Endometriosis affects millions of women worldwide. It’s when endometrial tissue grows outside the uterus, causing health problems. This condition is closely tied to hormone imbalance, mainly with estrogen and progesterone. Understanding how endometriosis and hormone levels are related and how it affects fertility.
This imbalance leads to symptoms like pelvic pain, heavy bleeding, and lower fertility. Studies show endometriosis relies on estrogen. Hormonal shifts can start in a woman’s 30s. It’s vital to grasp how endometriosis and hormone levels interact to find good treatments.
Key Takeaways
- Endometriosis is linked to significant hormone imbalance.
- Estrogen dominance and progesterone resistance are characteristic of endometriosis.
- Hormonal changes associated with endometriosis can start in a woman’s 30s.
- Endometriosis affects approximately one in ten women of reproductive age.
- Understanding hormone imbalance is key to treating endometriosis effectively.
Understanding Endometriosis

Endometriosis affects about 10% of women of childbearing age worldwide. This means around 176 million people globally. It’s a chronic condition where tissue like the uterus lining grows outside the uterus, causing health problems.
Definition and Prevalence
Endometriosis is when tissue like the uterus lining grows outside the uterus. This tissue, or endometrial implants, can be found on ovaries, fallopian tubes, and the tissue that holds the uterus in place.
The exact cause of endometriosis is not known. But genetics, hormonal influences, and environmental factors are thought to play a role. It’s more common in women with a family history of endometriosis and those who have never given birth.
Common Symptoms and Presentation
Endometriosis symptoms vary among women. Common ones include pelvic pain, heavy or irregular menstrual bleeding, and infertility. The pain can happen during menstruation, during sex, or at any time, and can be mild or severe.
Other symptoms include bloating and swelling, fatigue, and digestive issues. The severity of symptoms doesn’t always match the extent of the disease. Some women with little endometriosis may have severe pain, while others with a lot may have mild symptoms.
Understanding endometriosis is key for healthcare providers to diagnose and treat it well. Recognizing symptoms and knowing how common it is helps support women with this condition.
The Hormonal Foundation of Endometriosis

Understanding the hormonal basis of endometriosis is key to understanding its impact on women’s health. This condition is heavily influenced by hormones, mainly estrogen.
Normal Hormone Function in the Menstrual Cycle
The menstrual cycle is controlled by a balance of hormones like estrogen and progesterone. Estrogen helps the endometrium grow. Progesterone gets it ready for pregnancy. If pregnancy doesn’t happen, the endometrium sheds.
Important hormones in the cycle are:
- Estrogen: Stimulates endometrial growth
- Progesterone: Prepares the endometrium for implantation
- FSH (Follicle-Stimulating Hormone): Regulates follicle development
- LH (Luteinizing Hormone): Triggers ovulation
How Endometriosis Disrupts Hormonal Balance
Endometriosis messes with this balance, causing estrogen dominance and progesterone resistance. It’s estrogen-dependent, meaning estrogen helps endometrial lesions grow. This leads to more inflammation, pain, and symptoms.
The disruption caused by endometriosis includes:
- Increased local estrogen production within endometrial lesions
- Progesterone resistance, reducing the effectiveness of progesterone in controlling endometrial growth
- Inflammation and pain due to hormonal imbalances
Understanding how endometriosis affects hormones helps us see its complexity. It shows why we need treatments that tackle symptoms and hormonal causes.
Endometriosis and Hormone Levels: The Direct Connection
Research shows a strong link between endometriosis and hormonal imbalance. Endometriosis is when tissue like the uterus lining grows outside the uterus, causing pain. Hormonal changes throughout the menstrual cycle play a big role in this condition.
Research Evidence on Hormonal Dysregulation
Women with endometriosis often have hormonal imbalances. This means their estrogen and progesterone levels are not normal. This imbalance helps endometrial lesions grow and stay active.
High estrogen levels can make endometrial tissue grow. But, if the body doesn’t respond well to progesterone, it can mess up the hormonal balance even more.
Bidirectional Relationship Between Hormones and Endometriosis
Hormones and endometriosis affect each other. This means we need a full approach to treat endometriosis. Hormonal changes can make endometrial lesions grow. But, these lesions can also change the hormonal environment, creating a cycle.
