Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 700,000 people in the United States have gallbladder removal surgery each year. Some of them might face a condition called dumping syndrome. This happens when food, rich in sugar, moves too fast from the stomach to the small intestine. Explaining Dumping Syndrome After Gallbladder Removal symptoms and dietary triggers.
We will look into the reasons and signs of this issue. This will help you know what to expect if you’ve had gallbladder surgery. Knowing about dumping syndrome can help you manage your symptoms better. This can improve your life quality.
Key Takeaways
- Understand the definition and causes of dumping syndrome.
- Learn about the symptoms and effects of dumping syndrome.
- Discover ways to manage and alleviate symptoms.
- Find out how to improve your quality of life after gallbladder surgery.
- Gain insights into the relationship between gallbladder removal and dumping syndrome.
Dumping Syndrome After Gallbladder Removal: An Overview
Dumping syndrome is often linked to stomach surgery. But it can also happen after gallbladder removal. We’ll look at what dumping syndrome is, how it works, and how common it is after gallbladder surgery.
Definition and Pathophysiology
Dumping syndrome is a set of symptoms caused by food, mainly sugar, moving too fast into the small intestine. It affects both the stomach and blood vessels.
When food moves quickly into the small bowel, it pulls water into the intestine. This leads to bloating, pain, and diarrhea.
Also, hormones from the stomach play a big part in dumping syndrome symptoms.
Prevalence in Postcholecystectomy Patients
The number of people with dumping syndrome after gallbladder surgery varies. Most cases happen after stomach or esophagus surgery.
But, it can also occur after gallbladder surgery. The exact number of cases is not clear. Studies show it can happen a lot, so doctors need to know about it.
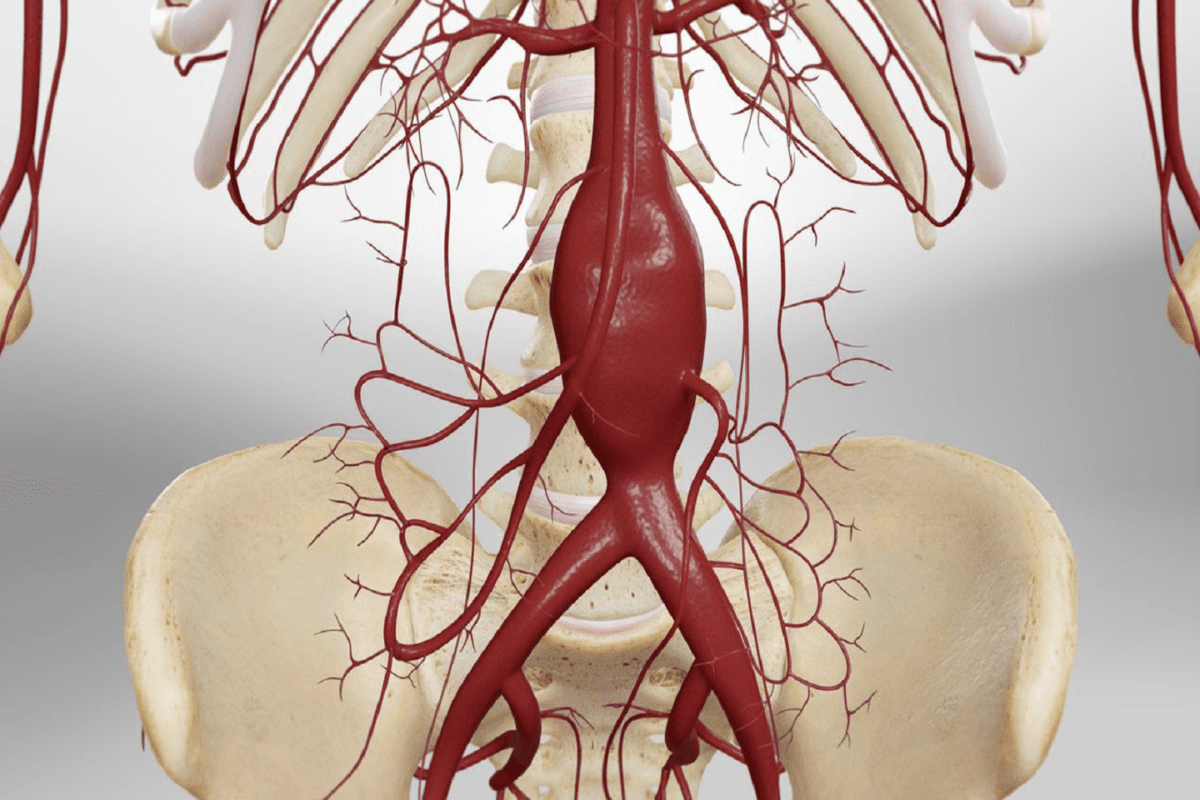
The Gallbladder’s Role and Consequences of Its Removal
The gallbladder stores bile, a digestive fluid from the liver. It releases bile into the small intestine to help digest fats. Knowing this helps us understand the changes after it’s removed.
