Last Updated on November 27, 2025 by Bilal Hasdemir
Thoracic surgery is a big deal and needs careful recovery. Many patients wonder when they can start driving again. Getting back to driving is important for feeling independent, but safety comes first.
After thoracic surgery, your body needs time to heal. Post-thoracic surgery recovery is not just about physical healing. It’s also about getting your strength and mobility back. It’s important to follow your doctor’s advice to avoid problems and have a smooth recovery.
Knowing about driving restrictions after surgery is key for your safety and the safety of others. We’ll help you understand when you can start driving again and other normal activities after thoracic surgery.
Key Takeaways
- Recovery time varies among individuals after thoracic surgery.
- Medical guidelines are vital for safe recovery and resuming activities.
- Understanding driving restrictions is key to avoiding complications.
- Resuming normal activities should be done under medical supervision.
- Patient safety and the safety of others are most important.
The Impact of Thoracic Surgery on Daily Activities
Thoracic surgery can change your daily life a lot. The effects depend on the surgery type. These surgeries can be on the lungs, heart, or esophagus. Each one has its own recovery and challenges.
Common Types of Thoracic Procedures
Thoracic surgeries include lung, heart, and esophageal operations. Lung surgeries like lobectomy or pneumonectomy affect breathing and movement. Heart surgeries, like CABG, impact heart function and require a long recovery. Esophageal surgeries, like esophagectomy, can make eating hard and require diet changes.
- Lung Surgeries: Procedures like lobectomy or pneumonectomy can significantly affect a patient’s respiratory function and overall mobility.
- Heart Surgeries: Surgeries such as CABG or valve repair/replacement impact cardiac function and may require a substantial recovery period.
- Esophageal Surgeries: Esophagectomy, for instance, can affect a patient’s ability to swallow and digest food, necessitating dietary changes.
How Surgery Affects Mobility and Function
Thoracic surgery can limit your movement and function. This is mainly due to pain, the incision, and how your body reacts. Patients often find it hard to lift, bend, or stretch.
Key aspects affected include:
- Pain and Discomfort: Post-operative pain can limit a patient’s ability to move freely or perform daily activities.
- Reduced Lung Capacity: Surgeries involving the lungs can temporarily reduce lung capacity, affecting endurance and stamina.
- Cardiac Function: Heart surgeries can impact cardiac function, necessitating a period of recovery before resuming strenuous activities.
Knowing these impacts helps manage expectations and plan recovery. By understanding the challenges, patients can prepare better for their recovery journey.
General Recovery Timeline After Chest Surgery
After chest surgery, patients follow a general recovery timeline. This timeline helps them get back to normal activities. The recovery time varies based on the surgery type and individual health.
Hospital Stay and Immediate Recovery (0-2 weeks)
The recovery starts right after surgery, in the hospital. Most patients leave the hospital in 1 to 2 weeks. During this time, they do gentle movements and breathing exercises to aid healing.
Immediate post-surgery care focuses on pain management, infection monitoring, and increasing mobility. Patients often need a caregiver for the first few days at home.
Early Recovery Phase (2-6 weeks)
After leaving the hospital, patients start the early recovery phase. They continue to heal and build strength. It’s key to follow the surgeon’s advice on medication, activity, and appointments.
Patients may feel tired, in pain, and have limited mobility. But these feelings get better over time. They can start doing light activities like short walks and simple tasks. But they should avoid heavy lifting and strenuous exercises.
Advanced Recovery Phase (6+ weeks)
The advanced recovery phase is when healing and strength gain are significant. Most patients can go back to their usual activities, like driving and work, depending on their job and the surgeon’s advice. It’s important to keep up with follow-up care and report any unusual symptoms.
At this stage, patients can start to increase their physical activity and do more strenuous exercises. The goal is to maintain a healthy lifestyle and follow any ongoing treatment plans.
