Last Updated on December 2, 2025 by Bilal Hasdemir

Many patients wonder if they’ll be awake during endoscopic surgery. It depends on the procedure type and the patient’s health.
The thought of being awake during a procedure can be scary. But, anesthesia for endoscopy is managed to keep you comfortable. Sedation is often used to relax patients.
We focus on your comfort at our institution. Whether it’s a simple endoscopy or a complex procedure, we’ll talk about sedation options. This way, you’ll feel as comfortable as possible.
Key Takeaways
- Endoscopic surgery can be performed with or without being awake.
- The type of anesthesia or sedation used depends on the procedure and patient health.
- Patient comfort is a top priority during endoscopic procedures.
- Sedation during endoscopy helps patients relax.
- We’ll discuss your sedation and anesthesia options with you.
What is Endoscopy and How Does it Work?
Endoscopy is a key tool in modern medicine. It lets doctors see inside the body without surgery. A flexible or rigid tube with a camera and light is used to look at internal organs.
Definition and Medical Purpose
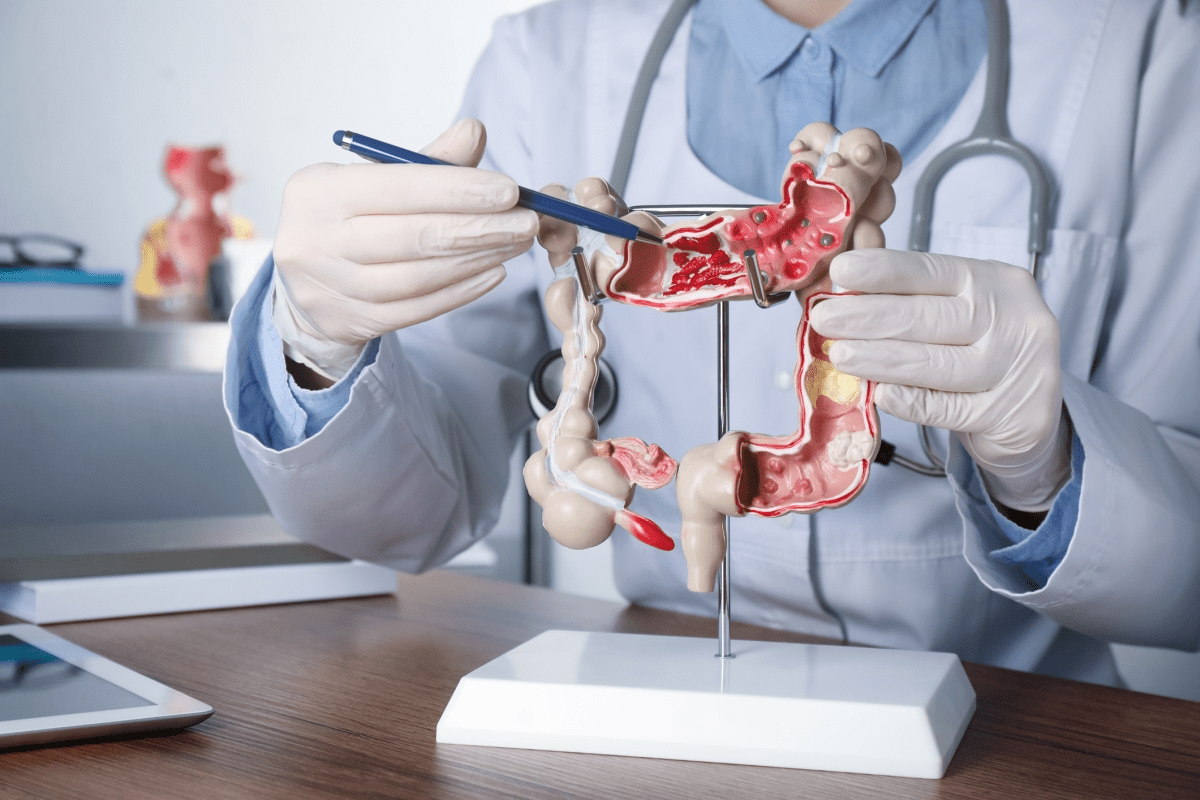
Endoscopy lets doctors see the upper part of the GI tract and other organs. It helps diagnose and sometimes treat problems. It’s great for finding ulcers, inflammation, and tumors.
