If you’re thinking about surgery for severe obesity, knowing the risks is key. The duodenal switch procedure can lead to big weight loss and health gains. But, it also comes with specific dangers like nutritional problems and digestive issues.Recognizing and managing the common duodenal switch complications (e.g., Malnutrition).
At Liv Hospital, we stress the need for full patient education. We know that about 15.3% of patients face early surgery complications. So, it’s vital to understand the possible issues and think carefully about the pros and cons.
Key Takeaways
- Duodenal switch surgery is a complex procedure with significant weight loss benefits.
- Early complications occur in approximately 15.3% of patients.
- Potential risks include nutritional deficiencies and digestive complications.
- Comprehensive patient education is key for making informed choices.
- Knowing the risks and benefits is essential for those considering this surgery.
What is the Duodenal Switch Procedure?
The duodenal switch, also known as biliopancreatic diversion with duodenal switch, is a complex bariatric surgery. It aims to help people lose a lot of weight by changing their digestive system.
Definition and Purpose of Biliopancreatic Diversion with Duodenal Switch
Biliopancreatic diversion with duodenal switch (BPD/DS) is a surgery that combines two main parts. It makes the stomach smaller and changes how food moves through the intestines. This limits how much nutrients the body can absorb.
“The duodenal switch surgery is a powerful tool in the fight against obesity,” says Dr. [Last Name], a renowned bariatric surgeon. “By reducing the stomach size and rerouting the intestines, we can help patients achieve substantial weight loss and improve their overall health.”
