
Medicare covers treatments that are medically necessary. For varicose veins, the treatment must fix a medical problem, not just for looks. Medical necessity is key to coverage.
Medicare looks at how bad the symptoms are and how they affect your life. If a treatment is needed, it’s more likely to be covered.
Medical Necessity Requirements
Varicose vein treatments need proof they’re medically necessary. This means showing pain, swelling, or other problems from the veins.
Documentation is essential to prove this. Patients should talk to their doctors to make sure all needed info is given to Medicare.
Conservative Treatment Requirements Before Approval
Before Medicare says yes to big treatments like laser ablation, you must try simpler ones first. This includes wearing compression stockings and making lifestyle changes.
This rule makes sure simpler ways are tried first. Conservative treatment failure is often needed for Medicare to cover varicose vein treatments.
Knowing these rules and talking to your doctor can help you get Medicare to cover varicose vein treatments.
Laser Ablation Coverage Under Medicare
Knowing about Medicare coverage for laser ablation helps patients choose the right treatment for varicose veins. Medicare covers many medical procedures, including laser ablation, under certain rules.
Specific Coverage Criteria for Laser Ablation
For Medicare to cover laser ablation, certain rules must be followed. These include proof of varicose vein condition, symptoms like pain or swelling, and trying conservative treatments first. Conservative treatments usually include wearing compression stockings and making lifestyle changes.
Medicare also needs to see that the treatment is medically necessary. This means the procedure is key for diagnosing or treating a medical issue. A healthcare provider decides if it’s necessary.
Documentation Required for Medicare Approval
To get Medicare approval for laser ablation, detailed records are needed. These include:
- Medical records showing the diagnosis and how bad the varicose veins are
- Proof of symptoms and how they affect daily life
- Records of trying conservative treatments, like wearing compression stockings and making lifestyle changes
- A letter from the doctor saying the treatment is needed
CPT Codes Related to Laser Ablation
Laser ablation procedures use specific CPT codes for billing and coverage. Common codes for this treatment are 36478 and 36479 for endovenous laser treatment. It’s important to check the latest CPT codes with Medicare or a healthcare provider.
Understanding the rules, needed documents, and CPT codes helps patients get Medicare coverage for laser ablation treatment for varicose veins.
Medicare Coverage for Other Varicose Vein Treatments
Medicare covers more than just laser ablation for varicose veins. It offers several treatments to meet different needs. These options are vital for those dealing with varicose veins and related issues.
Sclerotherapy Coverage and Limitations
Sclerotherapy involves injecting a solution to close off veins. Medicare covers sclerotherapy when it’s needed, after other treatments fail. But, there are limits on how many times it’s covered in a short time.
Radiofrequency Ablation Coverage
Radiofrequency ablation treats varicose veins like laser ablation but with radiofrequency energy. Medicare covers it when it’s medically necessary, after trying other treatments first.
Vein Stripping and Phlebectomy Coverage
Vein stripping and phlebectomy are surgeries to remove varicose veins. Medicare pays for these if they’re medically necessary. Coverage depends on how severe symptoms are and if other treatments failed.
It is essential for patients to understand Medicare’s rules regarding these treatments. They must meet certain medical criteria and show they’ve tried other treatments first. Patients should talk to their doctor to find the best treatment. They should also understand what Medicare covers and any costs they might face.
Does Medicare Cover Spider Vein Treatment?
To find out if Medicare covers spider vein treatment, we need to understand the difference between spider veins and varicose veins.
Differences Between Spider Veins and Varicose Veins
Spider veins and varicose veins are both vascular issues, but they look and feel different. Spider veins are small and appear as red or purple lines on the skin. On the other hand, varicose veins are bigger and can hurt. Knowing these differences helps figure out if Medicare will cover treatment.
Coverage Limitations for Cosmetic Procedures
Medicare usually doesn’t pay for cosmetic treatments. This includes most spider vein treatments, which are seen as cosmetic. But, there are times when Medicare might cover it if it’s medically necessary.
When Spider Vein Treatment May Be Covered
If spider veins are linked to venous insufficiency or other health issues, Medicare might pay for treatment. It’s important for patients to get a detailed medical check-up. This check-up helps see if Medicare will cover the treatment.
Patients should talk to their doctor to understand what’s needed for Medicare coverage. This way, they can make smart choices about their treatment and deal with Medicare’s rules on vein treatments.
Medicare Advantage Plans and Varicose Vein Coverage
Medicare Advantage plans offer different coverage options for varicose vein treatments. These plans are provided by private insurance companies approved by Medicare. They may offer extra benefits that are important for those seeking varicose vein treatment.
