The endometrial canal is key to female reproductive health. It’s where pregnancy starts and menstruation happens. What is the endometrial canal? This ultimate, simple guide reveals the vital, essential function of this part of the uterus.
Knowing about this part of our body is important. It’s covered in endometrium, a special tissue. This tissue changes a lot during the menstrual cycle. It helps with pregnancy or shedding blood.
At Liv Hospital, we think knowing about the endometrial canal helps women take care of their health.
Key Takeaways
- The endometrial canal is the central cavity within the uterus.
- It is lined by the endometrium, a specialized mucous membrane.
- The endometrial canal plays a critical role in reproduction and menstrual health.
- Understanding its anatomy and physiological changes is essential for appreciating its significance in women’s health.
- The endometrial canal undergoes significant transformations throughout the menstrual cycle.
The Female Reproductive System Architecture
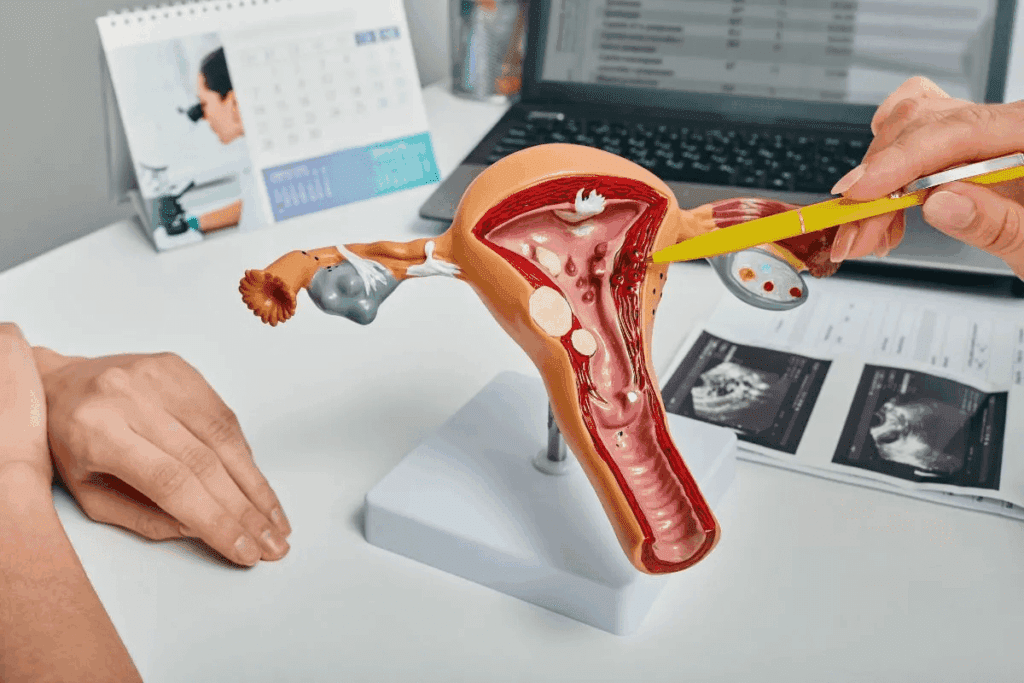
It’s important to understand the female reproductive system’s layout. This system has many organs that work together. They help with reproductive processes.Key Anatomical Components
The female reproductive system has key parts. The uterus, cervix, and endometrium are essential.
The uterus is a muscular organ with three parts: the body, cervix, and fundus. Its wall has three layers: the endometrium, myometrium, and serosa. The endometrium, the innermost layer, changes a lot during the menstrual cycle.
Functional Relationships Between Organs
The organs in the female reproductive system work together. The cervix links the uterus to the vagina. It lets menstrual blood and sperm pass through.
Organ | Function |
Uterus | Supports fetal development during pregnancy |
Cervix | Connects the uterus to the vagina, allowing for the passage of menstrual blood and sperm |
Endometrium | Undergoes changes throughout the menstrual cycle, preparing for possible embryo implantation |
What Is the Endometrial Canal?