Driving After Thoracic Surgery: Standard Medical Guidelines

Medical guidelines help decide when it’s okay to drive after thoracic surgery. These rules are made to keep patients and others safe on the road. They consider the surgery type, how well the patient is recovering, and the risks of driving too early.
Recommendations from American Medical Associations
The American Medical Association (AMA) and other groups give advice on driving after surgery. They usually say patients should not drive for a while after thoracic surgery. How long depends on the surgery’s complexity and the patient’s recovery.
The AMA says patients should stop using narcotic pain meds and be able to drive safely. This is usually after the first recovery phase, which can be 2-6 weeks. But, it can vary.
Scientific Rationale Behind Driving Restrictions
The main worry is if patients can drive safely after thoracic surgery. They need to react quickly, not be on narcotic meds, and have enough strength and mobility. Studies show thoracic surgery patients might have slower reaction times and physical limits that affect driving.
Driving too soon can also lead to problems like wound issues or making health conditions worse. So, the guidelines aim to reduce these risks and help patients recover safely.
Variations in Guidelines Based on Procedure Type
The type of thoracic surgery affects when patients can drive again. For example, those with minimally invasive procedures might drive sooner than those with open surgery. The surgery’s extent, the patient’s health, and any complications also play a big role in when it’s safe to drive.
| Type of Thoracic Surgery | Typical Driving Restriction Period | Key Considerations |
| Minimally Invasive Thoracic Surgery | 2-4 weeks | Less tissue trauma, potentially quicker recovery |
| Open Thoracic Surgery | 4-6 weeks or more | Greater tissue disruption, longer recovery time |
| Thoracic Surgery with Complications | Varies, potentially longer than 6 weeks | Complications can prolong recovery and impact driving readiness |
Knowing these guidelines and why they exist helps patients plan their recovery and decide when to drive again. It’s key to follow the advice from healthcare providers, as each situation is different.
Factors That Influence Your Return to Driving
Many things affect when you can drive again after thoracic surgery. The recovery process is complex. It depends on the surgery type, your health, and how fast you recover.
Surgical Approach: Open vs. Minimally Invasive
The surgery method greatly impacts recovery time and when you can drive. Minimally invasive surgeries, like VATS, cause less damage. This means you might recover faster than with open surgery.
“Patients with minimally invasive surgeries often feel less pain,” says Dr. Jane Smith, a thoracic surgeon. “They can get back to driving sooner than those with open surgery.” This is because these surgeries use smaller cuts and cause less muscle damage.
Individual Recovery Rate and Complications
Every patient recovers differently after thoracic surgery. Your health, age, and any complications can affect this. Complications like infection or bleeding can make recovery longer and delay driving.
It’s key to listen to your surgeon and report any unusual symptoms. This helps avoid complications and ensures a safe return to driving.
Age and Pre-existing Health Conditions
Your age and health before surgery also matter. Older patients or those with health issues like diabetes may need more time to recover. They should be careful when starting to drive again.
A study in the Journal of Thoracic Surgery found that older patients and those with health problems face higher risks. They might need longer to recover. It’s important for them to work with their healthcare team to set a safe driving timeline.
Pain Management and Its Effect on Driving Safety
Managing pain after thoracic surgery is key for recovery. But it also affects when a patient can safely drive again.
Common Pain Medications After Thoracic Surgery
Patients often get a mix of meds to control pain after thoracic surgery. These include:
- Opioids: These strong pain relievers can make you sleepy and slow your reaction time.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): They help with pain and swelling but might upset your stomach.
- Acetaminophen: Used with other meds to ease pain and lower fever.
Legal Implications of Driving While on Prescription Medications
Driving on some prescription meds can lead to serious legal trouble. It’s important to know the laws about driving on these meds. In many places, it’s a crime, like driving drunk.
Key Considerations:
- Always take your meds as your doctor says.
- Know how your meds might affect your driving.
- If you’re not sure about driving on your meds, talk to your doctor or pharmacist.