Basic Principles of Endoscopic Procedures
Endoscopy uses a special tube with a light and camera. This lets doctors see organs on a screen. The tube can also have tools for biopsies or small surgeries.
Procedure Type | Description | Common Applications |
Upper Gastrointestinal Endoscopy (EGD) | Examines the esophagus, stomach, and duodenum | Diagnosing ulcers, gastritis, and esophageal varices |
Colonoscopy | Examines the colon and rectum | Detecting colon cancer, polyps, and diverticulosis |
Bronchoscopy | Examines the airways and lungs | Diagnosing lung infections, tumors, and bleeding |
Understanding endoscopy helps patients see its importance in their care.
Types of Endoscopic Procedures and Their Applications
Endoscopy is very versatile, used in many medical fields. It helps doctors look inside the body. This gives them important information for diagnosis and treatment.
Upper Gastrointestinal Endoscopy (EGD)
EGD, or Upper Gastrointestinal Endoscopy, looks at the upper digestive system. This includes the esophagus, stomach, and the start of the small intestine. It helps find problems like ulcers, inflammation, and tumors.
Applications of EGD:
- Diagnosing gastroesophageal reflux disease (GERD)
- Identifying the cause of difficulty swallowing
- Investigating the source of gastrointestinal bleeding
- Removing foreign objects from the digestive tract
Lower Gastrointestinal Endoscopy (Colonoscopy)
Colonoscopy lets doctors see the whole colon. It’s key for finding colorectal cancer and other colon problems.
Key Uses of Colonoscopy:
- Screening for colorectal cancer
- Diagnosing the cause of rectal bleeding
- Identifying inflammatory bowel disease (IBD)
- Removing polyps to prevent cancer
Bronchoscopy and Respiratory Tract Examination
Bronchoscopy lets doctors look into the lungs. It’s used to diagnose and treat lung issues.
Applications of Bronchoscopy:
- Diagnosing lung infections and diseases
- Investigating the cause of persistent cough or difficulty breathing
- Removing foreign objects or secretions from the airways
- Taking tissue samples for biopsy
Specialized Endoscopic Procedures
There are many specialized endoscopic techniques. These include endoscopic ultrasound (EUS), capsule endoscopy, and arthroscopy. They help doctors examine different parts of the body.
Procedure | Description | Primary Use |
Endoscopic Ultrasound (EUS) | Combines endoscopy and ultrasound to obtain images and samples | Staging cancer, diagnosing pancreatic diseases |
Capsule Endoscopy | A capsule with a camera that travels through the digestive tract | Examining the small intestine for bleeding or disease |
Arthroscopy | Examines the interior of joints | Diagnosing and treating joint conditions |
The Technology Behind Modern Endoscopes
Modern endoscopes have come a long way thanks to years of research and innovation. They now offer better design, function, and diagnostic power. This makes procedures more precise and less invasive.
Components and Design Features
Today’s endoscopes come with high-definition cameras and better lighting. This lets doctors see internal organs more clearly. The key components of a modern endoscope include:
- A flexible or rigid tube that houses the camera and lighting system
- A high-resolution camera that captures detailed images
- Illumination systems, such as LED lights, for better visibility
- Instrument channels for passing specialized tools
- Control mechanisms for navigating the endoscope
These parts work together to give a clear view of the inside. This helps doctors make accurate diagnoses and treatments.
Recent Technological Advancements
In recent years, endoscopy has seen big technological advancements. Some of these include:
- High-Definition Imaging: Better image quality means more accurate diagnoses.
- Narrow-Band Imaging: Makes blood vessels and other structures easier to see.