Combined Restrictive and Malabsorptive Approach
The duodenal switch procedure has two main parts. The first part limits how much food you can eat by making your stomach smaller. The second part reduces nutrient absorption by changing the small intestine’s path.
This approach helps with weight loss and reduces risks from other surgeries.
Historical Development and Current Practice
The duodenal switch procedure has changed a lot over time. It started with the biliopancreatic diversion in the 1970s. Now, it’s a very effective surgery for weight loss and improving health.
It’s important for patients to know the risks and complications of the duodenal switch. Understanding the procedure helps people make better choices about their treatment.
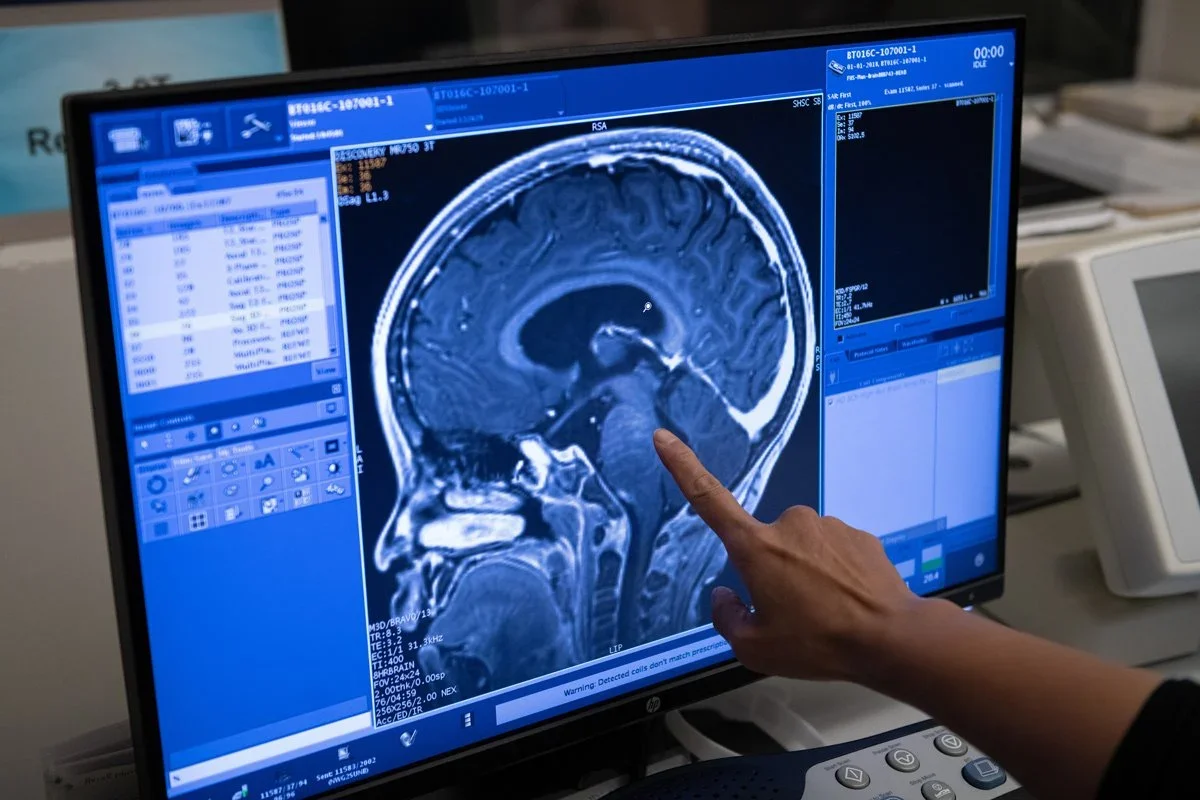
The Surgical Technique and Anatomical Changes
[Add image here]
Knowing how the duodenal switch surgery works is key for those thinking about it. This surgery makes big changes to the stomach and intestines. It aims to help people lose a lot of weight and improve their health.
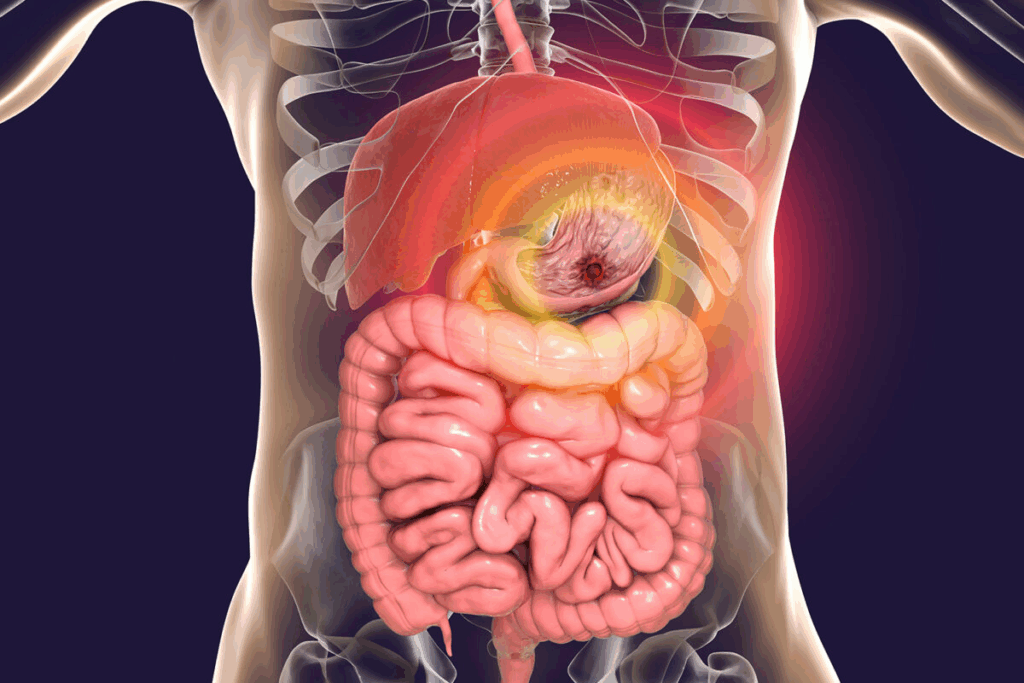
Partial Gastrectomy Along the Greater Curvature
The first part of the duodenal switch is removing a big part of the stomach. This is done along the greater curvature. It shrinks the stomach, which means less room for food and helps with weight loss. The stomach that’s left is made into a tube, much smaller than before.
Duodenal Transection 3-4 cm Distal to the Pylorus
After the stomach part is removed, the duodenum is cut about 3-4 cm from the pylorus. This is important because it keeps the pyloric valve working. The valve helps control how food moves into the small intestine. Cutting here is very precise to avoid problems.
