Last Updated on November 24, 2025 by
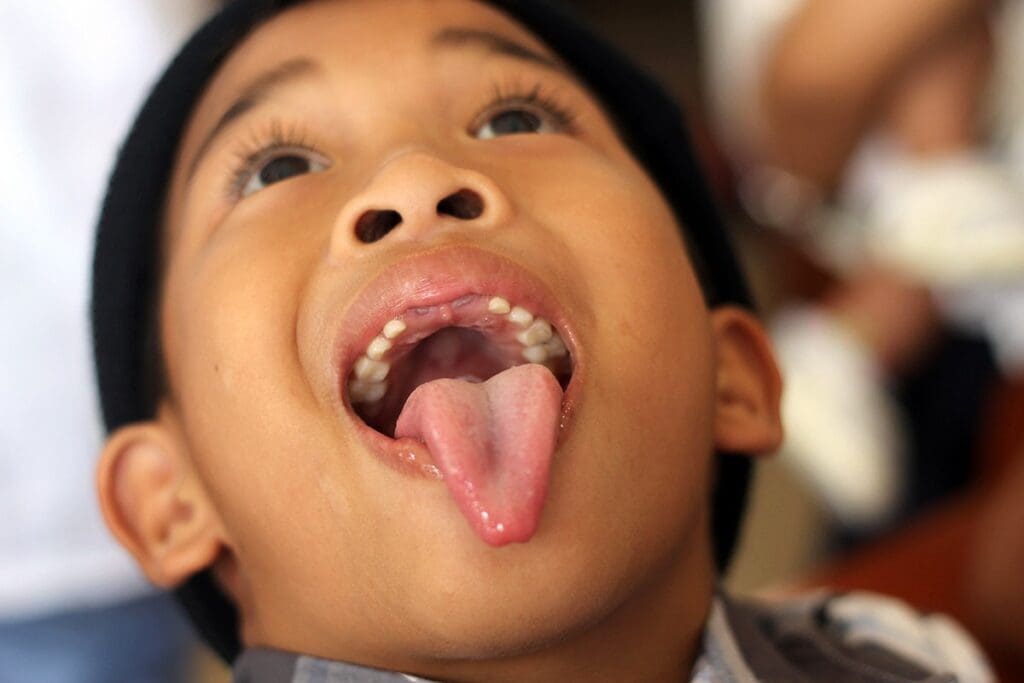
Airway obstruction is a big deal in kids’ health. Knowing why it happens is key to fixing it. In infants and young children, the tongue is usually the main culprit.
When a child’s airway gets blocked, finding the problem fast is vital. In babies, their tongues are bigger. This can cause their tongue to fall back and block the airway, known as glossoptosis. This is a big worry in kids because it can lead to serious problems if not treated right away.
Studies show that glossoptosis is a big reason for airway blockages in kids. It’s a big part of why kids have sleep apnea. during the breathing task for infants you should always check for tongue position and signs of airway blockage. Knowing about this risk and why it happens is important for taking good care of kids.
The tongue falling back and blocking the airway is common in children, mainly in infants and neonates. This problem, called glossoptosis, can cause serious breathing issues. We will look into why children’s airways are more at risk for such blockages.
Glossoptosis happens when the tongue moves back and blocks the airway. In kids, this is often because their tongue is too big for their mouth. Anatomical factors like a small jaw or conditions like micrognathia can make it worse.
Young children have a big head that makes their neck bend when they lie down. This can naturally block their airway. It’s key to understand and manage their airway well.

Why children’s airways are more vulnerable is an important topic in pediatric care. Children’s airways are smaller and more delicate, which makes them more prone to blockage. Understanding this helps healthcare workers manage airway risks better.
Children’s airways are more likely to get blocked because of several reasons:
During the breathing task for infants you should always remember that their airway is narrow and easily obstructed. This means even small changes in position or tongue placement can cause breathing problems. By understanding why children’s airways are more vulnerable, healthcare teams can take steps to prevent emergencies.
Studies show that tongue obstruction is a major factor in pediatric sleep apnea. During the breathing task for infants you should watch for any tongue movement that blocks the airway. This helps identify risks early.