Normal Bile Storage and Release Function
The gallbladder holds bile and releases it into the bile duct. This duct then empties into the small intestine. Eating fatty foods triggers this release through a hormone called cholecystokinin (CCK).
Bile salts break down fats, making them easier for enzymes to digest. This is key for absorbing fat-soluble vitamins.
Digestive Changes Following Cholecystectomy
Without a gallbladder, bile flows straight from the liver to the small intestine. This can cause digestive changes and some complications. People might have diarrhea or loose stools because of this constant bile flow.
Digestive Change | Description | Potential Impact |
Constant Bile Flow | Bile flows directly into the small intestine | Diarrhea or loose stools |
Altered Fat Digestion | Less efficient emulsification of fats | Potential for malabsorption of fat-soluble vitamins |
Changes in Bowel Habits | Variability in bowel movements | Inconvenience and possible dehydration |
It’s important to understand these changes to manage symptoms and adjust to life without a gallbladder. While some might not face big issues, others may need to change their diet. This helps deal with gallbladder function loss and post-surgery complications.
Postcholecystectomy Syndrome: Understanding the Broader Context
Removing the gallbladder can cause many problems, known as postcholecystectomy syndrome. This condition includes symptoms that people may face after gallbladder surgery. It’s important to know about postcholecystectomy syndrome to handle its complications.
Common Post-Gallbladder Surgery Complications
Patients might face issues like digestive problems, bile duct injuries, and other stomach issues after gallbladder removal. Some common problems include:
- Bile duct obstruction or injury
- Digestive changes, such as diarrhea or fatty stools
- Abdominal pain or discomfort
- Nausea and vomiting
These issues can really affect a person’s life. It’s key to know what causes them and how to manage them.
How Dumping Syndrome Fits Within Postcholecystectomy Syndrome
Dumping syndrome is a complication that can happen after gallbladder surgery. It’s when food moves too fast into the small intestine, causing stomach and blood flow problems. Dumping syndrome is a big part of postcholecystectomy syndrome, adding to the symptoms patients face.
We’ll look into dumping syndrome’s symptoms and how to manage them later. But it’s important to see dumping syndrome as part of a larger set of complications from cholecystectomy.
Understanding postcholecystectomy syndrome and its parts, like dumping syndrome, helps doctors create better treatment plans. This can lead to better results for patients.
Early vs. Late Dumping Syndrome: Timing of Symptoms
Knowing when dumping syndrome symptoms happen is key to managing it well. It’s a complication that can happen after gallbladder removal. Symptoms can be split into early and late dumping syndrome, based on when they start.
Immediate Post-Meal Symptoms (Within 30 Minutes)
Early dumping syndrome hits fast, usually within 30 minutes after eating. You might feel stomach cramps, diarrhea, and flushing. These happen because food moves too quickly into the small intestine, causing fluid shifts and discomfort.
Delayed Symptoms (1-3 Hours After Eating)
Late dumping syndrome kicks in 1 to 3 hours after eating. Symptoms include low blood sugar, dizziness, and feeling tired. These symptoms come from too much insulin being released after a meal.
Severity Spectrum and Impact on Daily Activities
Dumping syndrome symptoms can be mild or very severe. For some, it’s just a little discomfort, but for others, it can really disrupt their day. It can also affect how you feel mentally, making meal times stressful.
