Last Updated on December 2, 2025 by Bilal Hasdemir
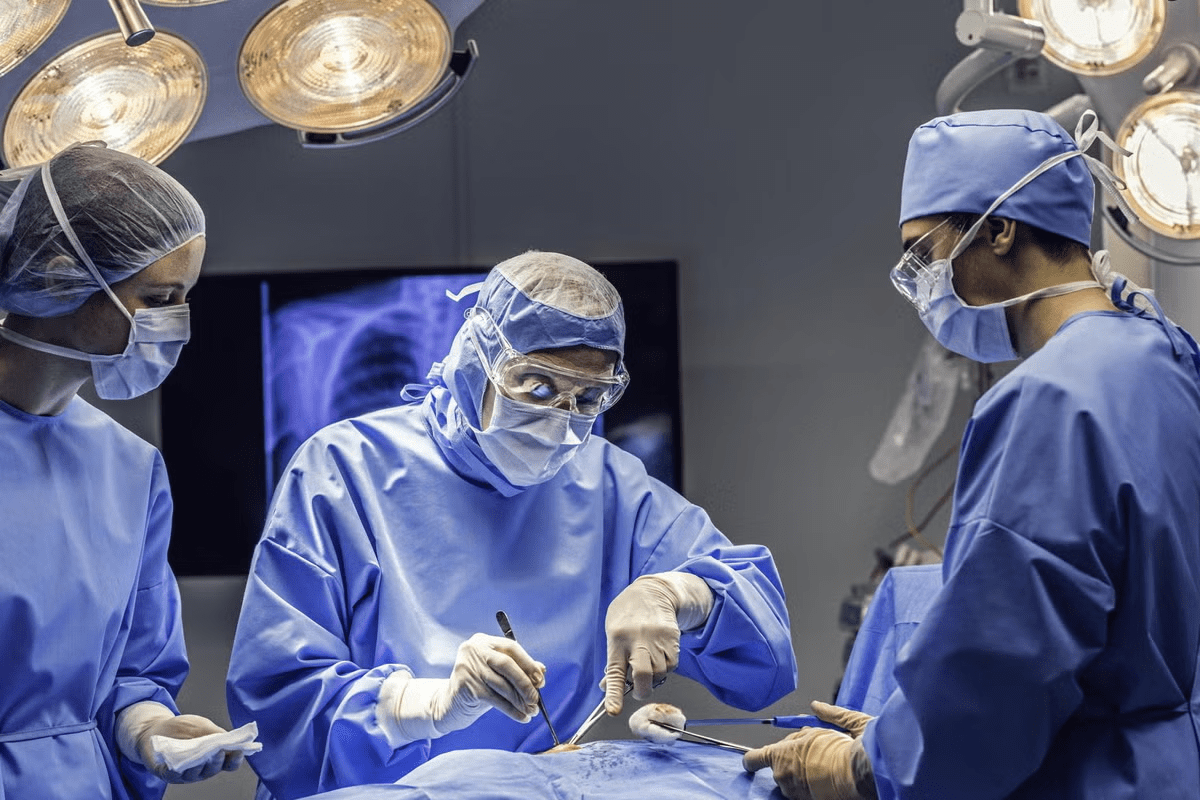
Minimally invasive neurosurgery has changed the game in treating the brain. It offers hope to those who were once too risky for old-school surgery. Thanks to new endoscopic methods, patients are seeing better results. They recover faster and face fewer complications.
Recent studies show a big jump in safety rates for these surgeries. This makes them a good choice for many brain issues. Knowing about the safety and success of endoscopic brain surgery can ease worries.
Key Takeaways
- Minimally invasive neurosurgery offers improved patient outcomes and reduced recovery times.
- Advancements in endoscopic techniques have enhanced the safety of these procedures.
- Endoscopic brain surgery is a viable option for various neurological conditions.
- Safety rates for endoscopic procedures have significantly improved in recent years.
- Understanding the benefits and risks can help patients make informed decisions.
What Is Endoscopic Brain Surgery?