The endometrial canal is a key part of the female body. It’s the main area inside the uterus. This area is covered by the endometrium, a tissue that’s important for the menstrual cycle and pregnancy.
Anatomical Definition and Location
The endometrial canal is the space inside the uterus. It’s lined by the endometrium. It’s found between the uterine horns and goes from the internal cervical os to the uterus’s top. Its shape looks like an inverted triangle when seen in a certain way.
Physical Characteristics and Dimensions
The size of the endometrial canal can change. It’s different for everyone and varies with the menstrual cycle. The lining of the canal, the endometrium, gets thicker or thinner based on hormones.
Relationship to Surrounding Structures
The endometrial canal is closely tied to other parts of the female reproductive system. It’s surrounded by the myometrium, the uterus’s muscle layer. This muscle helps with labor and menstruation. The canal also connects to the cervical canal through the internal cervical os.
Knowing about the anatomical definition and location of the endometrial canal is important. It helps us understand its role in health and how to diagnose problems.
The Endometrium: Lining of the Canal
The endometrium lines the endometrial canal and has two layers. It’s key in the female cycle, changing a lot to get ready for pregnancy.
The Basal Layer: Regenerative Foundation
The basal layer stays the same all month. It has stem cells for regrowing the top layer after bleeding. This layer keeps the endometrium working right.
The Functional Layer: Responsive Tissue
The functional layer changes a lot with hormones. It grows with estrogen and changes with progesterone. If there’s no pregnancy, it sheds and grows back with the basal layer’s help.
Cellular Composition and Organization
The endometrium has many cell types like epithelial, stromal, and immune cells. These cells are organized well, with glandular cells making glands for secretion and implantation.
Cellular Composition of the Endometrium
Cell Type | Function | Location |
Epithelial Cells | Form glands, involved in secretion | Glandular structures within the endometrium |
Stromal Cells | Supportive role, involved in decidualization | Surrounding the glands and blood vessels |
Immune Cells | Immune regulation and tolerance | Throughout the stroma and around blood vessels |
Knowing about the endometrium’s cells and how they’re organized helps us understand its role in reproductive health. It shows how it changes during the menstrual cycle.
Endometrial Canal Changes During the Menstrual Cycle
The endometrial canal changes a lot during the menstrual cycle. It gets ready for a possible pregnancy. These changes are key for reproductive health and happen because of hormone changes.
Proliferative Phase: Estrogen-Driven Growth
In the proliferative phase, the endometrium grows because of estrogen. This phase is when the endometrial lining grows back after the last period. Estrogen makes the endometrial glands and stroma grow, making the lining thicker.
This phase is very important for getting ready for a pregnancy. The endometrial glands get more twisted and the stroma gets denser. This makes a good place for the embryo to implant.
Secretory Phase: Progesterone-Mediated Transformation
After ovulation, the secretory phase starts. Progesterone changes the endometrium during this time. Progesterone makes the endometrial glands more twisted and secretory. They produce nutrients that help the embryo grow.
- The endometrial stroma gets more fluid, helping implantation.
- The glands release proteins and other nutrients for the embryo.
- The endometrium gets thicker, getting ready for implantation.
Menstruation: Shedding and Renewal Process
If there’s no pregnancy, the corpus luteum breaks down. This leads to less progesterone. The drop in progesterone starts menstruation, when the endometrial lining sheds. Menstruation is a complex process that includes the contraction of spiral arteries, causing the endometrium to die off.
After shedding, the endometrium starts to renew itself. The basal layer of the endometrium stays intact. It acts as a foundation for the next menstrual cycle.
Endometrial Glands and Secretory Functions
Endometrial glands are key for implantation and growth of the embryo. They are a big part of the endometrium, playing a big role in female reproduction.
Types and Distribution of Glandular Cells
The endometrium has many glands with glandular cells. These cells make secretions that help with reproduction. The number and type of cells change with the menstrual cycle.