Creation of 250 cm Alimentary Limb and Biliary Anastomosis
Next, a 250 cm alimentary limb is made. This is the part of the intestine that food will go through. Then, a biliary anastomosis is done, linking the biliary limb to the alimentary limb. This changes how food is digested, helping to lose weight by not absorbing as many calories and fats.
Surgical Step | Description | Outcome |
Partial Gastrectomy | Removal of a significant portion of the stomach along the greater curvature | Reduced stomach size, limited food intake |
Duodenal Transection | Transection of the duodenum 3-4 cm distal to the pylorus | Preservation of the pyloric valve, regulated food passage |
Creation of Alimentary Limb and Biliary Anastomosis | Creation of a 250 cm alimentary limb and connection of biliary and alimentary limbs | Reconfiguration of the digestive pathway, malabsorption of calories and fats |
The duodenal switch is a detailed surgery that needs a skilled surgeon. It changes the body’s anatomy in big ways. Understanding these changes helps patients see the surgery’s benefits and risks.
Benefits and Expected Outcomes of Duodenal Switch
The duodenal switch procedure is known for its success in weight loss and health improvement. It’s a complex surgery that many patients and doctors recommend. It has many benefits that make it popular.
Superior Weight Loss
The duodenal switch helps people lose a lot of weight. Studies show that it can lead to losing 70-80% of excess weight. This is more than other surgeries.
Bariatric Procedure | Average Excess Weight Loss (%) |
Duodenal Switch | 75-85% |
Roux-en-Y Gastric Bypass | 60-70% |
Sleeve Gastrectomy | 50-60% |
Resolution of Obesity-Related Comorbidities
The duodenal switch also helps with health problems linked to obesity. Conditions like type 2 diabetes, high blood pressure, and sleep apnea often get better or go away after surgery.
Long-term Quality of Life Improvements
People who have the duodenal switch surgery often feel better in the long run. They lose a lot of weight and their health problems get better. This leads to better physical and mental health and a happier life.
In summary, the duodenal switch offers many benefits. It helps with weight loss, health problems, and improves life quality. It’s a big decision, so patients should think carefully and talk to their doctor.
Understanding Duodenal Switch Complications: Incidence and Risk Factors
The duodenal switch procedure helps with weight loss but has its own set of complications. It’s important to know about these issues and the factors that make them more likely.
Early Complications
About 15.3% of patients face early complications after the surgery. These can include infections, bleeding, and breathing problems. Knowing these risks helps both patients and doctors prepare better.
Late Complications and Their Prevalence
Late complications happen after the first recovery period. They can include malnutrition and malabsorption. These problems come from how the surgery changes digestion.
Malnutrition and malabsorption can lead to vitamin and mineral deficiencies. Here’s a table showing some late complications and how common they are:
Complication | Prevalence |
Malnutrition | 20-30% |
Malabsorption | 15-25% |
Vitamin Deficiencies | 10-20% |
Patient-Specific Risk Factors
Some factors can make complications more likely after the surgery. These include health conditions like diabetes or heart disease. Lifestyle choices, like smoking, also play a role.
By understanding these risks, doctors can give better advice and plan to reduce them. This helps improve how well patients do after the surgery.
Critical Complication #1: Severe Malnutrition and Malabsorption
The Duodenal Switch can lead to severe malnutrition and malabsorption. This procedure changes how we digest food, which can cause nutritional problems.
Protein Deficiency and Hypoalbuminemia
Protein deficiency is common after a Duodenal Switch. The smaller stomach and changed intestines make it hard to absorb enough protein. This can cause low albumin levels in the blood. Monitoring protein intake and absorption is key to avoid this.
To fight protein deficiency, eating high-protein foods and taking supplements is advised. Regular blood tests help keep albumin levels in check and guide diet changes.
Fat-Soluble Vitamin Deficiencies (A, D, E, K)
The Duodenal Switch can also cause a lack of fat-soluble vitamins like A, D, E, and K. These vitamins are important for vision, bone health, and more. Without them, health problems can arise.
Patients need to take vitamins for life and have their levels checked often. A good follow-up plan is vital to catch and fix any vitamin shortages early.