It’s key to understand this relationship to find good treatments. Treatments should tackle both hormonal and symptom issues of endometriosis.
Estrogen Dominance in Endometriosis
Estrogen dominance is key to understanding endometriosis. We’ll see how this hormonal imbalance affects symptoms and how the condition progresses.
Elevated Estrogen Production Mechanisms
In endometriosis, estrogen production is often elevated. This helps endometrial lesions grow and stay alive. The rise in estrogen levels comes from different sources, like the conversion of androgens to estrogens in body tissues.
The aromatase enzyme is important here. It turns androgens into estrogens. In endometriotic tissues, aromatase is more active. This leads to more estrogen being made locally.
Local Estradiol Synthesis in Endometriotic Tissue
Endometriotic lesions can make estradiol locally. This helps them grow and survive. Local estradiol production is a major reason for estrogen dominance in endometriosis.
Endometriotic tissues have the right enzymes to make estradiol. This keeps estrogen levels high. It helps these lesions stick around and causes symptoms.
Estrogen Receptor Expression Changes
Endometriosis also changes how estrogen receptors work. These changes can make estrogen’s effects stronger. It’s like a feedback loop that worsens symptoms.
Estrogen receptors alpha and beta are involved. Changes in their levels can make symptoms worse. It also affects how fast the condition gets worse.
Progesterone Resistance: A Key Feature
Understanding progesterone resistance is key to knowing how endometriosis affects hormone balance. Progesterone resistance means progesterone, a hormone that helps control the menstrual cycle and supports pregnancy, doesn’t work as well. This issue is a big part of why endometriosis happens.
Mechanisms of Progesterone Resistance
Progesterone resistance in endometriosis comes from many factors. It involves how progesterone receptors work, different signaling paths, and the hormonal environment in endometrial lesions.
- Altered Progesterone Receptor Expression: Changes in progesterone receptors in endometriotic tissues have been found.
- Inflammation and Cytokines: The ongoing inflammation in endometriosis can mess with how progesterone receptors function.
- Epigenetic Modifications: Changes in DNA and histone modifications can also affect progesterone receptor activity.
Deficient Progesterone Receptor Expression
Endometriosis is marked by a lack of progesterone receptors. Research shows that both the amount and how well these receptors work are off in endometriotic lesions.
This lack hinders the decidualization process. This means endometrial tissue keeps growing outside the uterus.
Clinical Implications of Progesterone Resistance
Progesterone resistance has big implications for treating endometriosis. It makes hormonal therapies, which often use progesterone or its derivatives, less effective.
- Inadequate Response to Progestin Therapy: Women with this resistance may not get better with progestin treatments.
- Increased Risk of Associated Conditions: This resistance might also raise the risk of other issues, like endometrial hyperplasia and cancer.
Grasping progesterone resistance is vital for finding better treatments for endometriosis. More research into why this resistance happens could lead to new treatments.
Hormone-Driven Inflammation in Endometriosis
Inflammation caused by hormones is a big part of endometriosis. It makes symptoms worse and helps the condition grow. We’ll look at how this affects endometriosis.
Estrogen’s Role in Inflammatory Processes
Estrogen is key in the inflammation seen in endometriosis. It helps endometrial lesions grow and stay alive, leading to more inflammation. Estrogen affects inflammation in many ways, including how it controls immune cells and makes cytokines.
Studies show that women with endometriosis often have more estrogen. This extra estrogen makes inflammation worse. Estrogen made in endometrial lesions makes things even tougher.
Hormonal Factor | Effect on Inflammation | Clinical Implication |
Estrogen | Promotes inflammatory processes | Contributes to pain and lesion growth |
Prostaglandins | Enhances pain signaling | Increases severity of dysmenorrhea |
Cytokines | Regulates immune response | Influences disease progression |
Prostaglandins and Pain Signaling
Prostaglandins are important for pain signals. In endometriosis, they’re made more, making pain worse. Estrogen and prostaglandins work together, making pain and inflammation worse.
“The local production of prostaglandins within endometrial lesions is a key factor in the generation of pain associated with endometriosis.”