Differences in Coverage
Medicare Advantage plans cover varicose vein treatments differently than Original Medicare. While Original Medicare covers some treatments, Advantage plans might offer more. They might include dental, vision, and hearing coverage, but the details vary by plan.
Key differences in coverage may include:
- Different copays or coinsurance rates for varicose vein treatments
- Variations in coverage for specific treatments, such as sclerotherapy or laser ablation
- Requirements for prior authorization or referrals from primary care physicians
Comparing Plans for Vein Treatment Benefits
When comparing Medicare Advantage plans for varicose vein treatment benefits, it’s important to review the plan’s formulary and coverage rules. Look for plans that cover your prescribed treatments and consider the costs.
Factors to consider when comparing plans include:
- The network of providers and specialists available under the plan
- The plan’s coverage for specific varicose vein treatments
- Any additional benefits that may be relevant to overall health
Network Restrictions and Provider Considerations
Medicare Advantage plans often have network restrictions. Beneficiaries must see providers within the plan’s network for coverage. It’s important to ensure your vein specialist is in the network to avoid extra costs or denied claims.
Before enrolling, check if your preferred vein specialists are in the plan’s network. This helps ensure you get the care you need without unexpected expenses.
Out-of-Pocket Costs for Laser Ablation with Medicare
When you think about laser ablation for varicose veins, knowing the costs is key. Medicare helps a lot, but you’ll have some costs too. It’s good to know what you’ll pay.
Deductibles and Coinsurance
Medicare Part B covers laser ablation for varicose veins if it’s needed. After that, Medicare pays 80% of the cost, and you pay 20%.
Supplemental Insurance Considerations
Many people have supplemental insurance, or Medigap. It can help with Medicare costs like coinsurance and deductibles. The help varies by Medigap plan.
Check your Medigap policy to see what it covers. Some plans might cover the coinsurance for laser ablation. This can lower what you pay a lot.
Typical Cost Ranges for Patients
The cost of laser ablation under Medicare can change. It depends on the Medicare-approved amount, your insurance, and other medical costs.
| Expense Category | Cost | Patient Responsibility |
| Medicare Part B Deductible | $233 (2024) | $233 |
| Coinsurance for Laser Ablation | 20% of Medicare-approved amount | $400 (example based on $2,000 approved amount) |
| Medigap Coverage | Varies by plan | Potentially $0 if fully covered |
It’s important to know these costs if you’re thinking about laser ablation for varicose veins. Look at your Medicare, insurance, and talk to your doctor. This way, you can get ready for the costs of treatment.
Medicare Coverage Process for Vein Treatments
It’s important for patients to know how Medicare covers varicose vein treatments. The process has several steps. Patients need to follow these steps to get the coverage they need.
Prior Authorization Requirements
Getting prior authorization is the first step for Medicare coverage. Prior authorization means Medicare needs to approve a treatment before it’s done. For varicose veins, this means showing why the treatment is needed.
” “Patients should work with their doctors to make sure all needed documents are in.”
Appeals Process for Denied Claims
If Medicare denies a claim for varicose vein treatment, patients can appeal. The appeals process has several levels. It starts with a redetermination request to the Medicare Administrative Contractor (MAC).
Patients should work with their doctors to understand why the claim was denied. They also need to gather more information to support their appeal.
- Level 1: Redetermination by the MAC
- Level 2: Reconsideration by a Qualified Independent Contractor (QIC)
- Level 3: Hearing with an Administrative Law Judge (ALJ)
Working with Your Doctor to Secure Coverage
Working together with healthcare providers is key to getting Medicare coverage. Providers can help with the prior authorization and appeals. They make sure all needed documents are in.
Good communication between patients and doctors is important. Patients should talk about their symptoms, treatment options, and any concerns about Medicare coverage.
By understanding the Medicare coverage process and working with healthcare providers, patients can get the coverage they need for varicose vein treatments.
Vein Clinics That Accept Medicare
Many vein clinics across the country accept Medicare. This means patients with varicose veins have access to various treatments. These clinics provide specialized care to ensure the right treatment for each patient.
They use treatments like laser ablation and sclerotherapy. Their team works with patients to find the best treatment.
Services Offered: Laser Ablation, Sclerotherapy, Vein Stripping
Southlake Vein Care Services and Medicare Acceptance
They offer full care, from the first visit to aftercare. They use radiofrequency ablation and other treatments.
Services Offered: Radiofrequency Ablation, Sclerotherapy, Compression Therapy
Center for Vein Restoration in Leesburg
They tailor treatments like laser ablation and sclerotherapy to each patient’s needs.