Symptom Timing | Common Symptoms | Possible Causes |
Early (Within 30 minutes) | Abdominal cramps, diarrhea, flushing | Rapid emptying of food into the small intestine |
Late (1-3 hours after eating) | Hypoglycemia, dizziness, fatigue | Excessive insulin release |
Understanding dumping syndrome symptoms helps manage the condition better. By making dietary changes and using other strategies, you can handle both early and late symptoms. This can greatly improve your life quality.
Recognizing Symptoms of Dumping Syndrome
Dumping syndrome can happen after you have your gallbladder removed. It has specific symptoms that are important to know. These symptoms can really affect your life, so it’s key to catch them early and manage them well.
Gastrointestinal Manifestations
The symptoms you feel first are usually in your stomach. You might have:
- Abdominal cramps
- Diarrhea
- Nausea
- Bloating
These happen because food moves too fast into your small intestine. This can upset your digestion.
Vasomotor and Cardiovascular Symptoms
People with dumping syndrome also face other symptoms. These include:
- Flushing
- Dizziness or lightheadedness
- Rapid heart rate (tachycardia)
- Sweating
These symptoms come from how your body reacts to quick changes in blood sugar and fluid.
Hypoglycemic Episodes in Late Dumping
Late dumping happens 1-3 hours after you eat. It can cause low blood sugar. Signs of low blood sugar are:
- Shakiness
- Confusion
- Dizziness
- Hunger
These happen because your body makes too much insulin after eating too much sugar.
Knowing all the symptoms of dumping syndrome is important for managing it. Here’s a quick guide:
Symptom Category | Specific Symptoms |
Gastrointestinal | Abdominal cramps, diarrhea, nausea, bloating |
Vasomotor and Cardiovascular | Flushing, dizziness, rapid heart rate, sweating |
Hypoglycemic Episodes | Shakiness, confusion, dizziness, hunger |
To manage these symptoms, you need a plan. This plan should include changing your diet, making lifestyle changes, and possibly getting medical help.
Risk Factors for Developing Post-Gallbladder Dumping Syndrome
Knowing the risk factors for post-gallbladder dumping syndrome can help manage and prevent it. Health conditions, surgery techniques, and lifestyle choices all play a role. These factors can increase the chance of getting dumping syndrome.
Pre-existing Digestive Conditions
People with digestive problems are more likely to get dumping syndrome after their gallbladder is removed. Conditions like gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS) can make digestion harder. This makes it easier for dumping syndrome to occur.
These conditions change how the body digests food. Without a gallbladder, it’s harder for the body to adjust. So, people with these conditions might face worse symptoms or a higher risk of dumping syndrome.
Surgical Technique Considerations
The way a surgeon removes the gallbladder can affect the risk of dumping syndrome. For example, how much of the surrounding area is touched during surgery matters. This can impact how well the digestive system works after surgery.
Surgeons use different methods, like laparoscopic or open cholecystectomy. Each method has its own effects on recovery and risk of problems. Knowing these differences helps understand individual risks.
Dietary and Lifestyle Risk Factors
What you eat and how you live can also raise the risk of dumping syndrome. Eating high-sugar foods and large meals can make symptoms worse. Not eating a balanced diet also plays a part.
Other lifestyle factors, like eating habits and physical activity levels, can also affect the risk. Making smart choices about diet and lifestyle can lower this risk.
Healthcare providers can teach patients about these risks. This helps people take steps to avoid dumping syndrome after gallbladder removal.
Diagnostic Approaches for Dumping Syndrome
To find out if someone has dumping syndrome, doctors use a few methods. They look at how the body acts and do special tests. This way, they can figure out what’s wrong and how to fix it.
Clinical Evaluation and Symptom Assessment
First, doctors check the patient’s history and symptoms. They look at when these symptoms happen after eating. This helps them tell if it’s dumping syndrome or something else.