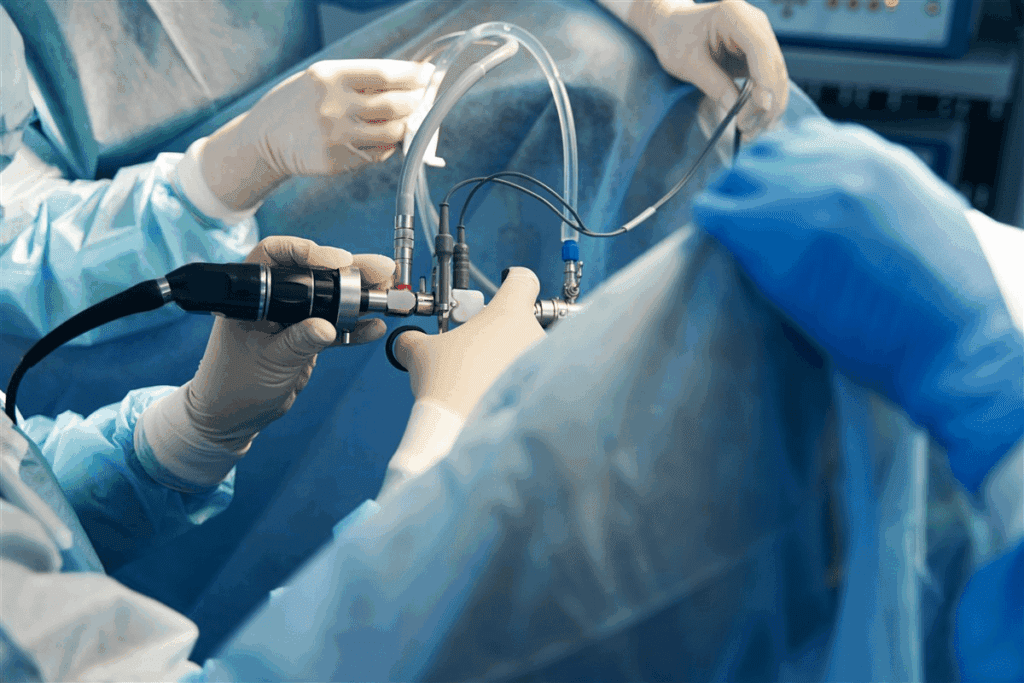
Endoscopic brain surgery is a big step forward in neurosurgical technology. It uses a thin, flexible tube with a camera and light to see and work on the brain. This method is a minimally invasive approach for treating brain problems.
This surgery lets neurosurgeons do complex tasks through small cuts. It causes less damage to the brain and helps patients recover faster than old surgery methods.
Definition and Basic Principles
Endoscopic neurosurgery uses an endoscope to reach and treat brain areas without a big cut in the skull. Its main goal is to harm less of the brain around it. This lowers the chance of problems and makes patients do better.
The surgery starts with small holes in the skull for the endoscope and tools. The camera in the endoscope shows clear pictures of the brain. This helps surgeons work very precisely.
Key Features | Benefits |
Minimally invasive | Less tissue damage |
High-definition visualization | Improved precision |
Smaller incisions | Faster recovery |
Historical Development of Endoscopic Techniques
The history of endoscopic brain surgery has grown a lot. At first, technology was not as good. But, new endoscopic surgery advancements have made these surgeries safer and more effective.
Today, endoscopic neurosurgery uses better cameras, lights, and navigation tools. This lets surgeons do detailed and safe operations.
Traditional vs. Endoscopic Brain Surgery Approaches
There are two main ways to do brain surgery: traditional open craniotomy and endoscopic surgery. The choice depends on the condition, the patient’s health, and the surgeon’s skill.
Open Craniotomy Procedures
Traditional brain surgery often uses open craniotomy. This method needs a big cut and disrupts more tissue. It gives surgeons a clear view of the brain but can cause more damage and longer recovery times.