Mineral Deficiencies (Iron, Calcium, Zinc)
Mineral deficiencies, such as iron, calcium, and zinc, are also risks. Iron deficiency can cause anemia, while calcium issues can lead to weak bones. Zinc problems can slow down healing and weaken the immune system.
Mineral | Deficiency Symptoms | Management Strategies |
Iron | Anemia, fatigue, weakness | Iron supplements, dietary adjustments |
Calcium | Osteoporosis, bone pain | Calcium supplements, vitamin D supplementation |
Zinc | Impaired wound healing, immune dysfunction | Zinc supplements, dietary adjustments |
A study on bariatric surgery highlights the need for lifelong nutritional support. “Lifelong nutritional supplementation and monitoring are critical to prevent deficiencies and related complications.”
“The importance of a multidisciplinary approach to managing nutritional deficiencies after Duodenal Switch cannot be overstated. It requires a coordinated effort from healthcare providers, nutritionists, and patients to ensure optimal outcomes.”
Understanding the risks of malnutrition and malabsorption helps healthcare providers support patients better. They can ensure patients get the right nutrition and care to avoid these problems.
Critical Complication #2: Gastrointestinal Disturbances
The duodenal switch procedure helps with weight loss but can cause stomach problems. These issues can really affect a person’s life quality. They might need constant medical care to manage them.
Chronic Diarrhea and Steatorrhea
After duodenal switch surgery, many people deal with chronic diarrhea and steatorrhea. Diarrhea can cause dehydration and imbalances in electrolytes if not managed right. Steatorrhea, or too much fat in the stool, can make people uncomfortable and lead to nutritional problems. It’s important for patients to stick to a strict dietary regimen to lessen these symptoms.
To manage these issues, patients should eat less fat and more fiber. Sometimes, doctors might prescribe medicine to control diarrhea and improve nutrient absorption.
Dumping Syndrome and Hypoglycemia
Dumping syndrome happens when food moves too fast through the stomach after duodenal switch surgery. It causes nausea, vomiting, stomach pain, and diarrhea. Dumping syndrome is often triggered by eating too much sugar or fat. Hypoglycemia, or low blood sugar, can also happen because of changes in the digestive system.
To deal with dumping syndrome, patients should eat smaller meals more often and avoid foods that trigger it. Keeping an eye on blood sugar levels and adjusting diet can help avoid hypoglycemia.
Small Intestinal Bacterial Overgrowth (SIBO)
Small intestinal bacterial overgrowth (SIBO) is another issue after duodenal switch surgery. It happens when bacteria grow too much in the small intestine, causing bloating, stomach pain, and poor nutrient absorption. Diagnosis usually involves breath tests or aspiration and culture.
Treatment for SIBO includes antibiotics and changes in diet. Doctors might also suggest probiotics to help the gut microbiome. It’s important to keep an eye on it to prevent it from coming back and to manage symptoms well.
Critical Complication #3: Surgical Complications of Duodenal Switch
Duodenal switch procedures come with serious surgical complications. These issues can greatly affect a patient’s recovery and surgery results.
Anastomotic Leaks and Strictures
Anastomotic leaks are a major concern. They happen when the intestine doesn’t connect properly, causing contents to leak into the belly. This can lead to severe infections and even be life-threatening. Prompt diagnosis and treatment are key to handling these leaks well.
Another issue is anastomotic strictures. This is when the connection between parts of the intestine narrows, causing blockages. Symptoms include pain, nausea, and vomiting. Treatment might involve widening the area with a scope or surgery.
Bowel Obstruction and Ileus
Bowel obstruction is a big risk after duodenal switch surgery. It happens when the intestine’s flow is blocked, either mechanically or due to ileus. Symptoms include severe pain, vomiting, and constipation. Early action is essential to avoid serious problems like bowel ischemia.
Complication | Symptoms | Treatment |
Anastomotic Leak | Severe abdominal pain, fever, infection | Surgical repair, antibiotics |
Bowel Obstruction | Abdominal pain, vomiting, constipation | Surgical intervention, bowel rest |
Internal Hernia | Abdominal pain, vomiting, bowel ischemia | Surgical repair |
Internal Hernias and Volvulus
Internal hernias happen when intestine bulges through a hole in the belly, causing blockages or ischemia. Volvulus, where a part of the intestine twists, can also cause these issues. Both need quick surgery to avoid serious problems.