They pay close attention to symptoms like:
- Abdominal cramps and pain
- Nausea and vomiting
- Diarrhea
- Dizziness and flushing
- Rapid heartbeat
Laboratory and Imaging Studies
Doctors also do tests to rule out other problems. These tests check for things like anemia or other health issues. They might include:
- Blood tests to check for anemia, electrolyte imbalance, or other metabolic changes
- Imaging studies such as a CT scan or MRI to evaluate the stomach and intestines
- Gastrointestinal endoscopy to examine the upper digestive tract
Even though these tests aren’t surefire, they help rule out other conditions.
Specialized Tests for Confirming Diagnosis
To be sure, doctors might use tests like the oral glucose tolerance test (OGTT) or a mixed meal test. These tests involve eating a certain meal or drink and then checking symptoms and blood sugar levels over time.
Key diagnostic tests include:
- Oral glucose tolerance test (OGTT)
- Mixed meal test
These tests help doctors confirm the diagnosis by seeing how the body reacts to food.
By using a mix of clinical checks, symptom assessments, and special tests, doctors can accurately diagnose dumping syndrome. Getting medical advice is key for the right diagnosis and treatment.
Bile Acid Diarrhea: A Related Condition
Bile acid diarrhea is a complication that can happen after gallbladder removal. It’s important to understand it well for proper treatment. This condition is linked to the body not absorbing bile acids properly after the gallbladder is gone.
Mechanism and Relationship to Gallbladder Removal
The gallbladder helps store and concentrate bile acids. These acids are key for digesting fats. Without the gallbladder, too much bile acid can flow into the intestine, causing diarrhea. This is known as bile acid diarrhea or bile salt diarrhea.
We will look into how not having a gallbladder affects bile acid flow. This is important for understanding bile acid diarrhea after gallbladder surgery.
Distinguishing from Dumping Syndrome
Dumping syndrome and bile acid diarrhea can both happen after gallbladder surgery. But they have different causes and symptoms. Dumping syndrome is about food moving too fast into the small intestine, causing stomach and intestine problems.
Bile acid diarrhea, on the other hand, is about not absorbing bile acids well. It’s important to tell these two conditions apart for the right treatment. We will talk about the main differences in symptoms and how to diagnose them.
Specific Management Approaches
There are several ways to manage bile acid diarrhea. These include changing what you eat, taking medicine, and making lifestyle changes. We will look at using bile acid sequestrants, like cholestyramine, to help.
Changing your diet, like eating less fat and avoiding certain foods, can also help. We will also discuss other treatments and lifestyle changes to improve life for those with bile acid diarrhea.
Dietary Strategies to Manage Dumping Syndrome
To manage dumping syndrome, certain dietary strategies are key. This condition happens after gallbladder removal. It causes food to move too fast into the small intestine, leading to uncomfortable symptoms. Changing your diet can help ease these symptoms and improve your life.
Foods That Trigger Symptoms
Knowing and avoiding foods that trigger dumping syndrome is important. Common culprits include:
- Sugary foods and drinks: High sugar can make symptoms worse.
- Dairy products: Dairy can trigger or worsen symptoms for some.
- High-fat foods: While fatty foods slow digestion, they can also trigger symptoms.
- Caffeine and carbonated beverages: These can irritate the stomach and worsen symptoms.
Beneficial Dietary Choices and Patterns
Eating a diet rich in nutrients and easy to digest can help manage dumping syndrome. Good choices include:
- Lean proteins: Chicken, fish, and tofu are good options.
- Complex carbohydrates: Whole grains, fruits, and vegetables are recommended.
- Low-fat dairy or dairy alternatives: Low-fat or non-dairy options are beneficial.
Eating smaller, more frequent meals can also help manage symptoms. This reduces the load on the digestive system.
Meal Timing, Frequency, and Portion Control
Adjusting meal timing and frequency is key to managing dumping syndrome. Recommendations include:
- Eating smaller, more frequent meals throughout the day.
- Avoiding eating before bedtime to reduce nighttime symptoms.
- Practicing portion control to prevent overloading the digestive system.
Hydration Guidelines and Considerations
Drinking enough water is essential for health and managing dumping syndrome symptoms. Recommendations include:
- Drinking fluids between meals to avoid rapid gastric emptying.
- Avoiding beverages high in sugar and caffeine.
- Monitoring hydration levels by observing urine output and color.
By following these dietary strategies, individuals with dumping syndrome can alleviate symptoms and improve their quality of life.