Key aspects of open craniotomy include:
- Larger incision and craniotomy
- Direct visualization of the surgical site
- Potential for greater tissue trauma
- Longer hospital stays and recovery periods
Minimally Invasive Endoscopic Methods
Endoscopic brain surgery is a newer, less invasive way. It uses small cuts to reach the brain, causing less damage and scarring. This leads to quicker recovery and better results. It’s great for hard-to-reach areas or when precision is key.
The benefits of endoscopic brain surgery include:
- Smaller incisions and reduced tissue disruption
- Less scarring and improved cosmetic outcomes
- Faster recovery times and shorter hospital stays
- Potential for fewer complications and improved safety
As shown in the image below, endoscopic surgery is a precise and less invasive option compared to traditional open craniotomy.
It’s important to know the differences between traditional and endoscopic brain surgery. This helps patients and doctors make the best choice for treatment.
Endoscopic Brain Surgery Safety: The Evidence
Many studies have looked into the safety of endoscopic brain surgery. They have shown it’s safe and effective for some conditions. This method is a good alternative to traditional surgery.
Clinical Studies on Safety Outcomes
Studies have checked how safe endoscopic brain surgery is. They looked at complications, recovery times, and long-term results. These studies found endoscopic surgery has fewer complications than open surgery.
Key findings from recent studies include:
- Reduced risk of infection due to smaller incisions
- Less tissue trauma resulting in faster recovery times
- Lower rates of postoperative complications such as cerebral edema and hemorrhage
Statistical Analysis of Complication Rates
An analysis of complication rates in endoscopic brain surgery shows it’s safe. By combining data from many studies, researchers found important trends. This helps us understand how safe and effective endoscopic surgery is.
A meta-analysis of endoscopic third ventriculostomy (ETV) found a lower complication rate than traditional methods. Such analyses are key to understanding the safety and effectiveness of endoscopic brain surgery.
Procedure | Complication Rate | Study Sample Size |
Endoscopic Third Ventriculostomy | 5.2% | 500 patients |
Endoscopic Tumor Resection | 7.1% | 300 patients |
These results highlight the need for more research into endoscopic brain surgery. They also show the importance of standard safety protocols in neurosurgery.
Benefits of Endoscopic Neurosurgery
Endoscopic neurosurgery is a safer and more effective way to treat brain issues. It’s a new method that’s getting a lot of attention. We’ll look at why it’s so beneficial.
Reduced Tissue Trauma and Scarring
One big plus of endoscopic neurosurgery is less tissue damage and scarring. Surgeons use small cuts and a camera to guide them. This means they can be more precise and cause less harm to the brain.
This approach also leads to less pain and scarring after surgery. Patients feel more comfortable and have less noticeable scars. Plus, it lowers the chance of infection and speeds up healing.
Shorter Hospital Stays and Cost Effectiveness
Endoscopic neurosurgery means patients stay in the hospital for less time. This is because it’s less invasive and leads to fewer complications. It makes patients happier and saves money too.
With shorter stays, patients avoid extra costs for long-term care. This makes endoscopic neurosurgery a more affordable choice.
Aspect | Traditional Surgery | Endoscopic Neurosurgery |
Hospital Stay | Average 7-10 days | Average 2-3 days |
Recovery Time | Several weeks to months | Several weeks |
Cost | Higher due to longer stays and complications | Lower due to reduced complications and shorter stays |
Faster Recovery Times and Return to Normal Activities
Endoscopic neurosurgery lets patients recover faster than traditional surgery. It causes less damage and scarring. This means patients can get back to their normal lives sooner.
Being able to get back to work and daily activities quickly is a big plus. It’s great for people with busy lives or family commitments.
Potential Risks and Complications
It’s important to know the risks and complications of endoscopic brain surgery. This method is usually safe and works well. But, there are possible risks to consider.
Common Complications
Common issues with endoscopic brain surgery include infection, bleeding, and cerebrospinal fluid (CSF) leakage. Infection rates are low thanks to clean techniques and antibiotics. But, bleeding can happen and might need more surgery to fix.
