Last Updated on November 26, 2025 by Bilal Hasdemir
Endovascular coiling is a new way to treat brain aneurysms. It’s safer and more effective. This method fills the aneurysm with platinum coils. This helps it clot and prevents it from bursting.
At Liv Hospital, our experts use the latest technology for coil embolization. This is a less invasive option compared to open brain surgery. It’s a reliable choice for many patients.
This method lowers the risks of traditional surgery. It also means patients can recover faster. This makes it a great choice for people looking for top-notch care.
We’ll dive into the key points of this aneurysm treatment. You’ll learn about its benefits, how it’s done, and any risks involved.
Key Takeaways
- Endovascular coiling is a minimally invasive treatment for brain aneurysms.
- The procedure involves filling the aneurysm with platinum coils to promote clotting.
- Liv Hospital uses advanced neurointervention techniques and imaging technology.
- This approach reduces risks and ensures faster recovery times.
- Coil embolization is a reliable alternative to open brain surgery.
Brain Aneurysms: Understanding the Condition That Requires Treatment

It’s important to know about brain aneurysms to get help quickly. A brain aneurysm is a weak spot on an artery wall in the brain. It balloons out and fills with blood. If it bursts, it can cause bleeding in the brain, which is very dangerous.
What Exactly Is a Brain Aneurysm?
A brain aneurysm is a weak area in an artery in the brain. This weak spot can bulge out, creating a sac-like structure that fills with blood. Aneurysms can be dangerous because they can rupture, leading to a hemorrhagic stroke.
Risk Factors and Causes of Aneurysm Formation
Many things can make you more likely to get a brain aneurysm. These include genetic predisposition, smoking, high blood pressure, and certain medical conditions. Knowing these risk factors helps prevent and detect aneurysms early. For example, people with a family history of aneurysms should get checked.
Warning Signs and Symptoms of Aneurysm Rupture
The signs of a ruptured aneurysm come on fast and are very bad. You might feel a severe headache, nausea, vomiting, a stiff neck, and light sensitivity. Getting medical help right away is key if you notice these symptoms. Spotting these signs early can save your life.
Endovascular Coiling: The Revolutionary Minimally Invasive Treatment

Endovascular coiling is a new way to treat brain aneurysms. It’s less invasive than old surgery methods. This method uses tiny coils to fill the aneurysm, helping it clot and preventing it from bursting.
Definition and Basic Principles of the Procedure
Endovascular coiling, or coil embolization, uses platinum coils to treat aneurysms. These coils are put into the aneurysm through a leg artery. They help stop bleeding by forming a blood clot.
This treatment works by cutting off the aneurysm from the blood flow. It’s guided by high-tech imaging to place the coils exactly right.
The Science Behind How Coiling Prevents Aneurysm Rupture
Coiling works by making the aneurysm clot. The platinum coils inside the aneurysm help form a blood clot. This clot makes the aneurysm stable, lowering the chance of it bursting.
Also, the coils block blood flow into the aneurysm. This creates a place where clots can form and stay. This is key to stopping bleeding and helping the aneurysm heal.
Types of Coils and Materials Used in Treatment
There are different coils used in endovascular coiling:
- Platinum coils: These are safe for the body and help clotting.
- Bare platinum coils: These are the most used and work well at clotting.
- Coated coils: Some coils have extra materials to help clotting or prevent the aneurysm from opening again.
The right coil depends on the aneurysm’s size, shape, and where it is. New coil technologies are improving treatment results for patients.
The Step-by-Step Process of an Endovascular Coiling Procedure
The endovascular coiling procedure is a precise and advanced technique. We guide our patients through each step, making sure they are well-informed and ready for treatment.
