Last Updated on November 20, 2025 by Ugurkan Demir

Sickle Cell Disease (SCD) is a group of inherited blood disorders. They affect the hemoglobin molecule in red blood cells. This makes them take on a sickle-like shape.Understand drépanocytose in English—its causes, symptoms, and genetics explained with simple diagrams.
This genetic mutation causes health problems. These include pain crises, anemia, and a higher risk of infections.
At Liv Hospital, we know sickle cell disease is a complex condition. It needs thorough care and support. Our team is dedicated to giving top-notch, patient-focused care to those with this condition.

A single point mutation in the HBB gene causes sickle cell disease. This mutation leads to abnormal hemoglobin, known as hemoglobin S (HbS). It results in red blood cells that are abnormally shaped.
The HBB gene tells our bodies how to make beta-globin, a key part of hemoglobin. A point mutation in this gene changes glutamic acid to valine at the sixth position of beta-globin. This small change greatly affects hemoglobin’s structure and function.
The mutation leads to the creation of HbS, an abnormal hemoglobin. Under certain conditions, HbS forms long, rigid fibers. This causes red blood cells to become sickle-shaped.
The sickling process is complex. It involves many molecular interactions. When red blood cells with HbS face low oxygen levels, they polymerize. This makes them rigid and sickle-shaped.
| Condition | Hemoglobin Type | Red Blood Cell Shape |
| Normal | HbA | Round |
| Sickle Cell Disease | HbS | Sickle-shaped |
Understanding these molecular mechanisms is key. It helps in developing therapies to reduce sickling crises in sickle cell disease patients.
Learning how sickle cells form is key to understanding the disease. It involves changes at the molecular level that cause red blood cells to sickle.
Hemoglobin is a protein in red blood cells that carries oxygen. In sickle cell disease, a genetic change leads to abnormal hemoglobin, called hemoglobin S (HbS). Unlike normal hemoglobin, HbS has a different amino acid that causes it to stick together when oxygen levels are low.
A medical expert says, “The change from glutamic acid to valine at position 6 of the beta-globin chain causes sickle cell disease.”
This mutation makes HbS prone to forming long strands when it’s not carrying oxygen.
When oxygen levels are low, HbS forms long strands in red blood cells. This process starts off reversible but becomes permanent as the strands grow and damage the cell membrane.
The formation of HbS strands is a key part of sickle cell disease. These strands distort the red blood cell, making it sickle-shaped.
| Hemoglobin Type | Structure | Behavior Under Low Oxygen |
| Normal Hemoglobin (HbA) | Normal beta-globin chains | Remains soluble |
| Sickle Hemoglobin (HbS) | Mutated beta-globin chains | Polymerizes |
The sickling of red blood cells causes several changes. These include increased rigidity, reduced ability to change shape, and sticking to blood vessel walls. These changes lead to vaso-occlusive crises, hemolytic anemia, and other complications.
Understanding sickle cell disease shows it’s more than a simple genetic disorder. It involves complex molecular and cellular processes.
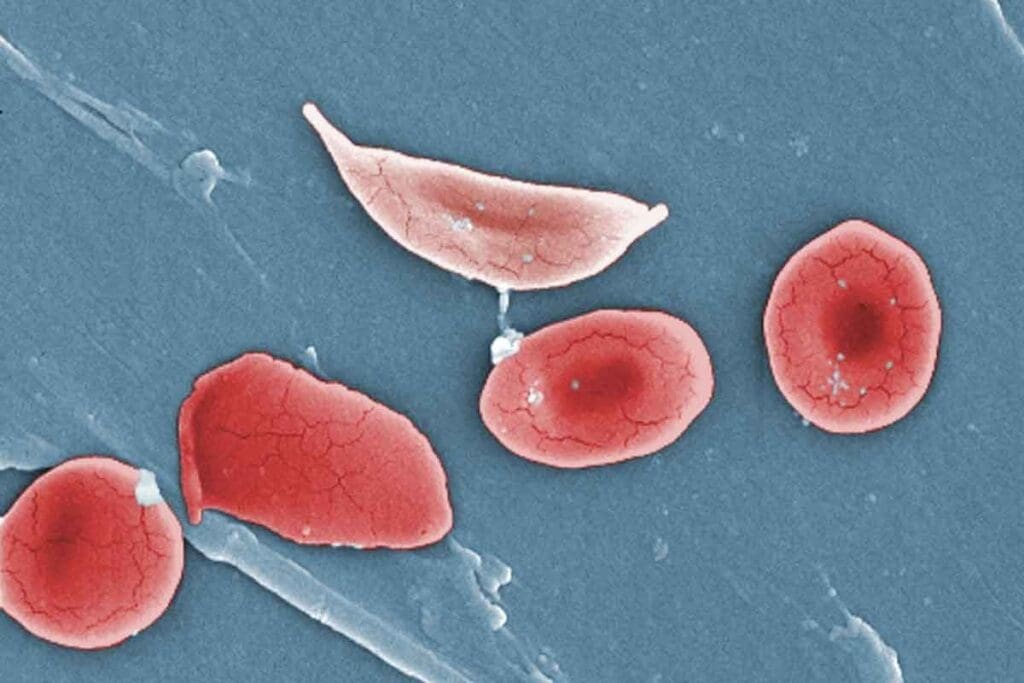
Understanding Sickle Cell Disease goes beyond knowing its genetic roots. It also requires seeing how it affects cells. Pictures help us understand the differences between normal and sickled red blood cells.