Understanding how pain meds affect driving and knowing the legal issues helps patients make smart choices about driving after surgery.
Physical Requirements for Safe Driving Post-Surgery
Driving safely after thoracic surgery needs a good level of physical fitness. This fitness is often lower after surgery. Driving demands range of motion, quick reaction, and endurance, all of which can be impacted by surgery.
Necessary Range of Motion for Driving
Safe driving needs good shoulder, elbow, and neck mobility. After thoracic surgery, patients might have less mobility due to pain or surgery limits. Studies show that full mobility is key for safe driving.
A study in the Journal of Thoracic Surgery found that shoulder and elbow mobility are vital for safe driving. It showed that those with less mobility are more likely to have driving accidents.
Reaction Time and Emergency Maneuvers
Quick reactions are critical for emergency situations on the road. Thoracic surgery can slow down reaction times due to pain, medication, or fitness loss. It may take weeks for reaction times to get back to normal.
A study in the Journal of Surgical Research found that thoracic surgery patients had slower reaction times at first. But, with rehab, most regained their pre-surgery reaction times.
| Physical Attribute | Pre-Surgery Level | Post-Surgery Level (Initial) | Post-Surgery Level (After Rehabilitation) |
| Range of Motion | Full | Limited | Near Full |
| Reaction Time | Normal | Delayed | Normal |
| Endurance | High | Low | Moderate |
Endurance for Various Driving Conditions
Driving endurance is also key for safe driving, like on long trips or in heavy traffic. Thoracic surgery can lower endurance due to fatigue and fitness loss. Slowly increasing driving time and frequency can boost endurance.
The American Thoracic Society advises starting with short drives and gradually increase time as endurance grows. This helps regain the physical fitness needed for safe driving.
When Can I Drive After Lung Surgery?
Getting back to driving after lung surgery depends on your recovery and the surgery type. The time it takes to recover varies with lobectomy, pneumonectomy, or VATS.
Lobectomy Recovery and Driving Timeline
A lobectomy removes a lung lobe, often for lung cancer. Recovery times differ, but usually, you should not drive for 2-4 weeks. You might feel pain, discomfort, or be less mobile, making driving unsafe.
Your doctor will give specific driving advice. Your health, any complications, and pain management are key factors.
Pneumonectomy Recovery Considerations
A pneumonectomy removes a whole lung, requiring a longer recovery than lobectomy. You might need 6-8 weeks or more before driving again.
Removing a lung affects your strength and endurance. Make sure you’re physically ready to drive.
Video-Assisted Thoracoscopic Surgery (VATS) Recovery
VATS is a less invasive surgery with quicker recovery times. You might drive again in 1-3 weeks after VATS.
Yet, always follow your doctor’s advice. Your comfort and ability to handle emergencies while driving are important.
Recovering from lung surgery is unique for everyone. Prioritize your safety and the safety of others by carefully checking if you’re ready to drive.
When Can I Drive After Heart Surgery?
After heart surgery, many patients wonder when they can drive again. The answer varies based on the surgery type, recovery pace, and doctor’s advice.
Coronary Artery Bypass Grafting (CABG) Recovery
CABG surgery is major and needs a lot of recovery time. Doctors usually say no driving for 4 to 6 weeks. This helps the sternum heal and lowers the risk of problems.
It’s important to follow the doctor’s advice on physical activity, including driving. Recovery means not just healing but also managing pain and getting stronger.
Valve Replacement or Repair Recovery
Valve surgeries also need careful recovery. Driving rules are often the same as CABG, from 4 to 6 weeks. But, the exact time depends on your health and surgery complexity.
Listen to your body and your doctor’s advice on when to start driving again.
Minimally Invasive Cardiac Procedures
Minimally invasive surgeries have shorter recovery times. Some might drive in 1 to 3 weeks. But, always follow your surgeon’s specific advice.
When you can drive depends on your full recovery and ability to drive safely.