Pre-Procedure Evaluation and Preparation
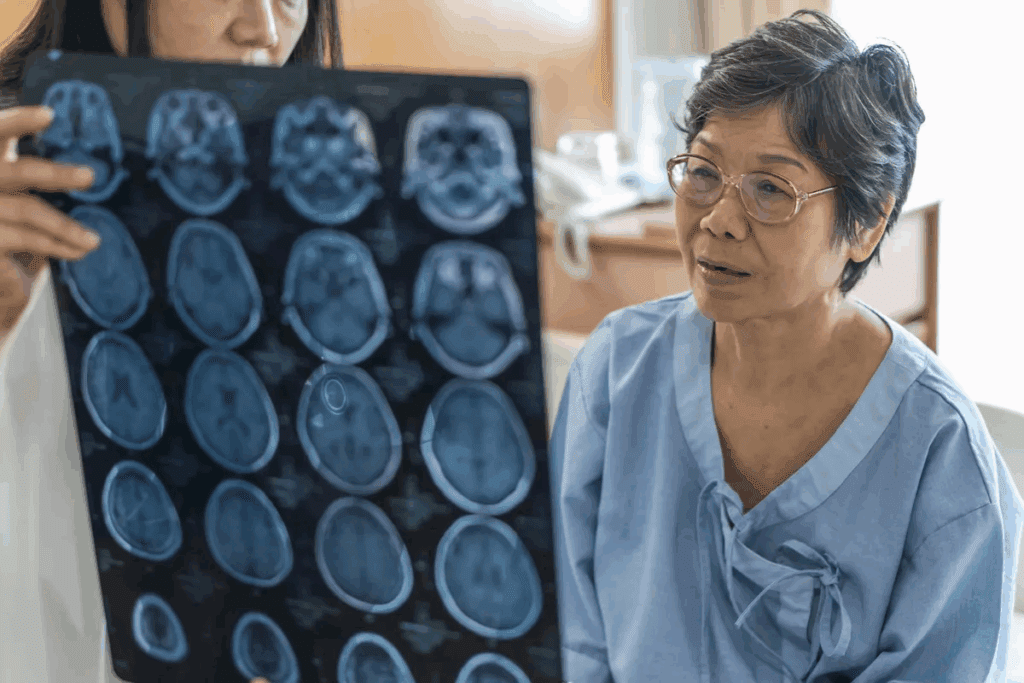
Before the procedure, patients get a detailed evaluation to see if they’re a good fit. This includes looking at their medical history, doing tests, and talking about any worries or questions. Preparation is key to a successful outcome, and our team makes sure every patient is ready.
Tests like angiograms or MRIs are key to understanding the aneurysm’s size, shape, and location. This info is vital for planning the coiling procedure, so we can tailor it to each patient’s needs.
During the Procedure: What Patients Can Expect
During the procedure, patients are given sedation to stay comfortable. A local anesthetic is applied to the area where the catheter is inserted, usually in the groin. The procedure happens in a special suite with top-notch imaging tech.
A catheter is carefully moved through the blood vessels to the aneurysm. Once there, platinum coils are put in to fill the aneurysm and stop blood flow. The whole thing is watched closely with advanced imaging.
Advanced Imaging Techniques That Guide Precise Coil Placement
Advanced imaging is key to the success of endovascular coiling. Fluoroscopy and 3D rotational angiography help guide the catheter and coils. These techs give real-time images, helping place the coils just right and lowering the risk of problems.
Using these advanced imaging methods makes sure the coils are in the right spot in the aneurysm. This boosts the treatment’s effectiveness and cuts down on the chance of it coming back.
Comparing Endovascular Coiling to Traditional Surgical Clipping
Endovascular coiling and surgical clipping are two ways to treat brain aneurysms. They both aim to stop the aneurysm from bursting. But, they use different methods and techniques.
Key Differences in Approach and Technique
Endovascular coiling is a less invasive method. Coils are inserted through a catheter to fill the aneurysm. This helps to stop blood flow into the aneurysm.
Surgical clipping, on the other hand, involves a craniotomy to place a titanium clip on the aneurysm. This clip isolates the aneurysm from blood flow.
A study in the Journal of Neurosurgery says the choice between these methods depends on the aneurysm’s size, location, and the patient’s health.
“The decision to use either endovascular coiling or surgical clipping should be made on a case-by-case basis, taking into consideration the specific characteristics of the aneurysm and the patient’s condition.”
Recovery Time and Hospital Stay Comparisons
Endovascular coiling is less invasive, leading to shorter recovery times and hospital stays. Patients often have less tissue damage and need less time in the hospital.
| Procedure | Average Recovery Time | Average Hospital Stay |
| Endovascular Coiling | 1-2 weeks | 2-3 days |
| Surgical Clipping | 4-6 weeks | 5-7 days |
How Doctors Determine Which Procedure Is Best for Each Patient
Doctors look at many factors to decide between endovascular coiling and surgical clipping. They consider the aneurysm’s size, shape, and location. They also think about the patient’s age, health, and medical history. Advanced imaging helps in making this decision.
By carefully looking at these factors, doctors can choose the best treatment for each patient. This ensures the best possible results.
Major Benefits That Make Endovascular Coiling a Preferred Option
Endovascular coiling is a new way to treat brain aneurysms. It has many benefits that make it a top choice for many. These include being minimally invasive, having a lower risk, and allowing for quicker recovery.