CSF leakage is another issue. It happens when a path is made through the brain or skull. Usually, it’s treated without surgery, but sometimes more surgery is needed.
Rare but Serious Adverse Events
Rare but serious problems can include damage to important brain parts. Vascular injury is a big risk. It can cause strokes or serious brain problems.
Other rare issues might be neurological deficits. These can be weakness, numbness, or changes in thinking. It depends on where in the brain the surgery is done.
Risk Factors for Complications
Some things can make complications more likely during or after surgery. These include the patient’s health, any other health issues, and how complex the surgery is.
- Those who have had brain surgery or radiation before might be at higher risk.
- The size and where the surgery is done also play a part.
- How experienced the surgeon is and the hospital’s volume of surgeries also matter.
Knowing these risks and complications helps patients make better choices about their treatment.
Patient Selection Criteria for Endoscopic Procedures
Choosing the right patient is key for endoscopic neurosurgery success. It’s about checking the patient’s health, the type of problem, and how well they can handle surgery.
Ideal Candidates for Endoscopic Approaches
Good candidates for endoscopic brain surgery have problems that are easy to reach and treat. This includes some brain tumors, hydrocephalus, and other issues that endoscopy can fix.
Key characteristics of ideal candidates include:
- Lesions that are well-defined and accessible endoscopically
- Good overall health with minimal comorbidities
- Ability to undergo general anesthesia
- Favorable anatomy for endoscopic access
Contraindications and Limitations
Endoscopic brain surgery is great, but it’s not for everyone. It’s not good for complex problems, serious health issues, or when the brain’s shape makes it hard to get to.
Relative contraindications may involve:
- Previous surgeries or radiation therapy that may alter anatomy
- Active infections or inflammatory conditions
- Severe coagulopathy or bleeding disorders
In summary, picking the right patient is vital for endoscopic brain surgery success. By finding the best candidates and knowing what doesn’t work, doctors can make sure patients do well and stay safe.
Common Endoscopic Brain Surgery Procedures and Their Safety Profiles
Endoscopic brain surgery has grown to include many procedures, each with its own safety level. Thanks to new technology and more experience, these surgeries are now safer and work better. We’ll look at some common endoscopic brain surgeries and talk about their safety.
Endoscopic Third Ventriculostomy
Endoscopic third ventriculostomy (ETV) treats hydrocephalus by making a new CSF flow path in the brain. It often replaces the need for a shunt. ETV’s safety is generally good, with success rates that depend on the patient and their condition.
A study in the Journal of Neurosurgery found ETV’s complication rate is about 10%, with serious issues being rare. “ETV is a valuable tool for treating hydrocephalus,” says a top neurosurgeon.
Endoscopic Tumor Resection
Endoscopic tumor resection removes brain tumors through small incisions. It’s used for tumors in or near the ventricles or other reachable spots. The safety of this procedure depends on the tumor’s location and size.
Studies show endoscopic tumor resection is safe and effective, with complication rates similar to or sometimes better than open surgery. Advanced imaging and navigation systems have made it safer.
Endoscopic Transsphenoidal Surgery
Endoscopic transsphenoidal surgery removes pituitary tumors through the nose, avoiding external cuts. This method is safe and works well, with low complication rates when done by skilled surgeons.
Common issues are nasal or sinus problems, but serious problems are rare. Endoscopic methods have lowered risks compared to older techniques.
Other Applications and Their Safety Considerations
Endoscopic techniques are also being used for other treatments, like some epilepsy cases and colloid cysts. The safety of these new uses is being studied, but early results are encouraging.
Choosing the right patient is key for good results and low risks. The skill of the surgeon and modern technology also play big roles in making endoscopic brain surgery safe and effective.
Technological Advancements Improving Safety
Technology has greatly improved the safety and success of endoscopic brain surgery. New technologies have made these surgeries safer and more effective. This has led to better results for patients.
High-Definition Visualization Systems
High-definition (HD) visualization systems are a big step forward in brain surgery. They give surgeons clearer, more detailed images of the area they are working on. This makes their work more precise and reduces the chance of problems.