Glandular cells mainly live in the functional layer of the endometrium. This layer is shed during menstruation and grows back in the proliferative phase. The basalis layer has more glands, keeping a steady supply of cells.
Biochemical Composition of Secretions
The secretions from endometrial glands are full of proteins, lipids, and other important molecules. These secretions help the embryo implant and grow. The types of molecules in these secretions change with the cycle, due to hormone changes.
Key parts of endometrial secretions include:
- Glycodelin: A protein that helps implantation
- Cytokines: Molecules that help the embryo and endometrium talk to each other
- Growth factors: Proteins that help cells grow and change
Functional Significance of Endometrial Fluids
Endometrial fluids, made by the glands, are very important for reproduction. They give nutrients to the growing embryo and help it implant.
Component | Function |
Glycodelin | Supports implantation |
Cytokines | Facilitates communication between embryo and endometrium |
Growth factors | Promotes cellular growth and differentiation |
In conclusion, endometrial glands and their secretions are very important for reproductive health. Learning about them helps us understand how the endometrium and embryo work together.
The Endocervical Canal and Its Connection
The endocervical canal is a key part of the female body. It connects directly with the endometrial canal. This link is important for many reproductive tasks.
Anatomical Junction with the Endometrial Canal
The endocervical canal links the cervix’s outer opening to the uterine cavity. This spot is key for menstrual blood flow and sperm passage. It marks a transition from cervical mucosa to endometrium.
Histological Differences Between Canals
The endocervical canal and the endometrial canal are different. The endocervical canal has a single layer of columnar cells that make mucus. The endometrial canal has cells that change with the menstrual cycle. These differences help each canal do its job.
The Transformation Zone: Where Canals Meet
The transformation zone is where the endocervical canal meets the endometrial canal. It’s a spot that’s often affected by cancer. Knowing about this area is key for finding and treating cervical problems.
Cervical Canal Fluid and Barrier Functions
The cervical canal’s fluid is key to its role in reproduction. It changes a lot during the menstrual cycle. This change is important for reproductive health.
Mucus Production Throughout the Cycle
The cervical canal makes mucus that changes with hormones. When you’re fertile, the mucus is thin and lets sperm through. It’s thicker and blocks sperm at other times.
This change helps sperm get through during ovulation. It keeps them out at other times. This is important for fertility.
Protective Mechanisms Against Pathogens
The mucus also keeps bad stuff out. It traps and kills bacteria and other harmful things. It has immune factors that help protect the reproductive tract.
This barrier is key to keeping the reproductive area healthy. It stops infections from going up into the upper genital tract.
Sperm Selection and Transport Facilitation
When you’re fertile, the mucus helps sperm move through the cervical canal. It chooses sperm based on how well they move and look. This means only the best sperm get to the egg.
This process is important for making sure the sperm are healthy. It helps the embryo grow well.
The Endometrial Canal’s Role in Conception and Pregnancy
The endometrial canal is key for successful conception. It’s more than just a path for sperm and embryos. Its structure and function are vital for pregnancy.
Sperm Navigation Through the Canal
Sperm navigating the endometrial canal is complex. Factors like the canal’s size, cervical mucus, and uterine contractions play a role. The endometrial canal’s environment supports sperm survival and transport, helping fertilization.
Studies show the canal’s secretions are important for sperm selection and transport. These secretions change throughout the menstrual cycle. They optimize conditions for sperm during the fertile window.
Embryo Implantation Mechanisms
Embryo implantation is a key step in pregnancy. The endometrial canal’s lining changes to support implantation. The endometrium becomes receptive to the embryo through decidualization, involving hormonal and molecular changes.
Implantation involves a complex interaction between the embryo and the endometrium. Adhesion molecules, growth factors, and immune regulation are key factors.