- Confocal Laser Endomicroscopy: Allows for real-time microscopic examination during the procedure.
- Endoscopic Ultrasound: Combines endoscopy with ultrasound for better views of deeper tissues.
These new technologies have improved the diagnostic and therapeutic capabilities of endoscopy. They help treat various gastrointestinal disorders more effectively.
Conscious Sedation vs. General Anesthesia in Endoscopy
Conscious sedation and general anesthesia are two ways to keep patients comfortable during endoscopies. The right choice depends on the procedure, the patient’s health, and how much discomfort is expected.
Levels of Sedation Explained
Sedation levels for endoscopies vary from minimal to deep. Minimal sedation makes patients relax but they can follow commands. Moderate or conscious sedation keeps patients awake but relaxed, able to respond to commands. Deep sedation makes patients less responsive but they can wake up with strong stimulation.
General anesthesia, by contrast, makes patients completely unconscious. This requires more careful monitoring and support.
Medications Commonly Used
Many drugs are used for sedation in endoscopies. Benzodiazepines, like midazolam, help patients relax and forget the procedure. Opioids, such as fentanyl, are used for pain relief. The choice of drug depends on the sedation level needed, the patient’s health, and the procedure.
Medication Class | Examples | Primary Use |
Benzodiazepines | Midazolam, Diazepam | Sedation, Amnesia |
Opioids | Fentanyl, Meperidine | Pain Relief |
Propofol | Propofol | Deep Sedation, General Anesthesia |
Monitoring During Sedated Procedures
During sedated endoscopies, patients’ vital signs are closely watched. This includes heart rate, blood pressure, oxygen levels, and breathing rate. The monitoring level changes based on the sedation depth and the patient’s health.
Knowing the differences between conscious sedation and general anesthesia helps patients feel more ready for their endoscopy. It also reduces their anxiety about the procedure.
Are You Awake During an Endoscopy? The Reality Explained
Whether you’re awake during an endoscopy isn’t a simple yes or no. It depends on many things. These include the type of endoscopy, your health, and what your doctor prefers.
Consciousness Levels During Different Endoscopic Procedures
Endoscopic procedures vary a lot. Some are simple, while others are more complex. The level of consciousness needed can change based on the procedure and your comfort.
For simple procedures like a gastroscopy, you might stay awake or get local anesthesia. But for more complex or uncomfortable procedures, you might get conscious sedation or even general anesthesia.
Procedure Type | Typical Level of Consciousness | Patient Experience |
Gastroscopy | Awake or Local Anesthesia | Mild discomfort, possible gagging |
Colonoscopy | Conscious Sedation | Relaxed, may not remember procedure |
Complex Interventions | Conscious Sedation or General Anesthesia | Varies, often no memory of procedure |
Patient Awareness and Memory Formation
Patient awareness during endoscopy can differ a lot. Some are fully awake, while others are sedated and remember little to nothing.
Conscious sedation is used in many procedures. It makes patients relax and forget more of the procedure. But, the level of sedation can vary, and some might stay somewhat aware.
What You Might Feel or Experience
Even with sedation, patients might feel some things during the procedure. These can be mild discomfort, pressure, or bloating, depending on the procedure.
Talking to your doctor about your fears before the procedure is key. This helps tailor the sedation to your needs, making the experience more comfortable.
After the procedure, you’ll be watched until the sedation wears off. Most people can go home the same day. But, you might need someone to drive you home because of the sedation’s effects.
Factors That Determine Your Sedation Level for Endoscopic Surgery
Many factors decide how much sedation you’ll need for endoscopic surgery. Knowing these can help you prepare and understand what to expect.
Procedure Complexity and Duration
The type and length of your endoscopy affect your sedation level. More detailed procedures, like therapeutic interventions or multiple biopsies, might need deeper sedation. This ensures you’re comfortable and the procedure goes well.