“The clarity provided by HD visualization is unparalleled, enabling us to navigate complex anatomical structures with greater confidence.” This is very important in surgeries where being exact is key.
Navigation and Imaging Integration
Navigation and imaging technologies have changed neurosurgery a lot. Intraoperative imaging like MRI and CT scans lets surgeons update their navigation as they go. This keeps the surgery on track and accurate.
- Improved accuracy in tumor resection
- Enhanced safety during complex dissections
- Better outcomes in patients with challenging anatomies
Specialized Instruments for Minimally Invasive Access
New specialized instruments have made brain surgery safer. These tools are made for minimally invasive access. They offer the needed precision and control.
“The development of instruments tailored to endoscopic neurosurgery has been a game-changer, allowing for more precise and safer procedures.”
These advances have made surgery safer for patients. They help make endoscopic brain surgery more effective and safe.
The Role of Surgeon Expertise in Endoscopic Neurosurgery Outcomes
In endoscopic neurosurgery, the surgeon’s skill is very important. The procedures are complex, needing a lot of skill. This makes the surgeon’s role key to success.
Learning Curve and Training Requirements
Endoscopic neurosurgery is hard to learn. Surgeons need special training. This includes practice with simulators, watching experienced surgeons, and doing procedures under supervision.
Good training programs are vital. They help surgeons learn to handle the challenges of endoscopic neurosurgery well.
Training Component | Description | Duration |
Theoretical Foundation | Understanding the principles and techniques of endoscopic neurosurgery | 2 months |
Simulation Training | Practicing endoscopic skills on simulators | 3 months |
Observational Learning | Observing experienced surgeons perform procedures | 6 months |
Supervised Practice | Performing procedures under the supervision of experienced surgeons | 12 months |
Volume-Outcome Relationship in Endoscopic Procedures
Studies show that more procedures lead to better results. Surgeons who do more procedures get better with time.
High-volume centers have better care because of their experience. It’s best to go to these centers for the best chance of success.
Surgeon skill is very important for good results in endoscopic neurosurgery. We need to keep improving training to help patients and advance the field.
Infection Rates and Prevention in Endoscopic Brain Surgery
Infections after endoscopic brain surgery are rare but serious. They highlight the importance of strict infection control. We must study the rates of infection in both traditional and endoscopic surgeries. We also need to look at how we prevent these problems.
Comparative Infection Rates Between Traditional and Endoscopic Approaches
Endoscopic brain surgery often has fewer infections than traditional open craniotomy. This is because endoscopic surgery is less invasive. It has smaller cuts and less damage to tissue. Research shows endoscopic surgery’s infection rate is 1-2%, much lower than the 5-10% for open surgery. But, infection rates can change based on the surgery, the patient’s health, and the surgeon’s experience.
Infection Prevention Protocols and Best Practices
To lower infection risks in endoscopic brain surgery, we use several prevention steps. These include:
- Preoperative Antibiotics: Giving antibiotics before surgery helps prevent infections.
- Sterile Technique: Keeping the surgery area clean is key. This means using sterile tools and following hand hygiene rules.
- Intraoperative Irrigation: Using fluids during surgery helps keep the area clean and lowers infection risks.
- Postoperative Care: Watching patients closely after surgery for infection signs and handling any problems quickly.
By following these steps and keeping up with new research, we can lower infection risks in endoscopic brain surgery. This improves patient safety and results.
Patient Decision-Making and Informed Consent
Informed consent is key for patients getting endoscopic brain surgery. It’s about weighing risks and benefits. This helps patients make smart choices about their care, knowing what the surgery means.
Weighing the Risks and Benefits
Knowing the risks and benefits of endoscopic brain surgery is important. Benefits include less tissue damage, shorter hospital stays, and quicker recovery. But, there are risks like infection, bleeding, and complications from the condition being treated.