Factor | Role in Implantation |
Adhesion Molecules | Facilitate embryo attachment to the endometrium |
Growth Factors | Support embryonic development and endometrial receptivity |
Immune Responses | Regulate the maternal immune system to tolerate the embryo |
Early Pregnancy Changes in the Canal
In early pregnancy, the endometrial canal changes a lot. The endometrium thickens and differentiates, forming the decidua. This supports the pregnancy.
These changes involve hormonal regulation, angiogenesis, and immune modulation. The endometrial canal’s environment is vital for early pregnancy. It ensures the embryo gets the nutrients it needs for growth.
Hormonal Regulation of the Endometrial Environment
The endometrium changes a lot with hormonal shifts. This change is key for it to work right. It helps with embryo implantation and keeps pregnancy going.
Estrogen Receptors and Signaling Pathways
Estrogen is very important for the endometrium’s growth and change. Estrogen receptors (ER), mainly ERα, help estrogen work in the endometrium. When estrogen binds to these receptors, it starts certain pathways. These pathways make genes that help cells grow and change.
The number of estrogen receptors changes throughout the menstrual cycle. This change helps the endometrium get ready for an embryo.
Progesterone’s Molecular Effects
Progesterone is also key, mainly in the luteal phase. Progesterone receptors (PR) help it work, making the endometrium ready for implantation and early pregnancy.
- Differentiation of Endometrial Stromal Cells: Progesterone turns endometrial stromal cells into decidual cells. This is vital for implantation.
- Regulation of Gene Expression: Progesterone controls genes for implantation and keeping pregnancy.
Inflammatory Mediators and Growth Factors
Other than hormones, inflammatory mediators and growth factors are also important. They help with endometrial receptivity, blood vessel growth, and tissue changes.
- Cytokines and chemokines manage the immune response in the endometrium.
- Growth factors like VEGF help blood vessels grow. This supports the endometrium’s growth and upkeep.
It’s important to know how hormones, inflammatory mediators, and growth factors work together. This helps us understand the endometrium’s complex environment.
Pathological Conditions of the Endometrial Canal
The endometrial canal can face many health issues. These problems can cause symptoms like pelvic pain and abnormal bleeding. They can also lead to infertility and increase the risk of cancer. It’s important to know about these conditions for proper care.
Endometriosis and Adenomyosis
Endometriosis and adenomyosis are conditions where endometrial tissue grows abnormally. Endometriosis happens when this tissue grows outside the uterus, causing inflammation and scarring. Adenomyosis is when this tissue grows into the uterus’s muscular wall, leading to heavy bleeding and pain.
These conditions can greatly affect your life and reproductive health. Symptoms include pelvic pain, heavy menstrual bleeding, and infertility. Treatment options include hormonal therapies and surgery.
Polyps and Hyperplasia
Endometrial polyps are growths in the uterine cavity that can cause irregular bleeding. They are usually benign but can be linked to cancer risk. Endometrial hyperplasia is when cells in the endometrium grow too much, which can lead to cancer if not treated.
Factors that increase the risk of these conditions include hormonal imbalances and obesity. Diagnosis involves ultrasound and biopsy. Treatment can range from hormonal management to surgical removal.
Endometrial Cancer
Endometrial cancer starts in the uterus’s lining and is a common gynecological cancer. Risk factors include unopposed estrogen exposure and obesity. Symptoms include postmenopausal bleeding or irregular menstrual bleeding.
Early detection is key, with diagnosis through biopsy. Treatment depends on the cancer’s stage and grade, including surgery, radiation, and chemotherapy.
Structural Abnormalities and Adhesions
Structural abnormalities and adhesions in the uterine cavity can also affect the endometrial canal. These can cause infertility, recurrent miscarriage, and menstrual issues.
Diagnosis often involves imaging studies like ultrasound or MRI, and sometimes hysteroscopy. Treatment may include surgery to correct anomalies or remove scar tissue.
Diagnostic and Imaging Techniques for Endometrial Assessment
Many methods are used to check the endometrium and decide on treatments. These tools help see if the endometrium is healthy and find problems that might affect it.