For example, a simple diagnostic endoscopy might just need a little sedation. But a complex one, like endoscopic retrograde cholangiopancreatography (ERCP), might need more or even general anesthesia.
Patient Medical History and Risk Factors
Your medical history and risks are key in picking the right sedation. If you have chronic illnesses like heart disease or diabetes, your sedation might be adjusted. This is to keep you safe during the procedure.
- Previous bad reactions to sedation or anesthesia
- Respiratory or cardiac conditions
- Medications that could react with sedatives
Patient Preference and Anxiety Management
Your preference and anxiety levels also matter. Some might want to be more sedated because they’re nervous. Others might want to stay more awake.
We listen to your concerns and preferences. We use relaxation exercises or pre-procedure counseling to help with anxiety.
Physician Recommendations
The doctor’s advice is very important. They look at all the factors and decide the best sedation for you. This is based on their experience and judgment.
Our team works together to give you care that fits your needs. We make sure you get the best care possible.
Preparing for Your Endoscopic Procedure: A Complete Guide
We’re here to help you get ready for your endoscopy. We’ll give you clear instructions and tell you what to expect. Preparing well is key for a good procedure, and knowing what to do can make you feel less anxious.
Dietary Restrictions and Fasting Requirements
Following dietary restrictions and fasting rules is very important. The rules depend on the type of endoscopy you’re having. For upper GI procedures, you might need to fast for a few hours to empty your stomach. For lower GI procedures like colonoscopies, you’ll need to follow a special bowel prep that includes dietary changes and laxatives.
It’s very important to follow your doctor’s dietary instructions carefully. Not doing so might mean your procedure is delayed. We’ll give you all the details on what to eat and avoid before your procedure.
Medication Adjustments Before the Procedure
Before your endoscopy, talk to your doctor about your medications. Some meds, like blood thinners, might need to be stopped to avoid bleeding risks. Tell your doctor about all your meds, including supplements and vitamins.
Your doctor will tell you how to manage your meds before the procedure. It’s very important to follow these instructions to stay safe during the endoscopy.
Bowel Preparation for Lower GI Endoscopy
For lower GI procedures, like colonoscopies, you need to prepare your bowel well. This usually means changing your diet, using laxatives, and sometimes enemas. The goal is to make sure your colon is empty so your doctor can see everything clearly.
We’ll give you all the details on how to prepare your bowel. It’s very important to follow this prep closely for the best results.
What to Bring and Wear on Procedure Day
On the day of your procedure, bring important things with you. These include your insurance cards, a list of your meds, and someone to drive you home. Wear loose, comfy clothes and avoid jewelry or valuables.
Arriving ready will help make your procedure go smoothly. We’ll also give you specific instructions on what to expect, including arrival times and what to do after you’re discharged.
The Endoscopic Surgery Process: What to Expect
Getting ready for your endoscopic procedure can be easier if you know what to expect. Learning about the steps involved can reduce anxiety and make the experience smoother.
Pre-Procedure Preparation in the Facility
When you arrive at the facility, our staff will welcome you. They will help you with the preparation steps. This includes:
- Finishing any paperwork and checking your medical history.
- Wearing a hospital gown and removing jewelry or items that could get in the way.
- Getting an intravenous (IV) line for sedation and medication.
- Our team will explain the procedure, answer your questions, and talk about what happens during and after.