Patients must think about these points and their health. For example, someone with a serious brain condition might see the benefits of endoscopic surgery as worth the risks. But, someone with a milder condition might need to weigh if the risks are too high.
Patient Experiences and Perspectives
Experiences with endoscopic brain surgery vary a lot. This depends on the surgery’s complexity, the patient’s health, and their strength. Hearing from others can offer valuable insights and prepare patients for their own surgery.
Some patients have a smooth recovery with little pain, while others face more hurdles. Knowing about these different experiences can help set realistic hopes and lower anxiety.
Choosing to have endoscopic brain surgery is a personal decision. It should be made with careful thought and expert advice. By understanding the risks and benefits, asking the right questions, and learning from others, patients can make choices that are best for them.
Recovery and Long-Term Outcomes After Endoscopic Brain Surgery
Endoscopic brain surgery has changed neurosurgery for the better. It’s safer and leads to a smoother recovery. Let’s look at what makes a surgery successful.
Long-Term Success Rates and Quality of Life
Endoscopic brain surgery often works well in the long run. Many patients see big improvements. For example, endoscopic third ventriculostomy works for over 80% of people with hydrocephalus.
Patients often feel better and can do things they couldn’t before. It’s important to keep up with follow-up care to make sure everything is okay.
Follow-up Care and Monitoring
Follow-up care is key to making sure patients are doing well. They usually see their doctor at one week, one month, and three months after surgery. This can change based on the patient’s needs.
At these visits, doctors check how the patient is doing, manage any ongoing issues, and give advice on getting back to normal. They might also do imaging tests to check the surgery site.
By following the recovery plan and going to follow-up appointments, patients can have the best chance of a good outcome and a better life after surgery.
Conclusion
Endoscopic brain surgery is now a safe and effective method. It causes less tissue damage and allows for quicker recovery. This article has covered its safety, benefits, and risks.
It’s important to choose the right patient and have skilled surgeons. Good care after surgery is also key.
As neurosurgery technology gets better, we’ll see more improvements in endoscopic brain surgery. These advancements will make procedures safer and more precise. This will give patients more treatment options.
Knowing the good and bad of endoscopic brain surgery helps everyone make better choices. This leads to better health for patients.
FAQ
Is endoscopic brain surgery a safe procedure?
Yes, endoscopic brain surgery is usually safe. But, like any surgery, it can have risks and complications.
What are the benefits of endoscopic brain surgery compared to traditional brain surgery?
Endoscopic brain surgery has many benefits. It causes less damage, leaves less scarring, and you can leave the hospital sooner. You also recover faster and might have a better quality of life.
What are the possible risks and complications of endoscopic brain surgery?
Risks include infection, bleeding, and leakage of cerebrospinal fluid. There’s also a chance of damage to brain tissue. Though rare, serious problems can happen.
How is patient safety ensured during endoscopic brain surgery?
Safety is ensured by choosing the right patients and having skilled surgeons. Advanced technology, like high-definition systems, also plays a big role.
What is the role of surgeon expertise in endoscopic neurosurgery outcomes?
A surgeon’s skill is key to a good outcome. They need special training and experience with endoscopic procedures.
How can infection be prevented during endoscopic brain surgery?
Preventing infection involves using clean equipment and antibiotics. Following strict protocols helps keep patients safe.
What is the typical recovery timeline after endoscopic brain surgery?
Recovery time varies. Generally, it takes a few weeks. Some people can get back to normal in just a few days.
What are the long-term success rates and quality of life after endoscopic brain surgery?
Most patients see big improvements in their symptoms and life quality. Success rates are usually high.
How can I make an informed decision about undergoing endoscopic brain surgery?
Talk to your neurosurgeon about the surgery’s risks and benefits. Ask questions and understand what to expect.
What are the latest advancements in endoscopic brain surgery technology?
New tech includes better visualization systems and tools for less invasive surgery. These advancements make the procedure safer and more effective.
References
National Center for Biotechnology Information. Endoscopic Endonasal Skull Base Surgery Complication Avoidance: A Contemporary Review. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9776068/