To sum up, recovery and driving readiness vary by surgery and individual. Here’s a quick look at typical recovery times for different heart surgeries:
| Surgical Procedure | Typical Recovery Time | Driving Restrictions |
| CABG | 6-12 weeks | 4-6 weeks |
| Valve Replacement/Repair | 6-12 weeks | 4-6 weeks |
| Minimally Invasive Cardiac Surgery | 3-6 weeks | 1-3 weeks |
Talking to your healthcare provider is key to getting advice on driving after heart surgery.
Recovery After Esophageal and Other Thoracic Surgeries
Recovering from thoracic surgeries like esophagectomy and thymectomy needs careful planning. These surgeries are complex and require a detailed approach for a smooth recovery.
Esophagectomy Recovery Timeline
Esophagectomy, or removing the esophagus, is a big surgery. Patients usually stay in the hospital for 1-2 weeks after surgery. They are watched closely for any problems.
At home, recovery can take weeks. Patients must follow a special diet and avoid hard work. It can take several months to fully recover. Most people can get back to normal in 3-6 months. But, recovery time can differ based on health and surgery details.
Thymectomy and Mediastinal Surgery Recovery
Thymectomy, or removing the thymus gland, also needs careful recovery planning. Less invasive methods can help speed up recovery. But, patients must give their body time to heal.
Mediastinal surgery, in the space between the lungs, also needs a special recovery plan. Patients should avoid heavy lifting and bending. They must follow their surgeon’s post-operative care instructions.
Chest Wall Resection and Reconstruction
Chest wall resection and reconstruction involve removing and rebuilding chest wall parts. This complex surgery needs a long recovery time. Patients must be watched for complications and supported with pain management and physical therapy.
The recovery time for chest wall resection varies. But, patients usually need months to get strong again. Regular follow-up with their healthcare team is key for a good recovery.
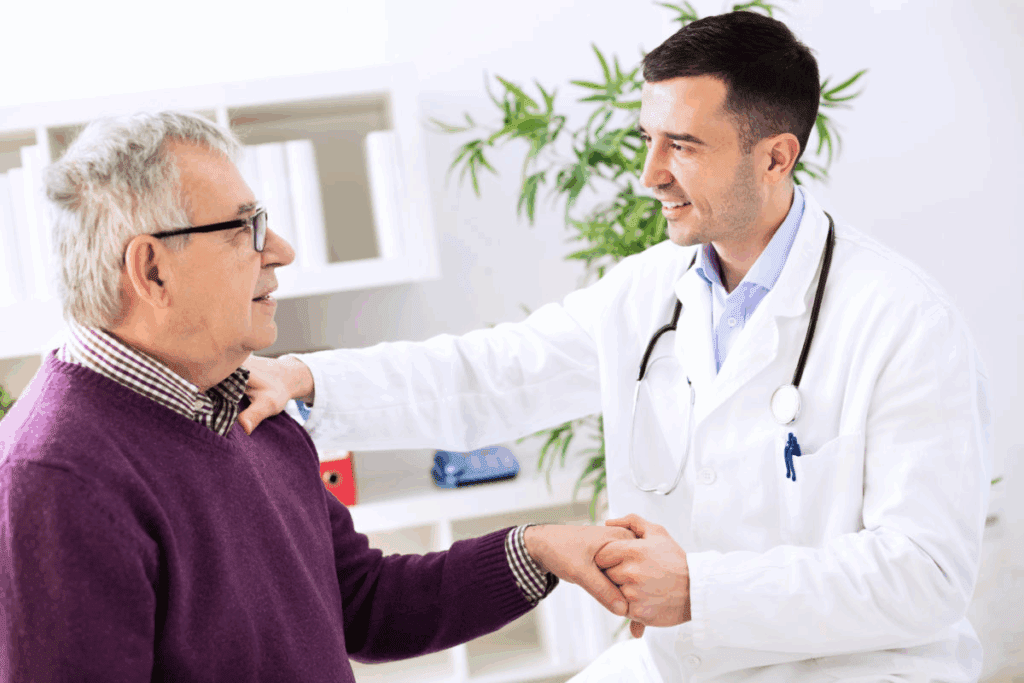
Your Surgeon’s Role in Determining Driving Readiness
Your surgeon is key in deciding when you can drive again after thoracic surgery. The recovery is complex. Their expert advice is vital in checking if you’re ready to drive.