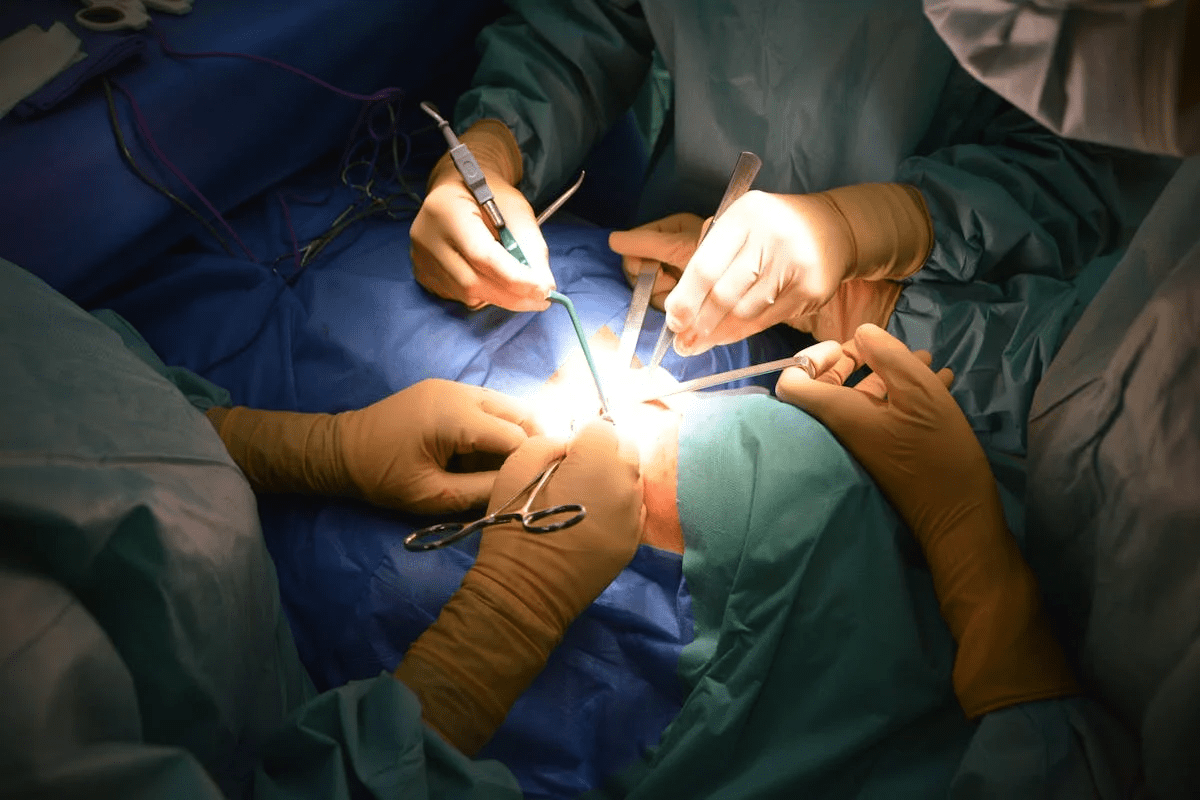
During the Procedure: Step by Step
The endoscopic procedure is closely watched and done with great care. Here’s what happens:
- First, sedation is given to help you relax.
- The endoscope is inserted through your mouth or rectum and guided to the needed area.
- Air or carbon dioxide is used to make the area clearer for viewing.
- The doctor looks at the internal structures on a monitor and checks for any issues.
- If needed, biopsies are taken or treatments are done.
Immediate Recovery Room Experience
After the procedure, you’ll go to the recovery room. Our staff will watch over you as the sedation fades. You can expect:
- Monitoring of your vital signs and overall health.
- Help with any discomfort or side effects, like bloating or soreness.
- Advice on what to do after the procedure, including what to eat and how active to be.
- A talk with your doctor about the results and what comes next.
Knowing these steps can help you feel more ready and confident for your endoscopic procedure.
Diagnostic Applications of Endoscopy
Endoscopy is a key tool in modern medicine. It lets us see inside the body without surgery. This helps us find and diagnose many health issues.
Conditions Commonly Diagnosed
Endoscopy is great for checking the stomach and intestines. It helps find problems like:
- Gastroesophageal reflux disease (GERD)
- Peptic ulcers
- Gastritis
- Celiac disease
- Colorectal cancer
Tissue Sampling and Biopsy Techniques
During an endoscopy, we can take tissue samples. This helps us check areas that look odd. We use special tools to get these samples, which are then looked at under a microscope.