Diagrams show the clear difference between normal and sickled red blood cells. Normal cells are flexible and disk-shaped, moving easily through blood vessels. Sickled cells, on the other hand, are stiff and crescent-shaped, causing blockages.
The change from normal to sickled red blood cells is complex. It involves the clumping of abnormal hemoglobin. Diagrams make this process clear, showing how HbS molecules come together under low oxygen, causing cells to sickle.
Visual aids also show how sickled cells block blood flow. Figure (A) shows normal cells moving freely. Figure (B) shows sickled cells causing a blockage at a blood vessel branch. These diagrams are key to understanding Sickle Cell Disease.
It’s important to know who gets sickle cell disease to help them better. This disease is a big problem in many places, mainly in warm and tropical areas.
Most people with sickle cell disease are from Africa, the Middle East, and South Asia. This is because the disease helps protect against malaria, a serious illness.
In Sub-Saharan Africa, about 80% of sickle cell disease cases happen. This is because the disease is very common in areas where malaria is also common. Millions of people worldwide have the sickle cell trait.
The sickle cell trait helps protect against malaria, a deadly disease. This is why it’s more common in places where malaria is a big problem.
“The sickle cell trait provides a selective advantage against malaria, which has led to its increased frequency in populations from areas with high malaria transmission.”
There’s a lot of data on sickle cell disease and how it affects people. About 300,000 children are born with it every year around the world.
| Region | Estimated Prevalence | Annual Births with SCD |
| Sub-Saharan Africa | High | 240,000 |
| India and the Middle East | Moderate | 50,000 |
| North America and Europe | Low | 10,000 |
These numbers show we need to keep working on finding better treatments and care for sickle cell disease.
It’s important to know the different types of sickle cell disease. Each type is based on a specific mutation in the hemoglobin gene.
Sickle cell anemia, or Hemoglobin SS, is the most common and severe form. It happens when a person gets two mutated HBB genes, one from each parent. This leads to the production of hemoglobin S (HbS).
Hemoglobin SS is linked to more severe and frequent crises. It also increases the risk of serious health problems.
Hemoglobin SC disease is another important variant. It occurs when a person has one HbS gene and one HbC gene. This type is milder than sickle cell anemia but can cause health issues.
People with Hemoglobin SC disease might have fewer crises than those with Hemoglobin SS. Yet, they can face complications like splenic sequestration and higher infection risks.
S-Beta thalassemia happens when a person has one HbS gene and one beta-thalassemia gene. The severity can vary a lot, depending on the beta-thalassemia mutation.
There are two main types of S-Beta thalassemia. S-Beta zero thalassemia means no normal hemoglobin is made, and S-Beta plus thalassemia means some is made. Zero thalassemia is usually more severe.
There are also rare variants of sickle cell disease. These include combinations with other abnormal hemoglobin genes like HbD and HbE. These rare types can have unique symptoms and complications.
It’s key to understand these rare types for proper care and management.
| Genotype | Description | Severity |
| Hemoglobin SS | Sickle Cell Anemia | Severe |
| Hemoglobin SC | Hemoglobin SC Disease | Mild to Moderate |
| S-Beta Thalassemia | S-Beta Thalassemia Variants | Variable |
Sickle cell disease follows an autosomal recessive pattern. This affects family planning and genetic counseling. It means the disease comes from a mutation in an autosomal chromosome. An individual needs two defective copies of the gene, one from each parent, to have the disease.
Carriers of the disease have one normal and one mutated gene. They usually don’t show the full symptoms but can pass the mutated gene to their kids. If both parents are carriers, there’s a 25% chance their child will have the disease.
There’s also a 50% chance the child will be a carrier like the parents. And a 25% chance the child will have two normal genes and not have the disease or be a carrier.
It’s important to know the difference between sickle cell trait and sickle cell disease. People with sickle cell trait are carriers. They have one normal and one sickle-cell hemoglobin gene. They usually live normal lives, but can pass the sickle gene to their kids.