Cytokine Production and Immune Dysfunction
Cytokines are proteins that help control the immune system. In endometriosis, cytokines are not made right, leading to immune problems and more inflammation. Cytokines, estrogen, and other hormones work together, helping endometrial lesions grow and stay.
Understanding how hormones and inflammation work in endometriosis is key to finding better treatments. By focusing on these areas, we might be able to help women with endometriosis feel better and live better lives.
Symptoms of Hormone Imbalance in Endometriosis
Hormone imbalance in endometriosis causes both physical pain and emotional issues. Knowing these symptoms is key to managing and treating the condition.
Distinguishing Endometriosis Symptoms from Hormone Imbalance
Endometriosis and hormone imbalance share similar symptoms, making diagnosis hard. Common signs include:
- Pelvic pain and cramping
- Heavy or irregular menstrual bleeding
- Bloating and water retention
- Mood swings and emotional changes
It’s important to tell apart symptoms from endometriosis and hormone imbalance for proper treatment.
How Hormonal Fluctuations Affect Pain Patterns
Hormonal changes in the menstrual cycle affect pain in women with endometriosis. Estrogen levels are key in growing and keeping endometrial lesions, leading to more pain at certain times.
For example, some women feel:
- More pain during ovulation due to hormonal changes
- Worse symptoms before menstruation because of estrogen and progesterone changes
- Less pain during menstruation, but this varies a lot
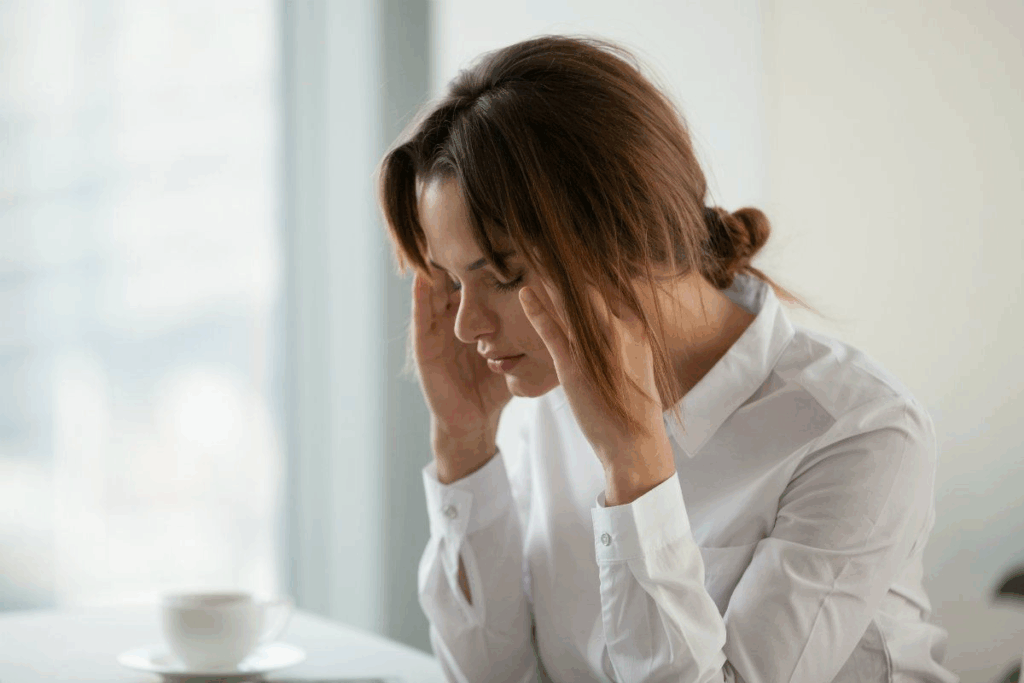
Emotional and Psychological Effects
Hormone imbalance in endometriosis affects not just the body but also the mind. Mood swings, anxiety, and depression are common, likely because of hormonal changes and the long-term nature of the condition.
These emotional and psychological effects can be just as tough as physical symptoms. They can affect daily life and overall happiness. Healthcare providers must tackle these issues fully.
Understanding all symptoms of hormone imbalance in endometriosis helps healthcare providers create better treatment plans. These plans should address both physical and emotional symptoms.