Biopsy Technique | Description | Common Applications |
Forceps Biopsy | Using forceps to grasp and remove tissue | Suspected malignancies, ulcers |
Brush Biopsy | Using a brush to collect cells | Strictures, suspicious lesions |
Fine-needle Aspiration | Using a needle to aspirate cells or fluid | Cystic lesions, lymph nodes |
These methods are key for finding diseases like cancer and infections. The right method depends on where and what the problem is.
Endoscopy combines looking inside with taking tissue samples. This way, doctors can make accurate diagnoses and plan the best treatments.
Therapeutic Endoscopic Surgeries and Interventions
Therapeutic endoscopy has changed gastroenterology a lot. It offers many treatments that help patients a lot. We use endoscopy for both checking and treating stomach problems.
Polyp Removal and Cancer Prevention
Removing polyps is a big deal in endoscopy. It helps stop colorectal cancer. We find and take out polyps during a colonoscopy. This helps a lot in preventing cancer.
- Early detection and removal of precancerous polyps
- Reduced risk of colorectal cancer
- Minimally invasive procedure with quick recovery
Stricture Dilation and Stent Placement
Stricture dilation is another key use of endoscopy. We use balloons or dilators to make narrow parts of the gut wider. This helps with swallowing and digestion problems. Sometimes, we put in stents to keep things open.
Benefits of stricture dilation and stent placement include:
- Improved swallowing and digestion
- Relief from obstructive symptoms
- Avoidance of more invasive surgical procedures
Bleeding Control Techniques
Endoscopy helps control bleeding in the gut, which is very serious. We use cauterization, clips, or sclerosing agents to stop the bleeding. This helps keep the patient stable.
Effective bleeding control techniques are key for:
- Rapid stabilization of the patient
- Prevention of further complications
- Avoidance of blood transfusions
Stone Extraction Procedures
Stone extraction is another use of endoscopy, mainly for bile duct stones. We use sphincterotomy and balloon extraction to take out stones. This helps bile flow normally again.
Advantages of endoscopic stone extraction include:
- Minimally invasive approach
- Reduced risk of complications compared to surgery
- Quick recovery time
Potential Risks and Complications of Endoscopy
Endoscopy, like any medical procedure, has risks and complications. It’s generally safe, but knowing these can help patients prepare and understand what to expect.
Common Side Effects and Discomfort
Most people have endoscopy without big problems. But, some might feel minor side effects. These can include:
- Sore throat or discomfort
- Bloating or gas
- Mild abdominal pain
These side effects are usually short-lived and go away in a few hours to days.
Serious but Rare Complications
Though rare, serious complications can happen. These include:
- Perforation: A hole in the organ wall, needing surgery.
- Bleeding: Heavy bleeding that might need a blood transfusion or more procedures.
- Infection: Though rare, infections can happen if not done properly.
Doctors say, “The risk of serious complications is low, but knowing about them is important for patient safety and satisfaction.”
“The overall risk of complications from endoscopy is low, but being informed is key to patient safety and satisfaction.” –
Medical Expert
When to Seek Medical Attention Post-Procedure
After your endoscopy, watch your health closely. Seek medical help if you have:
- Severe abdominal pain
- Vomiting blood or black tarry stools
- Fever or chills
- Severe difficulty swallowing or breathing
If you’re worried or have these symptoms, call your healthcare provider right away.
Recovery After Endoscopic Surgery
After your endoscopic surgery, the recovery process is key. It helps you heal smoothly and without issues. Taking good care of yourself is important to avoid risks and support your body’s healing.
Immediate Post-Procedure Period
In the first hours after surgery, you’ll be watched closely in a recovery area. Medical staff will check your vital signs and help with any pain. This time is important to catch any immediate problems and keep you safe.
Key aspects of immediate post-procedure care include:
- Monitoring of vital signs
- Pain management
- Observation for any signs of complications
First 24 Hours After Endoscopy
The first 24 hours are critical for a good recovery. It’s important to follow certain guidelines to stay safe and comfortable.