Services Offered: Laser Ablation, Sclerotherapy, Ambulatory Phlebectomy
| Clinic Name | Location | Services | Medicare Accepted |
| Legacy Vein Clinic | Mishawaka | Laser Ablation, Sclerotherapy, Vein Stripping | Yes |
| Southlake Vein Care | Southlake | Radiofrequency Ablation, Sclerotherapy, Compression Therapy | Yes |
| Center for Vein Restoration | Leesburg | Laser Ablation, Sclerotherapy, Ambulatory Phlebectomy | Yes |
Restless Leg Syndrome and Vein Disease Connection
For many, Restless Leg Syndrome (RLS) is more than a bother; it’s a sign of vein disease. Studies show a strong link between RLS and venous insufficiency, often linked to varicose veins.
RLS and Venous Insufficiency Relationship
RLS’s cause is complex, but venous insufficiency is a big part of it. When leg veins can’t move blood back to the heart, pressure and oxygen-depleted blood build up. This can cause the uncomfortable feelings of RLS.
Key factors linking RLS to venous insufficiency include:
- Poor circulation and venous hypertension
- Increased inflammation and oxidative stress
- Potential genetic predispositions
Medicare Coverage for RLS Related to Vein Issues
Medicare’s coverage for RLS treatments due to vein disease is complex. Medicare Part B covers necessary procedures, like tests and treatments for varicose veins and venous insufficiency.
If RLS is linked to vein disease, treatments for the vein issue might be covered. This could include laser ablation or sclerotherapy for varicose veins.
It’s vital for patients to work with their doctors to prove these treatments are needed. This might mean trying conservative treatments first before getting approval for more invasive ones.
emphasizes, “Getting a correct diagnosis and proof is key to getting Medicare to cover RLS treatments related to vein disease.”
State-by-State Variations in Medicare Coverage for Vein Treatments
State-by-state differences are key in figuring out Medicare coverage for vein treatments. Medicare is a federal program, but how it works can change a lot from state to state.
Local Coverage Determinations (LCDs)
Local Coverage Determinations (LCDs) are a big reason for these differences. LCDs are made by Medicare Administrative Contractors (MACs) about what medical procedures are covered. This includes treatments for varicose veins.
For example, an LCD might say what makes a treatment necessary, what documents are needed, or what treatments are okay. So, what’s covered in one state might not be in another. Or, the rules for coverage could be different.
Regional Medicare Administrative Contractors
Regional Medicare Administrative Contractors (MACs) handle Medicare claims in their areas. They make sure LCDs are followed and Medicare rules are applied right.
The choices MACs make about LCDs can cause differences in coverage for vein treatments. It’s important for patients and doctors to know the specific rules in their area.
How to Research Coverage in Your State
To deal with these differences, you can take a few steps to find out about Medicare coverage for vein treatments in your area:
- Check the Medicare website for info on LCDs and MACs in your state.
- Call your local Medicare Administrative Contractor to ask about coverage policies.
- Talk to your doctor, who can help understand the rules and what’s needed for vein treatments in your state.
Knowing the state-specific things that affect Medicare coverage helps patients get the treatments they need for varicose veins.
Alternative Insurance Options for Varicose Vein Treatment
There are other insurance options for varicose vein treatment beyond Medicare. Medicare is a main insurance for many, but knowing about other insurance types is key for full care.
Medicaid Coverage for Vein Treatments
Medicaid is a program funded by the state and federal government. It covers health care for low-income adults, children, pregnant women, the elderly, and people with disabilities. Medicaid coverage for varicose vein treatments varies by state, as each state has its own rules.
Some states may cover treatments like laser ablation for varicose veins under Medicaid. This is if the treatment is seen as medically necessary. But, the amount of coverage and what treatments are covered can change a lot.
Private Insurance Comparison
Private insurance plans are offered by employers or can be bought individually. The specifics of coverage depend on the insurance provider and the details of the plan. Some plans might cover more treatments, like sclerotherapy and vein stripping, along with laser ablation.
When looking at private insurance plans, it’s important to check the policy details. Look at deductibles, copays, and any out-of-pocket maximums. Also, make sure to understand the network of providers and any pre-approval needs.
For those looking into varicose vein treatment, checking out these alternative insurance options can help lower costs. Whether it’s through Medicaid or private insurance, the right coverage can greatly affect the cost and accessibility of treatments.
Future Trends in Medicare Coverage for Vein Treatments
The future of Medicare coverage for vein treatments is linked to new technologies and policy changes. As medical science advances, it’s key to know how these changes might affect coverage for varicose vein treatments.
Emerging Technologies and Coverage Implications
New technologies are changing how we treat varicose veins. Some of these include:
- Advanced laser systems that are more precise and less invasive.