Key Questions to Ask During Follow-up Appointments
At follow-up visits, ask important questions to track your progress and any limits. You should discuss your physical strength, pain control, and any meds that might impact driving. Some questions to ask include: “What shows I’m getting better?”, “What should I avoid?”, and “How will I know I’m ready to drive?”
- What are the signs that I’m recovering well?
- Are there any activities I should avoid?
- How will I know when I’m ready to drive again?
Medical Clearance Process
Getting medical clearance to drive is a big step in your recovery. Your surgeon will check your health, including your movement, reaction speed, and any risks. They’ll decide if it’s safe for you to drive again. This is for your safety and the safety of others on the road.
Medical clearance is a personalized process that considers your surgery and recovery details. It’s not a standard decision.
Second Opinions and Specialist Consultations
Getting a second opinion or talking to specialists can give more insight into your recovery and driving readiness. This is helpful if you’re unsure about your surgeon’s advice or have unusual symptoms. A second opinion can give you peace of mind and help you decide when to start driving again.
It’s your right as a patient to seek additional medical opinions if you’re unsure about any part of your care, including when it’s safe to start driving again.
Warning Signs That Indicate You’re Not Ready to Drive
Knowing when you’re not ready to drive after thoracic surgery is key for your safety and others’. Your body changes a lot after such a big surgery. These changes can affect your ability to drive safely.
Physical Warning Signs
There are physical signs that show you might not be ready to drive. These include:
- Persistent Pain: If pain is not managed well or gets worse, it can make driving unsafe.
- Reduced Mobility: If you can’t move your neck, shoulders, or chest well, it’s hard to control your car.
- Fatigue: Feeling very tired or weak can slow down your reaction time, making driving risky.
- Dizziness or Lightheadedness: Feeling dizzy or lightheaded means you might not be ready to drive. It could cause you to lose control of your car.
Medical experts say it’s important to listen to your body and not push yourself too hard.
“The key to safe driving after surgery is not just about the absence of pain but also about having the physical capability to react and maneuver the vehicle effectively.”
Cognitive and Medication-Related Warning Signs
Some signs in your mind and from your medicine can also tell you not to drive. These include:
- Confusion or Disorientation: Feeling confused or disoriented means you should not drive.
- Medication Side Effects: Some pain medicines or other drugs can make you less able to judge and react while driving.
- Impaired Judgment: If you’re not sure you can make quick decisions on the road, it’s best not to drive.
It’s important to follow your doctor’s advice about medicine and driving. Always talk about your medicine’s side effects with your healthcare provider.
Knowing these warning signs helps you decide when it’s safe to drive again after thoracic surgery. Always check with your healthcare provider if you’re not sure if you’re ready to drive.
Practical Tips for Resuming Driving Safely
When you start driving again after thoracic surgery, safety and comfort are key. You need to balance wanting to drive on your own with keeping yourself and others safe.
Gradual Return Strategy
It’s important to get back to driving slowly. Start with short, easy routes during quiet times. This helps you get used to driving again without too much stress.
Begin in a safe place like an empty parking lot. This lets you check how you feel and how well you react. Having someone with you can also help. They can help you navigate and give feedback on how you’re doing.
Vehicle Modifications and Seat Adjustments
Changing your car to fit you better can make a big difference. Make sure your seat is set right to avoid putting pressure on your chest area. Using a lumbar support or adjusting the seatback can help you stay comfortable.
Think about making your car easier to get in and out of. A steering wheel cover or adjusting the steering wheel can help. Some people might also need special tools to help them drive longer without getting tired.