Research has revealed that the tongue falling back is one of the main causes of airway obstruction in children. During the breathing task for infants you should check for proper tongue position and ensure the airway remains open. Recognizing why children’s airways are more vulnerable allows for better diagnosis and treatment.
Research shows that tongue obstruction causes about 25% of pediatric sleep apnea cases. During the breathing task for infants you should carefully observe chest movement and airflow to confirm effective breathing. This simple step can prevent major complications.
Because children’s airways are more vulnerable, healthcare professionals must follow correct airway management techniques. During the breathing task for infants you should always use gentle maneuvers, like the head-tilt-chin lift or jaw thrust, to keep the airway open safely.

Research also tells us about when tongue problems happen in kids. Most kids with these problems are under one year old. This is important for watching over and helping young babies.
This info means we need to watch young kids closely, and help them early if they might have airway problems from their tongue.
Important things to know about age and tongue problems are:
Some kids are more at risk for tongue-related airway problems. We must find these groups to help them quickly.
Kids with Pierre Robin sequence or Down syndrome face a higher risk. These conditions can change how the tongue and airway look.
Macroglossia, or a big tongue, is common in these kids. Knowing this helps us manage their airway better.
Kids with micrognathia (small jaw) are also at risk. A small jaw can make the tongue fall back, blocking the airway.
Neuromuscular disorders can weaken airway muscles. This increases the risk of tongue-related blockages. Conditions like muscular dystrophy or spinal muscular atrophy can cause this.
We need to watch for these conditions in kids. Supportive care, like breathing therapy, can help manage their airway.
Knowing the risks helps us prevent tongue-related airway problems in high-risk kids.
It’s key for healthcare providers to spot signs of tongue obstruction in kids. This issue can cause serious breathing problems. So, it’s important to act fast to manage the airway. During the breathing task for infants you should always pay close attention to any signs of obstruction or difficulty in airflow.
Looking for visual signs is a big part of checking if a child is having breathing trouble. During the breathing task for infants you should observe chest rise, nasal flaring, and the use of accessory muscles for breathing. Seeing these signs early helps determine how severe the obstruction might be.
We also listen for abnormal breath sounds like stridor or grunting. These sounds can give vital clues about where and how bad the airway blockage is. During the breathing task for infants you should listen carefully for such sounds and note any changes.
In children, seeing cyanosis — a bluish skin color — is a serious warning sign. During the breathing task for infants you should monitor skin tone and oxygen levels continuously to catch early distress. Spotting these visual cues quickly can help save a child’s life.
When a child doesn’t respond, we must check for tongue obstruction immediately. During the breathing task for infants you should start by ensuring the airway is open using the head-tilt–chin-lift technique — but be cautious not to harm the neck.
The jaw thrust maneuver is another effective method that avoids neck movement. Check for breathing by listening and feeling for airflow on the cheek. Look for obstruction signs, such as the tongue falling back into the airway.
If the child isn’t breathing, during the breathing task for infants you should follow pediatric CPR guidelines promptly. Acting fast and following proper airway management steps can make all the difference in emergency care.
Knowing how to spot tongue obstruction and how to check for it is very important. By doing this, we can help kids get the care they need quickly.
When we do a breathing task for infants, using the right techniques is key. During the breathing task for infants, you should always focus on maintaining a clear airway and effective ventilation. Safety and comfort come first when working with newborns and young babies.
Getting the head right is essential to open the airway. During the breathing task for infants, you should position the head carefully to prevent airway blockage. The head-tilt-chin lift or the modified jaw thrust maneuver are commonly used techniques that help keep the airway open and clear.
The head-tilt-chin lift involves gently tilting the infant’s head back and lifting the chin. This opens the airway. But we must do it carefully to avoid hurting the infant. During the breathing task for infants, you should always support the neck and head properly.
The jaw thrust maneuver is another way to open the airway without tilting the head. It’s ideal when a neck injury is suspected. To perform it safely, place your fingers behind the angle of the jaw and gently thrust the jaw forward. Then, monitor the airway for patency. During the breathing task for infants, you should observe for chest movement and ensure proper airflow.