- Enhanced sclerotherapy techniques with new formulas and ways of delivery.
- Minimally invasive procedures that cut down recovery time and boost results.
As these technologies grow, Medicare might update its coverage to include them. But, adding new technologies to Medicare coverage is a detailed process. It involves careful evaluation.
Potential Policy Changes
Medicare policies can change due to new evidence, law updates, and feedback from stakeholders. Possible changes that could affect varicose vein treatment coverage include:
- Updates to what makes a treatment medically necessary.
- Changes to the list of covered procedures and technologies.
- Modifications to the prior authorization process.
It’s important for healthcare providers and patients to keep up with these possible changes.
Advocacy for Expanded Coverage
Advocacy is key in shaping Medicare coverage policies. Groups like patient advocacy, healthcare providers, and device makers can sway coverage by sharing evidence and success stories.
Key areas for advocacy include:
- Spreading the word about the latest treatment options.
- Sharing data on how effective and cost-effective new technologies are.
- Talking to policymakers to push for more coverage.
By teaming up, everyone can help Medicare coverage for varicose vein treatments keep getting better.
Conclusion: Navigating Medicare Coverage for Laser Ablation
Understanding Medicare coverage for laser ablation is key. It’s important to know what’s needed for varicose vein treatment. Medicare will cover laser ablation if it’s medically necessary.
To get coverage, patients must meet certain criteria. They need to have tried conservative treatments first. They also need to document their condition well.
Working with healthcare providers is vital. They can help gather all the needed documents. This makes it easier to get Medicare to cover varicose vein treatments, like laser ablation.
If you’re thinking about varicose vein treatment, learn about Medicare coverage. Knowing the costs and what’s required helps make better choices. This way, patients can get the care they need.
FAQ
Does Medicare cover laser ablation for varicose veins?
Medicare covers laser ablation for varicose veins if it’s medically necessary. It must meet specific criteria, including trying conservative treatments first.
What are the requirements for Medicare to cover varicose vein treatment?
Medicare needs varicose vein treatments to be medically necessary. Patients must try conservative treatments before getting approved for more invasive ones.
Is sclerotherapy covered by Medicare for varicose veins?
Sclerotherapy might be covered by Medicare for varicose veins if it’s needed. Coverage depends on the situation and the Medicare plan.
Does Medicare cover spider vein treatment?
Medicare usually doesn’t cover spider vein treatment because it’s seen as cosmetic. But, if spider veins are linked to venous insufficiency, treatment might be covered.
How do Medicare Advantage plans cover varicose vein treatments?
Medicare Advantage plans might cover varicose vein treatments, like laser ablation. But, coverage varies a lot between plans. It’s key to check the plan’s benefits and network.
What are the out-of-pocket costs for laser ablation under Medicare?
Costs for laser ablation under Medicare include deductibles and coinsurance. Supplemental insurance can help lower these costs.
Can I appeal a denied claim for varicose vein treatment under Medicare?
Yes, you can appeal a denied claim for varicose vein treatment. Working closely with your healthcare provider is important in the appeals process.
Is restless leg syndrome related to venous insufficiency covered by Medicare?
If restless leg syndrome is caused by venous insufficiency, Medicare might cover treatments. This depends on medical necessity and coverage criteria.
How can I find out the specific Medicare coverage for varicose vein treatments in my state?
Medicare coverage for varicose vein treatments varies by state. You can find out your state’s coverage by contacting Medicare or visiting their website.
Are there alternative insurance options for varicose vein treatments?
Yes, you can look into Medicaid and private insurance for varicose vein treatments. Coverage and benefits differ, so it’s important to review each option.
Will emerging technologies affect Medicare coverage for varicose vein treatments?
New technologies might change Medicare’s coverage for varicose vein treatments. It’s important to stay updated on the latest developments and policy changes.
Does caffeine affect restless leg syndrome associated with venous insufficiency?
Caffeine can make restless leg syndrome (RLS) symptoms worse. If RLS is caused by venous insufficiency, treating both the RLS and vein issues is key.
Can ibuprofen help with restless leg syndrome?
Ibuprofen might help with some RLS symptoms. But, it doesn’t treat the underlying cause. Treating the vein issues is necessary if RLS is related to venous insufficiency.
Does Tylenol help with restless legs?
Tylenol (acetaminophen) might ease some RLS discomfort. But, it doesn’t fix the root cause. Treating the vein condition is essential if RLS is caused by venous insufficiency.
Is there a connection between weed use and restless leg syndrome?
Some studies suggest cannabis (weed) might affect RLS, possibly helping or worsening symptoms. More research is needed to fully understand its impact.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra2017365