Diagnosing Hormone Imbalances in Endometriosis Patients
It’s key to find hormone imbalances to manage endometriosis well. These imbalances can make symptoms worse. So, finding them accurately is vital for a good treatment plan.
Hormone Testing Methods
There are many ways to test for hormone imbalances in endometriosis patients. Here are a few:
- Serum hormone tests: These measure hormone levels in the blood. They check estrogen, progesterone, and more.
- Saliva hormone tests: These look at hormone levels in saliva. They show how hormones change during the menstrual cycle.
- Urine hormone tests: These test hormone metabolites in urine. They help understand hormone production and how they’re cleared.
We usually start with serum hormone tests. Other tests might be needed based on each patient’s situation.
Interpreting Test Results
Understanding hormone test results needs skill. Hormone levels change a lot during the menstrual cycle. We look at many things when we interpret results, like:
- Hormone levels: We check estrogen, progesterone, and other hormones against the menstrual cycle.
- Symptom correlation: We match hormone levels with symptoms to see how they affect endometriosis.
- Medical history: We also consider the patient’s medical history. This includes past hormone treatments and other important factors.
Getting hormone test results right helps us create treatments that fix specific imbalances.
When to Seek Hormonal Evaluation
Endometriosis patients should get hormonal tests if they have:
- Severe symptoms: Symptoms like heavy bleeding, severe pain, or emotional distress.
- Inconclusive diagnosis: If they’re not sure about their diagnosis or if current treatments aren’t working.
- Treatment resistance: If treatments aren’t working, it might mean a hormone imbalance.
Getting hormonal tests early can really help. It can find and fix hormone imbalances, improving treatment results for endometriosis patients.
Hormone-Based Treatments for Endometriosis
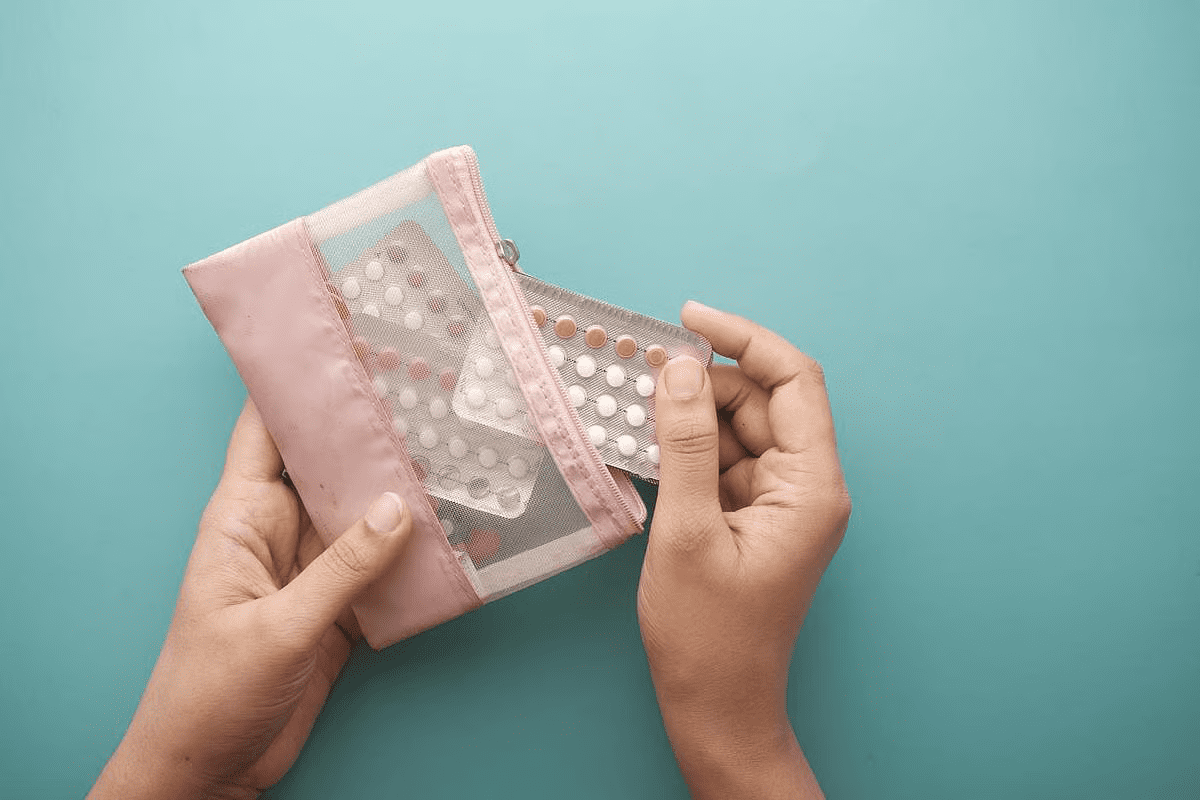
Hormone-based treatments are key in fighting endometriosis symptoms. They aim to balance hormones that cause the condition and pain.