Activity | Recommendation |
Rest | Avoid strenuous activities and rest as much as possible. |
Diet | Start with liquids and gradually move to soft foods as tolerated. |
Medication | Follow the medication instructions provided by your healthcare provider. |
Long-term Recovery Expectations
Recovery time can vary based on the procedure and your health. Most people can get back to normal in a few days to a week.
It’s important to follow your healthcare provider’s specific instructions regarding:
- Activity levels
- Dietary restrictions
- Follow-up appointments
Follow-up Care and Appointments
Follow-up care is essential for recovery. Going to scheduled appointments lets your healthcare provider check on your healing. They can also remove any sutures or clips if needed.
By following the recommended recovery guidelines, you can improve your healing. This helps reduce the risk of complications after endoscopic surgery.
Alternatives to Traditional Endoscopic Procedures
Patients now have many options beyond traditional endoscopy. These alternatives meet different needs, ranging from less invasive to more comfortable. They offer various ways to diagnose and treat conditions.
Non-Invasive Imaging Techniques
Modern non-invasive imaging is very advanced. It gives important information without needing to insert instruments into the body. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are examples. They help see inside the body without harm.
- MRI is great for soft tissue images.
- CT scans show detailed cross-sections.
Capsule Endoscopy Technology
Capsule endoscopy uses a small camera capsule swallowed. It takes pictures of the GI tract’s inside. This method is perfect for the small intestine, hard to reach with traditional endoscopy.
Feature | Capsule Endoscopy | Traditional Endoscopy |
Invasiveness | Non-invasive | Involves insertion of a scope |
Area of Examination | Primarily the small intestine | Accessible areas of the GI tract |
Patient Comfort | Generally more comfortable | May require sedation |
Virtual Endoscopy Options
Virtual endoscopy uses CT or MRI to create 3D models of organs. It allows for a virtual look inside. This method is less invasive and good for some diagnoses.
When Traditional Surgery May Be Necessary
Even with new methods, sometimes surgery is the best choice. Complex or urgent conditions often need a more direct approach.
- Severe bleeding that can’t be stopped by endoscopy.
- Complex polyps that can’t be removed endoscopically.
- Cancerous lesions needing surgery.
Knowing all options helps patients make better choices. We help patients find the best care for their needs and conditions.
Cost and Insurance Coverage for Endoscopy in the United States
Endoscopy costs can be a big worry for patients. Insurance coverage is key in managing these costs. It’s vital to understand the financial side of endoscopic procedures in today’s healthcare world.
Insurance Coverage Considerations
Insurance for endoscopy varies by provider and policy. Most plans cover these procedures if they’re needed. But, how much they cover can vary a lot.
It’s important to check your insurance policy:
- Deductibles and co-payments
- Out-of-pocket maximums
- Network providers vs. out-of-network providers
Questions to Ask Your Insurance Provider
Before getting an endoscopy, it’s key to know about your insurance. Here are some questions to ask:
- Is the procedure covered under my plan?
- What are the out-of-pocket costs for the procedure?
- Are there any pre-approval requirements?
- Can I use an out-of-network provider, and if so, what are the implications?
A healthcare expert says, “Knowing your insurance can really help with the cost of procedures like endoscopy.”
“Patients should not hesitate to ask questions about their coverage to avoid unexpected medical bills.”
Understanding endoscopy costs and insurance can help patients prepare financially. It’s wise to talk about these with your healthcare provider and insurance company. This way, you can have a smoother experience.
Choosing the Right Endoscopy Specialist and Facility
Finding a good endoscopy specialist and facility is key for a smooth procedure. This choice affects your experience, the success of the procedure, and your recovery.
Qualifications and Certifications to Look For
When picking an endoscopy specialist, look at their qualifications and certifications.
- Choose a gastroenterologist or surgeon who is board-certified.
- Make sure they have special training in endoscopy.
- Check their experience with your specific procedure.