Medical Treatment Options and Interventions
Managing dumping syndrome after cholecystectomy often requires a mix of medications, lifestyle changes, and other treatments. We’ll look at the medical options for managing dumping syndrome. These aim to control symptoms and enhance life quality for those affected.
Medications for Symptom Control
Several drugs can help manage dumping syndrome symptoms. Octreotide is a synthetic analogue of somatostatin. It slows down stomach emptying and reduces symptoms. It’s good for both early and late dumping syndrome.
Other drugs, like acarbose, help control blood sugar. This can lessen symptoms of late dumping syndrome.
Nutritional Supplements and Support
Nutritional supplements are key in managing dumping syndrome, when diet changes aren’t enough. Vitamin and mineral supplements help fix malabsorption-related deficiencies. For severe malnutrition or when oral feeding is hard, enteral nutrition or parenteral nutrition might be needed.
Advanced Interventions for Severe Cases
For severe dumping syndrome that doesn’t respond to basic treatments, more advanced options are considered. Gastric electrical stimulation involves a device that helps regulate stomach movement. For some, surgical revision of previous surgeries might help.
Knowing the medical options and interventions helps those with dumping syndrome. They can work with healthcare providers to create a plan. This plan aims to improve symptoms and life quality.
Lifestyle Modifications for Improved Quality of Life
Making lifestyle changes is key to managing dumping syndrome and feeling better. By making simple changes, people can lessen their symptoms and live a better life.
Physical Activity Recommendations
Being active is important for health and can help with dumping syndrome. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Good choices include brisk walking, cycling, or swimming.
Adding strength training to your routine is also good. Building muscle mass can improve metabolic health. But, always talk to a doctor before starting any new workout.
Stress Management Techniques
Stress can make dumping syndrome symptoms worse. So, finding ways to manage stress is important. Mindfulness practices, like meditation and deep breathing, can lower stress. Yoga and tai chi are also great, mixing physical activity with stress relief.
- Meditation and mindfulness practices
- Deep breathing exercises
- Yoga and tai chi
- Progressive muscle relaxation
Finding a stress management method that works for you can greatly help with dumping syndrome symptoms.
Sleep Optimization Strategies
Getting enough sleep is vital for health and managing dumping syndrome. Keep a regular sleep schedule and make your bedroom sleep-friendly. Try to avoid caffeine and screens before bed.
Aim for 7-9 hours of sleep each night. If you can’t sleep well, see a doctor for help.
When to Seek Medical Advice for Dumping Syndrome
Getting medical advice on time is key to managing dumping syndrome. Knowing when to act fast is vital. It helps avoid serious problems and improves your life quality.
Warning Signs Requiring Immediate Attention
Some symptoms need quick medical help. These include:
- Severe abdominal pain that doesn’t subside
- Vomiting blood or experiencing bloody stools
- Dizziness or fainting spells
- Rapid or irregular heartbeat
- Severe diarrhea or constipation
If you see any of these signs, get medical help fast. Quick action can stop things from getting worse and help you feel better.
Preparing for Your Doctor’s Appointment
Being ready for your doctor’s visit is important. It helps you get the best care. Here’s how to prepare:
- Keep a symptom journal to track when your symptoms occur and their severity
- List all medications and supplements you’re currently taking
- Note any questions or concerns you have about your condition
- Bring a friend or family member for support if needed
Having this info ready can make your talk with your doctor more helpful.
Questions to Ask Your Healthcare Provider
Asking the right questions is important. It helps you understand your condition and treatment options. Consider asking:
- What are the underlying causes of my dumping syndrome?
- What dietary changes can I make to manage my symptoms?
- Are there any medications that can help alleviate my symptoms?
- What lifestyle modifications can I make to improve my quality of life?
Being informed and proactive helps you and your doctor create a good plan. This way, you can manage your symptoms better.
Long-term Management and Prognosis
Managing dumping syndrome long-term is key to better living for those who’ve had their gallbladder removed. It involves changing diets, making lifestyle changes, and sometimes medical treatments.
Timeline for Symptom Improvement
Symptoms of dumping syndrome can get better with the right care. People often see improvements in a few months after making diet and lifestyle changes. But, how long it takes can really vary.