We’ll look at hormone treatments for endometriosis. We’ll see how they work and their benefits. This helps patients and doctors make better choices.
Hormonal Contraceptives
Hormonal contraceptives are often used for endometriosis. They control hormone levels, mainly estrogen, which helps endometrial growth.
Benefits of Hormonal Contraceptives: They lessen menstrual cramps and bleeding. They also help with other symptoms. Using them continuously can stop or reduce periods.
GnRH Agonists and Antagonists
GnRH agonists and antagonists are hormone treatments for endometriosis. They lower estrogen, which slows endometrial growth and symptoms.
GnRH agonists first increase hormone levels then lower them. GnRH antagonists quickly lower hormone levels, acting faster than agonists.
Progestins and Aromatase Inhibitors
Progestins and aromatase inhibitors are other hormone treatments. Progestins stop endometrial growth, while aromatase inhibitors cut estrogen levels.
Progestins can be taken orally or through IUDs. Aromatase inhibitors are often used with other hormones to help patients.
Knowing about these hormone treatments helps us manage endometriosis better. It improves life quality for those with the condition.
Natural Approaches to Balancing Hormones with Endometriosis
Hormone balance is key for managing endometriosis. Natural methods can help achieve this balance. By making dietary changes, taking supplements, and changing your lifestyle, you can reduce symptoms and feel better.
Dietary Modifications for Hormone Balance
Changing what you eat can greatly affect hormone balance and symptoms. Eat whole, nutrient-rich foods like fruits, veggies, whole grains, lean proteins, and healthy fats. Some foods can directly impact hormone levels.
- Foods rich in omega-3 fatty acids, such as salmon and flaxseeds, may help reduce inflammation associated with endometriosis.
- Leafy greens like spinach and kale are rich in antioxidants and may support hormonal health.
- Cruciferous vegetables, including broccoli and cauliflower, contain compounds that may aid in estrogen metabolism.
It’s also important to avoid foods that can worsen symptoms and disrupt hormone balance. These include processed foods, high-sugar diets, and foods high in saturated fats.
Food Group | Examples | Potential Benefits for Hormone Balance |
Omega-3 rich foods | Salmon, flaxseeds, walnuts | Reduces inflammation |
Leafy greens | Spinach, kale, collard greens | Rich in antioxidants, supports hormonal health |
Cruciferous vegetables | Broccoli, cauliflower, Brussels sprouts | Aids in estrogen metabolism |
Supplements That May Help
While diet changes are key, some supplements can also support hormone balance in endometriosis. Always talk to a healthcare provider before starting any supplements.
- Omega-3 supplements: May help reduce inflammation and pain associated with endometriosis.
- Probiotics: Can support gut health, which is linked to hormonal balance and immune function.
- Vitamin D: Important for overall health and may play a role in managing endometriosis symptoms.
Lifestyle Changes to Support Hormonal Health
Changing your lifestyle can also help support hormone balance and manage endometriosis symptoms. Regular exercise, stress management, and enough sleep are all important.
- Exercise: Regular physical activity can help reduce symptoms of endometriosis and support overall hormonal health.
- Stress management: Techniques such as meditation, yoga, or deep breathing exercises can help manage stress, which is known to impact hormone balance.
- Adequate sleep: Ensuring sufficient sleep is critical for hormonal regulation and overall well-being.
By adding these natural approaches to your lifestyle, women with endometriosis may find more ways to manage their symptoms and achieve better hormone balance.