It’s important for both patients and doctors to know about these complications. Recognizing risks and symptoms early can help improve surgery outcomes for duodenal switch patients.
Critical Complication #4: Metabolic and Systemic Disorders
After duodenal switch surgery, patients may face metabolic and systemic disorders. These issues can greatly affect their quality of life. They need careful management to handle these problems.
Bone Demineralization and Osteoporosis
Bone demineralization and osteoporosis are big worries after duodenal switch surgery. The surgery can make it hard for the body to absorb calcium and vitamin D. This can lower bone density, raising the risk of osteoporosis and fractures.
Patients should get regular bone density scans. They also need to follow a calcium and vitamin D supplement plan.
Nephrolithiasis (Kidney Stones)
Kidney stones are another possible issue. The surgery can change how the body makes urine, raising the risk of stones. Drinking plenty of water and making dietary changes can help prevent this problem.
Hepatic Dysfunction and Liver Failure
Hepatic dysfunction and liver failure are rare but serious. The surgery can lead to malabsorption of nutrients and protein deficiency. This can harm liver function.
It’s key to keep an eye on liver function and nutrition. This can help avoid liver problems.
We stress the need for thorough checks before and after surgery. This helps reduce the risk of metabolic and systemic disorders. By knowing these risks, patients and doctors can work together for the best results after duodenal switch surgery.
Critical Complication #5: Psychological and Behavioral Impact
Choosing to have a duodenal switch surgery is a big decision. It changes your body and mind. Patients face many challenges as they lose weight and change their lifestyle.
Body Image Disturbances After Massive Weight Loss
After a duodenal switch, your body looks different. Some people feel better about themselves, but others struggle with loose skin and body shape changes. They might need more surgeries to fix these problems.
It’s hard to get used to these changes. Some patients find help in counseling or support groups to deal with body image issues.
Disordered Eating Patterns and Food Aversions
Patients after a duodenal switch must follow a strict diet. This can cause disordered eating patterns or make them dislike certain foods.
Working with a healthcare team, including a dietitian, is key. They help create a diet plan that’s right for you. This plan should help you eat healthily and feel good about food.
Depression, Anxiety, and Adjustment Disorders
The big changes after a duodenal switch can affect your mental health. You might feel depressed or anxious. It’s hard to adjust to your new life.
Psychological Challenge | Potential Solutions |
Body Image Disturbances | Counseling, Support Groups, Body Contouring Surgery |
Disordered Eating Patterns | Personalized Eating Plans, Nutritional Counseling |
Depression and Anxiety | Mental Health Support, Therapy, Medication |
We stress the need for full care, including mental health support. This helps patients overcome these challenges and succeed.
Preventing and Managing Duodenal Switch Complications
To prevent and manage duodenal switch complications, we need a detailed plan. A good strategy is key to keeping risks low and outcomes high.
We focus on three main areas. These are: a thorough check before surgery, regular follow-ups after, and a lifelong diet plan. Each part is important for avoiding and handling problems.
Comprehensive Preoperative Evaluation and Preparation
Before surgery, we do a deep check to find risks. We look at medical history, nutrition, and mental health. This helps us get each patient ready for the surgery’s challenges.
Key parts of this check include:
- Nutritional advice to prepare for diet changes after surgery
- Psychological tests to spot mental health issues
- Reviewing medical history for risk factors
Structured Postoperative Follow-up Schedule
After surgery, regular visits are key. They help us watch how the patient is doing and fix problems fast. This way, we can keep track of nutrition and make changes if needed.
As a top bariatric surgeon says,
“Regular check-ups are vital for duodenal switch success. They let us solve problems quickly and adjust plans as needed.”
Lifelong Nutritional Regimen and Monitoring
After duodenal switch surgery, a special diet is needed forever. This includes a balanced diet, vitamins, and checking nutrition levels. Working with dietitians helps patients stay on track and avoid shortages.
Key parts of this diet include:
- A diet rich in protein, vitamins, and minerals
- Vitamins to prevent shortages
- Regular blood tests to check nutrition
By using a detailed plan for preventing and managing duodenal switch problems, we can greatly improve patient results and life quality.