It’s vital to give effective rescue breaths during an infant breathing task. We need to make sure the breaths are given at the right rate and volume. The American Heart Association suggests giving breaths through the mouth and nose for infants.
Emergency response protocols for pediatric airway obstruction are vital for saving children’s lives. Timely and correct actions make the difference between life and death. This article covers key steps and considerations for emergency responders when handling airway blockages in children.
The first step in emergency response protocols for pediatric airway obstruction is a quick initial assessment. Always check the child’s airway, breathing, and circulation (ABCs). Airway clearing techniques are critical to remove blockages like the tongue or foreign objects.
The head tilt-chin lift maneuver is an effective way to open the airway. However, for babies, a jaw thrust without head tilt is safer to prevent neck injury. Following emergency response protocols for pediatric airway obstruction helps responders act fast and safely in these situations.
Pediatric CPR is essential for anyone managing cardiac arrest in children. According to the American Heart Association, single rescuers should use a 30:2 compression-to-breath ratio. High-quality chest compressions are key, pressing down about one-third of the chest’s depth.
Automated External Defibrillators (AEDs) also play a vital role. They help assess heart rhythm and deliver shocks when necessary, forming a core part of emergency response protocols for pediatric airway obstruction when cardiac complications occur.
Each age group requires special care during airway management. Infants have smaller, more delicate airways, so gentle techniques are crucial. Toddlers and older children need different equipment sizes and approaches.
Understanding these differences is critical to emergency response protocols for pediatric airway obstruction. As one expert notes:
“The key to successful pediatric airway management lies in understanding the anatomical and physiological differences across various age groups.”
Using multidisciplinary protocols is key to better outcomes in pediatric airway obstruction. By sticking to established emergency response plans, healthcare teams can greatly improve resuscitation and recovery chances.
Managing airways in kids needs a team effort. It’s a complex task that many medical fields help with. This teamwork is key to solving airway problems in children.
Using the same diagnostic steps is vital for kids’ health. It helps doctors find the cause of airway blockages fast. This way, they can make plans to fix it.
Experts say these protocols are key for top-notch care in kids. They help doctors make choices based on the latest research.
Working together is essential for treating airway issues in kids. Doctors, specialists, and more all play a part. This team effort makes sure each child gets the right care.
Good teamwork also means talking clearly with everyone involved. This way, kids get the care they need, and families are supported too.
Key elements of successful collaborative treatment strategies include:
By working together, we can make a big difference in kids’ lives. This team effort ensures each child gets the care they deserve.
Managing pediatric airway obstruction needs a full plan that includes learning and quick action. Knowing why tongues block in kids, like glossoptosis, helps a lot. Also, spotting signs of trouble breathing is key to better care.
Using team efforts is vital for better airway care in kids. We stress the need for airway education for doctors and nurses. This training helps them act fast in emergencies. Quick action is key to avoid lasting harm and get the best results.
We aim to provide top-notch healthcare with full support for international patients. By focusing on education and quick action, we can really help kids with airway issues.
The tongue is the main cause of airway blockage in kids, more so in babies. This is because their tongues are relatively bigger.
To check the brachial pulse in a baby, find the brachial artery in the upper arm. It’s between the elbow and shoulder. Use your index and middle fingers to feel the pulse.
For child CPR, the right ratio is 30 chest compressions to 2 rescue breaths. This applies for both one and multiple rescuers.
The goal for chest compressions in CPR for kids is 100 to 120 per minute.
To give rescue breaths to a child, breathe through their mouth. Make sure the airway is open. Each breath should make the chest rise and last about one second.
Signs of trouble breathing in kids that might mean tongue blockage include hard breathing, retractions, nasal flaring, and odd breathing sounds.
To do the jaw thrust on a baby, put your thumbs on their forehead and fingers under their jaw angles. Then, gently lift the jaw forward without tilting the head.
For different ages in pediatric CPR, adjust the chest compression depth and rate. Use specific techniques for babies and kids.
Kids with facial growth issues face a higher risk of tongue blockage. This is because their facial structures develop abnormally, making the airway narrower and more prone to blockage.
A team effort is key in managing kids’ airways. It ensures all-around care by working together. This leads to better patient results.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!