Transvaginal Ultrasound Evaluation
Transvaginal ultrasound is a key tool for checking the endometrium. It shows clear pictures of the uterus and how thick the endometrium is. This method is great for measuring the endometrium, spotting issues like polyps or fibroids, and planning more tests.
Key benefits of transvaginal ultrasound include:
- It’s non-invasive and quick.
- It gives clear images of the endometrium.
- It accurately measures the endometrium’s thickness.
Hysteroscopy and Direct Visualization
Hysteroscopy lets doctors see inside the uterus. A thin, lighted telescope (hysteroscope) is put through the cervix into the uterus. It’s very useful for finding and treating problems like endometrial polyps, adhesions, and septa.
The advantages of hysteroscopy include:
- It lets doctors see the inside of the uterus directly.
- It can do biopsies or remove problems during the procedure.
- It’s minimally invasive and has a quick recovery.
Endometrial Biopsy and Sampling Methods
Endometrial biopsy takes a sample of endometrial tissue for tests. It’s key for finding issues like endometrial hyperplasia or cancer. There are different ways to take the sample, like with a Pipelle catheter or a Novak curette.
Endometrial biopsy is useful for:
- Figuring out why there’s abnormal bleeding.
- Looking into infertility issues.
- Checking how well hormone therapy is working.
Advanced Imaging Modalities
Techniques like saline infusion sonography (SIS) and magnetic resonance imaging (MRI) give more info about the endometrium and nearby areas. SIS adds saline to the uterus for better ultrasound images. MRI shows detailed pictures of the uterus and can spot complex problems.
The benefits of advanced imaging include:
- They show more details of the endometrium and nearby areas.
- They help find complex problems more accurately.
- They help plan surgeries.
Conclusion: The Endometrial Canal’s Vital Importance in Women’s Health
The endometrial canal is key to women’s reproductive health. It’s where the embryo implants and grows. Its role is closely tied to the menstrual cycle, showing how hormones affect it.
Knowing about the endometrial canal helps us see its role in reproduction and menstrual health. Its health is vital for women’s overall health. It affects fertility and well-being.
By understanding the endometrial canal, we can handle health issues better. This includes conditions like endometriosis and adenomyosis. It shows we need more research and education on it.
FAQ
What is the endometrial canal?
The endometrial canal is the space inside the uterus. It’s lined with the endometrium. This area is key for reproduction and menstrual health.
What is the function of the endometrial canal?
It helps the embryo implant and grow. The endometrial canal changes throughout the menstrual cycle.
What is the endocervical canal?
The endocervical canal is a narrow part of the cervix. It connects the outside to the uterus. It’s covered in cells that make mucus.
How do the endocervical and endometrial canals connect?
The endocervical canal meets the endometrial canal at the internal cervical os. This forms a continuous path.
What is the role of cervical canal fluid?
Cervical canal fluid, or mucus, helps sperm move. It also acts as a barrier against harmful bacteria. The type of mucus changes throughout the cycle.
What are the changes in the endometrial canal during the menstrual cycle?
The endometrial canal goes through phases. It prepares for implantation, then sheds if there’s no pregnancy.
How do hormonal changes affect the endometrial canal?
Hormones like estrogen and progesterone control the endometrium. They influence growth and shedding of the lining.
What pathological conditions can affect the endometrial canal?
Issues like endometriosis, adenomyosis, and cancer can affect the endometrial canal. These problems can harm reproductive health.
How is the endometrial canal assessed?
Doctors use ultrasound, hysteroscopy, and biopsies to check the endometrium. Advanced imaging helps too.
What is the significance of the transformation zone?
The transformation zone is where the endocervical and endometrial canals meet. It’s important because it can show signs of disease.
How does the endometrial canal support conception and pregnancy?
It helps sperm reach the egg and supports implantation. The endometrial canal is key for a successful pregnancy.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6257623/