Bariatric Revision Surgery: When and Why It’s Needed
When duodenal switch surgery doesn’t work as planned, bariatric revision surgery is a good option. This surgery is for those who face complications or don’t lose enough weight. It’s a way to fix problems and help with weight loss.
Indications for Surgical Revision
Revision surgery is needed for several reasons. These include severe malnutrition, ongoing stomach problems, or not losing enough weight. We carefully check each patient to see if they need this surgery.
- Severe malnutrition or malabsorption
- Persistent gastrointestinal disturbances
- Inadequate weight loss or weight regain
- Complications such as anastomotic leaks or strictures
Common Revision Procedures and Techniques
Revision surgery can take many forms, depending on the patient’s needs. We look at the patient’s health, why they need surgery, and the best techniques to use.
Revision Procedure | Description | Potential Benefits |
Revision of Anastomosis | Correcting or revising the anastomotic connection | Improved nutrient absorption, reduced complications |
Limb Length Adjustment | Adjusting the length of the alimentary or common limb | Enhanced weight loss, improved metabolic outcomes |
Gastric Pouch Revision | Revising the gastric pouch to improve restriction | Better weight management, reduced reflux |
Outcomes and Expectations
The results of bariatric revision surgery can differ. We talk about the good and bad with our patients. This helps them make informed choices.
Good outcomes include better weight loss, solving problems, and a better life. But, it’s important to know that surgery comes with risks. We want our patients to have realistic hopes and understand the challenges.
Conclusion: Making Informed Decisions About Duodenal Switch Surgery
Exploring duodenal switch surgery shows it’s key to make smart choices. Knowing the good and bad sides helps face its challenges and chances. This is vital for those thinking about it.
It’s important to know the risks, like severe malnutrition and metabolic issues. But, there are also benefits like losing a lot of weight and better health. These are things to think about.
Patients should talk a lot with their doctors before deciding. This helps them understand if it’s right for them. It prepares them for what comes next, aiming for the best results.
Following up after surgery and sticking to a diet for life is also key. This helps avoid problems and keeps success going. Knowing all about duodenal switch surgery helps patients make choices that improve their health and life quality.
FAQ
What is the duodenal switch procedure?
The duodenal switch procedure is a complex surgery for weight loss. It combines two methods: making the stomach smaller and changing how the body absorbs nutrients. This helps patients lose a lot of weight and improve health problems linked to being overweight.
What are the benefits of the duodenal switch procedure?
This surgery leads to better weight loss than other methods. It also helps solve health issues related to being overweight. Plus, it improves quality of life in the long run.
What are the possible complications of the duodenal switch procedure?
Possible complications include severe malnutrition and trouble absorbing nutrients. Other issues are stomach problems, surgery side effects, and health problems. It can also affect mental health and behavior.
How can severe malnutrition and malabsorption be managed after duodenal switch surgery?
Managing these issues involves lifelong monitoring of nutrition. Patients need to adjust their diet and take supplements. This includes protein, vitamins, and minerals that are fat-soluble.
What are the indications for bariatric revision surgery after duodenal switch?
Revision surgery is needed if weight loss is not enough or if weight comes back. It’s also for complications like bowel blockages or hernias. Or if there are problems with nutrients.
What are the common revision procedures after duodenal switch?
Common revisions include changing the stomach part that connects to the small intestine. Adjusting the bile connection and fixing any other issues are also done. These help with weight loss and solve problems.
How can patients prevent and manage duodenal switch complications?
Preventing and managing complications involves careful planning before surgery. Follow-up care is key. Also, lifelong monitoring of nutrition is essential.
What is the importance of lifelong nutritional monitoring after duodenal switch surgery?
Monitoring nutrition for life is vital. It helps catch and manage nutrient deficiencies. This includes protein, vitamins, and minerals that are fat-soluble.
Can duodenal switch surgery lead to psychological and behavioral changes?
Yes, the surgery can cause changes in how you feel about your body and eat. It can also lead to depression. Ongoing support is needed to manage these changes.
References
National Center for Biotechnology Information. Duodenal Switch: Key Complications and Risks. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10771970/