Emergency Preparedness While Driving
Being ready for emergencies is very important when you’re driving after surgery. Keep a kit in your car with things like a first-aid kit, phone charger, and basic tools.
Also, have a list of important phone numbers with you. Tell your family or caregivers about your driving plans. This way, someone knows where you are and can help if you need it.
By following these tips, you can safely start driving again after thoracic surgery. It helps you get back to your normal life smoothly.
Legal and Insurance Considerations Post-Thoracic Surgery
After thoracic surgery, patients face a complex recovery. They must heal medically and deal with legal and insurance matters, like driving. “The decision to drive after thoracic surgery involves not only medical clearance but also legal and insurance considerations,” as it can impact both personal safety and financial liability.
Liability Issues If Driving Against Medical Advice
Driving against medical advice after thoracic surgery can lead to big liability issues. If a patient is in an accident while driving against doctor’s orders, they might be legally responsible for damages or injuries. This is because driving under such conditions could be seen as negligent, if the patient’s medical condition played a part in the accident.
Key Considerations for Liability:
- Understanding the legal implications of driving against medical advice
- Potential consequences of being involved in an accident while not medically cleared to drive
- The role of medical records in determining liability
Insurance Coverage Concerns
Insurance coverage is key when starting to drive again after thoracic surgery. Patients should know that driving against medical advice might void their insurance in an accident. Insurance companies often have clauses that exclude coverage for activities against medical advice.
“Insurance policies typically include provisions that may void coverage if the insured engages in activities that are contrary to medical advice, potentially leaving the driver financially exposed in case of an accident.”
Documentation to Keep in Your Vehicle
It’s wise for patients to keep certain documents in their vehicle after thoracic surgery. This includes:
- A copy of their medical clearance letter
- Records of their surgery and recovery progress
- Any relevant insurance information
Having this documentation ready can help in emergencies or if stopped by police. It shows their medical status and if they followed their doctor’s orders.
Alternative Transportation Options During Recovery
Patients who have had thoracic surgery need to find new ways to get around. They can’t drive right away. So, they look for other ways to get to doctor’s appointments and keep up with daily life.
Rideshare and Medical Transportation Services
Rideshare services like Uber and Lyft are great for getting to medical visits. Some even offer special services for health needs. There are also medical transportation services for those who need more help.
These services are good for people without cars or who can’t use public transport. It’s important to tell the driver about any special needs you have.
Public Transportation Accessibility
Public transport is another good choice for getting around. Many cities have buses and trains that are easy to use for people with mobility issues. You can use them to get to appointments, shop, or visit loved ones.
To make the most of public transport, plan your trip ahead of time. Use apps or websites to find the best route. Also, check if you can get discounts because of your age or disability. Make sure you have any mobility aids you need.
Family and Community Support Networks
Having family and friends help is key to getting better. They can drive you to appointments, do errands, and offer emotional support. It’s a big help during a tough time.
You can also use community resources like volunteer driver programs or non-profit groups. They offer rides and help you feel less alone during recovery.
| Transportation Option | Benefits | Considerations |
| Rideshare Services | Convenient, flexible, and widely available | May require advance booking, costs can add up |
| Public Transportation | Cost-effective, accessible in many areas | May require more time and planning, accessibility varies |
| Family and Community Support | Emotional support, flexible, and potentially cost-free | Dependent on the availability of supporters, may impose on others |
Comparing Driving to Other Post-Surgical Activities
After thoracic surgery, it’s important to know how different activities affect our healing. Driving is just one activity patients need to think about after surgery.
Returning to Work Timeline
The time it takes to go back to work after thoracic surgery varies. It depends on the job and the surgery type. Desk jobs might allow a return in 2-4 weeks, if the job doesn’t require much physical effort.
But, jobs that are very physical might take 6-12 weeks or more. It’s key to talk to your doctor about your job to know when it’s safe to go back.