Questions to Ask Before Scheduling
Before your procedure, write down questions for your specialist:
- What are the risks and benefits of my procedure?
- What prep do I need before the procedure?
- What sedation will be used, and why?
- How long will I recover, and what should I do after?
Endoscopy Centers vs. Hospital Settings
You might choose between an endoscopy center or a hospital for your procedure.
- Endoscopy centers offer a more personal experience and might be cheaper.
- Hospitals can handle more complex cases and emergencies.
Reading Patient Reviews and Outcomes
Reading patient reviews can give you insight into a specialist or facility’s quality. Look for feedback on:
- The staff’s professionalism and kindness
- The facility’s cleanliness and comfort
- The clarity of instructions before and after the procedure
“The care I received was top-notch. I was impressed by the expertise and kindness of my endoscopy specialist.”
By researching and asking the right questions, you can have a good experience and a successful procedure.
Conclusion: Making Informed Decisions About Your Endoscopic Care
As we wrap up our guide to endoscopic surgery, it’s clear that knowing what to expect is key. Understanding the details of endoscopic procedures helps you make choices that fit your health goals.
Endoscopic care is a complex field that needs teamwork between patients and doctors. Knowing about different procedures, the technology used, and sedation levels helps you prepare better.
We urge you to be active in your care. Ask questions, follow instructions, and talk about any worries with your doctor. Learning about your care is essential for a good outcome.
Choosing the right specialist and facility is important. Also, knowing your insurance helps ensure you get the best care. Your health journey is a partnership, and being informed is the first step to a successful experience.
FAQ
What is endoscopy?
Endoscopy is a medical test. It uses a flexible or rigid tube with a camera and light. This lets doctors see inside body cavities or organs.
Are you awake during endoscopic surgery?
Your level of awareness can vary. Some procedures use conscious sedation, making you relaxed but not asleep. Others might need general anesthesia, where you’re completely asleep.
What are the different types of endoscopic procedures?
There are many types. These include upper GI endoscopy (EGD), colonoscopy, bronchoscopy, and ERCP. Each has its own purpose.
How do I prepare for an endoscopic procedure?
You’ll need to follow some steps. This includes dietary restrictions and adjusting your medications. You might also need to prepare your bowel for certain procedures.
What can I expect during the endoscopic surgery process?
First, you’ll prepare for the procedure. Then, you’ll go through the procedure itself. After that, you’ll recover in a designated area. The details can vary.
What are the diagnostic applications of endoscopy?
Endoscopy helps diagnose many conditions. It lets doctors see inside organs and take tissue samples. This helps with diagnosis.
Can endoscopy be used for therapeutic purposes?
Yes, it can. Endoscopy is used for treatments like removing polyps and controlling bleeding. It offers a minimally invasive way to treat conditions.
What are the risks and complications of endoscopy?
While safe, endoscopy can have side effects and rare complications. It’s important to follow instructions and seek help if you have concerns.
How do I recover after endoscopic surgery?
Recovery has different stages. You’ll need to follow your doctor’s instructions closely. Attending follow-up appointments is also key.
Are there alternatives to traditional endoscopic procedures?
Yes, there are. Options include non-invasive imaging and capsule endoscopy. The right choice depends on your condition and health.
How much does endoscopy cost, and is it covered by insurance?
Costs vary widely. Many insurance plans cover endoscopy. It’s important to check with your provider about coverage and any costs you might have to pay.
How do I choose the right endoscopy specialist and facility?
Look for specialists with the right qualifications. Ask questions before scheduling. Consider the differences between centers and hospitals.
Is endoscopy considered a surgical procedure?
Endoscopy is a minimally invasive procedure. It’s less invasive than traditional surgery but requires proper care and preparation.
Will I be in pain during or after the endoscopy?
Most people feel little discomfort during the procedure. Afterward, any pain is usually mild and short-lived.
Can I drive myself home after an endoscopy?
It’s not recommended to drive yourself home, even if you’re not feeling pain. Make sure someone can drive you home safely.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31856567/