On the other hand, those with sickle cell disease have two sickle hemoglobin genes. This leads to abnormal hemoglobin production. It causes red blood cells to sickle.
| Condition | Genotype | Health Implications |
| Sickle Cell Trait | One normal gene, one sickle gene | Generally healthy, but can pass the sickle gene to offspring |
| Sickle Cell Disease | Two sickle genes | Can experience sickling of red blood cells, leading to various health issues |
Genetic counseling is key for families with sickle cell disease history. Counselors help understand the risks of passing the disease to future generations. They discuss reproductive options. This helps families make informed decisions about having children.
Carrier testing shows if someone carries the sickle cell gene. It’s critical for couples planning to have kids, with a family history of the disease. Knowing if you’re a carrier helps assess the risk of having a child with sickle cell disease.
Sickle Cell Disease (SCD) causes many problems that affect patients’ lives a lot. These issues start around 5 to 6 months old, when the protection from fetal hemoglobin goes away. We will look at the different health issues and complications SCD can cause.
A big problem in SCD is the vaso-occlusive crisis (VOC). It happens when sickled red blood cells block blood vessels. This leads to pain and tissue damage.
These pain episodes can be very bad and sometimes need hospital care. Knowing what triggers them and how to prevent them is key to managing VOC.
SCD can damage organs like the spleen, kidneys, and lungs over time. This is because of repeated blockages in blood vessels.
Chronic organ damage can cause long-term health problems. For example:
People with SCD get sick more easily because their spleen doesn’t work right. This is because of damage from repeated blockages.
To prevent infections, it’s important to:
The health problems caused by SCD really affect people’s lives. They deal with chronic pain, frequent hospital stays, and the emotional toll of a chronic illness.
It’s vital to have a full care plan. This includes managing pain, mental health support, and social services. It helps improve the quality of life for those with SCD.
Early diagnosis of sickle cell disease is key for better management and outcomes. We have many ways to diagnose it, from newborn screening to genetic testing.
Newborn screening for sickle cell disease is vital. Many places screen all newborns for this condition soon after birth. Early detection leads to timely treatment, improving life quality for babies.
These screenings use a blood test from a heel prick. They check for abnormal hemoglobin. The benefits include:
Hemoglobin electrophoresis helps diagnose sickle cell disease. It separates hemoglobin types to find Hemoglobin S, the disease’s cause.
Blood tests like complete blood counts (CBC) and reticulocyte counts also help. They show signs of anemia, infection, and other issues.
Genetic testing is essential for diagnosing sickle cell disease. It helps find carriers and confirm the disease in suspected cases. Polymerase chain reaction (PCR) and DNA sequencing find the HBB gene mutation.
Genetic testing is great for:
Prenatal diagnosis can spot sickle cell disease in the fetus. CVS and amniocentesis give genetic material for analysis. This helps parents decide about their pregnancy.
This is very important for families with sickle cell history. It allows for early planning and care for affected children.
Living with sickle cell disease means understanding the condition well. It’s caused by a genetic mutation that makes red blood cells sickle. This leads to health problems like vaso-occlusive crises and infections.
New medical research offers hope for those with sickle cell disease. Gene therapies, which modify blood cells, have shown great promise. In 2023, new gene therapies were approved, marking a big step forward.
Looking ahead, we need more research and support for sickle cell disease patients. We must find new treatments and care strategies. This way, we can help those with sickle cell disease live better, healthier lives.
Sickle cell disease is a group of inherited disorders. It affects the hemoglobin molecule in red blood cells. This causes cells to take on a sickle-like shape.
It’s caused by a point mutation in the HBB gene. This mutation leads to abnormal hemoglobin, known as Hemoglobin S (HbS).
The sickling process happens when HbS polymerizes under certain conditions. This causes red blood cells to become sickle-shaped. This can lead to various health issues.
There are different genotypes and variants. These include sickle cell anemia (Hemoglobin SS), Hemoglobin SC disease, S-beta thalassemia, and other rare variants.
It’s inherited in an autosomal recessive pattern. This means an individual must inherit two copies of the mutated gene (one from each parent) to express the disease.
The sickle cell trait means an individual has one normal and one mutated HBB gene. Sickle cell disease occurs when an individual has two mutated genes. This leads to the expression of the disease.
Diagnosis is usually through newborn screening programs. It’s also done with hemoglobin electrophoresis, genetic testing, and prenatal diagnosis options.
Symptoms include vaso-occlusive crises and chronic organ damage. Individuals are also more susceptible to infections. This significantly impacts their quality of life.
It’s found worldwide, with a higher prevalence in areas where malaria is or was prevalent. This is because the sickle cell trait offers protection against malaria.
Yes, there are ongoing advancements. Gene therapy and new treatments aim to improve management and quality of life for those affected.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!