Key factors influencing symptom improvement include:
- Adherence to dietary recommendations
- Effectiveness of lifestyle modifications
- Presence of any underlying conditions
Potential Complications if Left Untreated
Not treating dumping syndrome can cause serious problems. These include malnutrition, dehydration, and imbalances in electrolytes. Also, the emotional side effects should not be ignored. They can lead to anxiety, depression, and a lower quality of life.
The emotional impact of dumping syndrome can be huge, affecting not just the patient but also their family and caregivers. It’s important to tackle both the physical and emotional sides of the condition for full care.
Monitoring and Follow-up Care
Regular check-ups and follow-up care are essential for long-term management. Healthcare providers need to keep an eye on symptoms, adjust treatments as needed, and quickly handle any issues or concerns.
Aspect of Care | Frequency | Purpose |
Symptom Monitoring | Every 3-6 months | To adjust treatment plans and address concerns |
Dietary Counseling | As needed | To ensure adherence to recommended dietary changes |
Emotional Support | Ongoing | To address the emotional impact and provide resources |
In conclusion, managing dumping syndrome long-term needs a mix of diet changes, lifestyle tweaks, and regular check-ups. Knowing how symptoms can improve, the risks of not treating it, and the need for ongoing care helps patients manage their condition better. This way, they can improve their life quality.
Conclusion
We’ve looked into dumping syndrome after gallbladder removal. This condition can really affect a person’s life. It’s important to know what causes it, its symptoms, and how to manage it.
Support resources are key in helping patients deal with dumping syndrome. They offer dietary advice, medical treatments, and tips for changing your lifestyle. This helps patients manage their condition better.
Patients with dumping syndrome can find more help and support. They can talk to doctors who know about stomach problems, join online groups, and read educational materials from trusted sources.
Using these resources, patients can face the challenges of dumping syndrome head-on. This way, they can improve their health and well-being.
FAQ
What is dumping syndrome, and how is it related to gallbladder removal?
Dumping syndrome, or rapid gastric emptying, happens when food moves too fast from the stomach to the small bowel. It’s often linked to stomach or esophagus surgery. But, it can also happen after gallbladder removal because of digestion changes.
What are the symptoms of dumping syndrome?
Symptoms include diarrhea, stomach cramps, and bloating. You might also feel flushing, heart racing, and dizzy. Late dumping syndrome can cause low blood sugar.
How is dumping syndrome diagnosed?
To diagnose, doctors will check your symptoms and do tests. They might use lab and imaging studies to rule out other conditions. Special tests can confirm the diagnosis.
What dietary changes can help manage dumping syndrome?
Start by avoiding foods that trigger symptoms. Choose foods that are good for you and eat them at the right times. Drinking enough water is also important.
Are there any medical treatments available for dumping syndrome?
Yes, there are medicines to help manage symptoms. Nutritional supplements can also offer support. For severe cases, there are more advanced treatments.
How can lifestyle modifications improve the quality of life for patients with dumping syndrome?
Being active, managing stress, and getting enough sleep can help. These changes can reduce symptoms and improve your overall health.
What are the risk factors for developing dumping syndrome after gallbladder removal?
Conditions like pre-existing digestive issues, certain surgeries, and lifestyle choices can increase your risk. These factors can lead to dumping syndrome.
How does bile acid diarrhea relate to gallbladder removal, and how is it managed?
Bile acid diarrhea can happen after gallbladder removal due to bile changes. Managing it involves specific diets and sometimes medication to control symptoms.
When should I seek medical help for dumping syndrome?
If symptoms are severe or don’t go away, seek medical help. Look out for signs like severe pain, vomiting, or dehydration.
What is the long-term outlook for managing dumping syndrome?
With the right management, symptoms can get better over time. This includes dietary changes, lifestyle adjustments, and sometimes medication. Regular check-ups are key to avoiding complications.
Can dumping syndrome be prevented after gallbladder removal?
While prevention isn’t always possible, being aware of risk factors helps. Making the right dietary and lifestyle choices can lower your chances of getting dumping syndrome.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41575-020-0280-4