Fertility Implications of Hormone Imbalance in Endometriosis
Endometriosis and hormone imbalance can greatly affect a woman’s ability to get pregnant. This condition causes tissue like the uterine lining to grow outside the uterus. It disrupts hormones, leading to fertility issues.
How Hormonal Disruptions Affect Conception
Hormonal imbalances in endometriosis can make it hard to conceive. Estrogen dominance creates an unfriendly environment for fertilization and implantation. Hormonal changes can also mess with ovulation, making it tough to get pregnant.
Key factors affecting conception include:
- Altered hormone levels affecting ovulation
- Poor egg quality due to hormonal imbalances
- Changes in the uterine environment that hinder implantation
Ovulation and Implantation Challenges
Ovulation and implantation are key for getting pregnant. Hormonal imbalances can mess with ovulation, causing irregular or no ovulation. They can also make the uterine lining less welcoming for implantation.
Some of the challenges include:
- Irregular ovulation due to hormonal fluctuations
- Implantation failure resulting from an unfavorable uterine environment
- Increased inflammation affecting embryo implantation
Fertility Treatment Options
Women with endometriosis and fertility issues have several treatment options. These include hormonal therapies, surgical removal of lesions, and assisted reproductive technologies (ART) like IVF.
Treatment options may involve:
- Hormonal therapies to regulate menstrual cycles and improve fertility
- Surgical removal of endometriotic lesions to enhance fertility
- Assisted reproductive technologies (ART) for direct conception assistance
It’s important for women to talk to healthcare providers. They can help find the best treatment for their condition and fertility goals.
Conclusion
Endometriosis is a complex condition that affects millions of women worldwide. It is linked to significant hormone imbalance. We’ve looked at how estrogen dominance and progesterone resistance play a big role in this disease.
Understanding the hormonal aspects of endometriosis is key to managing its symptoms. Recognizing hormone imbalance signs helps healthcare providers tailor treatments. This approach improves the quality of life for those affected.
The connection between endometriosis and hormone levels is complex. Effective management requires a detailed approach. This includes considering each person’s hormonal profile, medical history, and personal situation. By doing this, we can better treat endometriosis and improve women’s overall well-being.
FAQ
Does endometriosis cause hormone imbalance?
Yes, endometriosis often leads to hormone imbalance. This imbalance is mainly due to too much estrogen and not enough progesterone. These changes can cause various symptoms.
How does endometriosis affect hormone levels?
Endometriosis can mess with hormone levels. It can cause more estrogen to be made and change how estrogen receptors work. This results in hormone imbalance.
What is estrogen dominance in endometriosis?
Estrogen dominance in endometriosis means there’s too much estrogen. This helps endometrial lesions grow, leading to symptoms like pelvic pain and heavy bleeding.
How does progesterone resistance contribute to endometriosis symptoms?
Progesterone resistance means the body doesn’t respond well to progesterone. This can cause irregular bleeding, pelvic pain, and infertility.
Can hormone imbalance in endometriosis affect fertility?
Yes, hormone imbalance can make it hard to get pregnant. It can disrupt ovulation, implantation, and conception.
What are the natural approaches to balancing hormones in endometriosis?
Natural ways to balance hormones include changing your diet and taking supplements like omega-3 fatty acids and vitamin D. Lifestyle changes like managing stress and exercising regularly also help.
How is hormone imbalance in endometriosis diagnosed?
Doctors use hormone tests like blood and saliva tests to check estrogen and progesterone levels. They look at test results along with symptoms and medical history to diagnose.
What are the hormone-based treatments for endometriosis?
Treatments include hormonal contraceptives, GnRH agonists, progestins, and aromatase inhibitors. These aim to lower estrogen levels, stop menstruation, or ease symptoms.
Can endometriosis cause emotional and psychological symptoms?
Yes, hormone imbalance can lead to mood swings, anxiety, and depression. A full treatment plan can help manage these symptoms.
How do hormonal fluctuations affect pain patterns in endometriosis?
Hormonal changes can make pain worse in endometriosis. Some women feel more pain during ovulation or just before their period.
References
World Health Organization. Evidence-Based Medical Guidance. Retrieved from https://www.who.int/news-room/fact-sheets/detail/endometriosis.