Exercise and Physical Activity Progression
Starting to exercise is important for a good recovery after thoracic surgery. Begin with gentle movements and slowly add more intense activities. Walking is often recommended first to help prevent blood clots.
As you get better, you can do more intense exercises. But, always follow your doctor’s advice to avoid pushing too hard.
Air Travel and Long-Distance Journeys
Air travel and long trips can be risky after thoracic surgery. They can lead to deep vein thrombosis (DVT) and the strain of sitting for a long time. Doctors usually advise against flying or long car trips for 4-6 weeks after surgery.
On long trips, move often, drink plenty of water, and wear compression stockings to lower DVT risk.
| Activity | Typical Recovery Time Before Resuming | Precautions |
| Returning to Desk Work | 2-4 weeks | Discuss with healthcare provider |
| Returning to Physical Work | 6-12 weeks | Avoid heavy lifting, bending |
| Gentle Exercise (e.g., Walking) | 1-2 weeks | Start slow, progress gradually |
| Strenuous Exercise | 6-8 weeks | Follow healthcare provider’s guidance |
| Air Travel | 4-6 weeks | Move regularly, stay hydrated |
Conclusion: Balancing Recovery Needs with Independence
Thoracic surgery is a big deal and needs careful recovery and rehab. It’s important to balance recovery needs with wanting to be independent. We must think about many things, like the surgery type, how fast you recover, and your health before surgery.
Following doctor’s advice is key to a safe recovery. Don’t rush back to daily tasks, like driving. Knowing when you’re ready to drive is important. This balance helps you get back to normal while staying safe and healthy.
We suggest being patient and working with your healthcare team. This way, you can handle your recovery well and get back to your usual life with confidence.
FAQ
How long after thoracic surgery can I drive?
The time to start driving again after thoracic surgery varies. It depends on the surgery type, how fast you recover, and your doctor’s advice. Usually, doctors say wait at least 4-6 weeks.
What factors influence my ability to drive after thoracic surgery?
Several things can affect your driving ability after thoracic surgery. These include the surgery method, how quickly you recover, any complications, your age, and any health issues you had before.
Can I drive after taking pain medication following thoracic surgery?
It’s not safe to drive on strong pain meds. They can slow down your reaction time and judgment. Always listen to your doctor and follow the medicine’s instructions.
How do I know if I’m ready to drive after thoracic surgery?
You’re ready to drive when you have enough strength, movement, and quick thinking. Your doctor will check this during follow-up visits. It’s important to follow their advice.
Are there specific considerations for driving after lung surgery?
Yes, lung surgery type affects when you can drive. More complex surgeries might mean waiting longer to drive.
Can I drive after heart surgery, and when?
When you can drive after heart surgery depends on the surgery type. Usually, doctors say wait 4-6 weeks. But, it can vary based on your recovery and doctor’s advice.
What are the warning signs that I’m not ready to drive after thoracic surgery?
Warning signs include ongoing pain, limited movement, feeling sleepy or dizzy from meds, and trouble thinking clearly. If you notice these, don’t drive.
Are there alternative transportation options during my recovery?
Yes, you can use rideshare services, public transport, or get help from family and friends. These options help you move around without driving.
How does driving after thoracic surgery compare to other post-surgical activities?
Driving readiness is compared to returning to work, exercising, and flying. Recovery times differ, but always follow your doctor’s advice for each activity.
What should I do if I’m unsure about my ability to drive after thoracic surgery?
If you’re unsure, talk to your surgeon or healthcare provider. They can check your condition and tell you when it’s safe to drive again.
Are there any legal or insurance considerations I should be aware of when resuming driving after thoracic surgery?
Yes, driving against doctor’s orders could lead to legal issues. Also, check your insurance. Keep your medical clearance in your car.
Reference
- Bellmann, P., et al. (2022). Driving ability after right-sided inguinal hernia surgery. Springer Nature. https://pubmed.ncbi.nlm.nih.gov/33825012/