Reduced Physical Trauma and Minimal Scarring
Endovascular coiling is great because it causes less harm and scarring. Unlike old methods, it doesn’t need a big cut in the skull. This makes it safer and helps patients heal faster.
This method also means patients feel less pain and discomfort after. And, because there’s no big cut, there’s less scarring. This makes patients look better after treatment.
Lower Risk Profile for High-Risk and Elderly Patients
Endovascular coiling is good for people who are at high risk or are older. They might not be good candidates for old surgeries. This new method is safer and less risky.
- Reduced risk of procedural complications
- Lower risk of morbidity and mortality
- Ability to treat patients with complex aneurysms
This makes it possible to help more people. Even those who were thought to be too risky or not operable.
Faster Return to Normal Activities After Treatment
Endovascular coiling also means patients can get back to their lives faster. They usually don’t have to stay in the hospital as long. This means they can get back to work and daily life sooner.
The benefits of getting back to normal faster include:
- Reduced healthcare costs due to shorter hospital stays
- Less time away from work and daily activities
- Improved overall patient satisfaction
By cutting down on downtime, endovascular coiling makes the treatment better for patients.
Potential Risks and Complications to Be Aware Of
Endovascular coiling is a cutting-edge treatment for brain aneurysms. But, it’s important to know the possible risks. Like any medical procedure, there can be complications before and after treatment.
Immediate Procedure-Related Complications
Right away, there could be thromboembolic events. This means a blood clot might form and cause a stroke. There’s also a small chance of aneurysm rupture during the procedure. Other issues might include vascular injury, coil migration, and reactions to the contrast material used in imaging.
Long-Term Concerns: Recanalization and Rebleeding Rates
Long-term worries mainly focus on recanalization. This is when the aneurysm might reopen because the coil moves or gets pushed into the wall. This could lead to rebleeding. But, the risk of this happening is much lower after coiling. It’s key to have regular check-ups and imaging to watch for these problems.
How Doctors Mitigate and Manage These Risks
Doctors take steps to lower these risks. They use top-notch imaging during the procedure to place the coils accurately. Afterward, patients are watched closely for any signs of trouble. For ongoing worries, regular check-ups and scans are set up to spot issues early.
Advances in coil technology and materials also help improve results. By knowing these risks and complications, patients can make better choices about their treatment. It’s a team effort between the patient and their healthcare team to get the best results.
Determining If You’re an Ideal Candidate for Coiling Treatment
Choosing endovascular coiling as a treatment option needs careful thought. This procedure is not for everyone. A detailed check is needed to see if it’s right for you.
Doctors look at the aneurysm’s details and your health to decide. They aim to find the best treatment for you.
Aneurysm Characteristics: Size, Shape, and Location Considerations
The size, shape, and where the aneurysm is matter a lot. Small aneurysms with a narrow neck are best for coiling. The aneurysm’s shape and location also affect if coiling works well.
For example, aneurysms at the brain’s base or with complex shapes might not be good for coiling. In these cases, other treatments or a mix of treatments might be needed.
| Aneurysm Characteristic | Ideal for Coiling | Not Ideal for Coiling |
| Size | Small to medium | Large or giant |
| Shape | Spherical or oval with a narrow neck | Irregular shape or wide neck |
| Location | Accessible locations | Difficult-to-reach locations |
Patient-Specific Factors That Influence Treatment Decisions
Things like your health, past medical issues, and any other health problems matter a lot. People with serious health issues or at high risk for surgery might do better with coiling.
Also, your age, how well you’re doing neurologically, and if you’ve had treatments before are important. A team of doctors will look at all these to choose the best treatment for you.
“The decision to treat an unruptured aneurysm should be based on a careful assessment of the patient’s individual risk factors, the aneurysm’s characteristics, and the risks and benefits of the treatment options available.”
— American Heart Association
The Collaborative Decision-Making Process With Your Medical Team
Deciding on coiling is a team effort. You, your family, and doctors will talk about the options. They’ll discuss the good and bad of each choice and what you want.
A plan just for you will be made. It makes sure the treatment fits your needs and situation.
Post-Procedure Recovery and Long-Term Monitoring Protocol
Recovering from endovascular coiling needs a detailed plan. This includes care right after the procedure and ongoing checks. Knowing these steps helps ensure a smooth recovery.
Immediate Post-Procedure Care in the Hospital
After the procedure, patients stay in the hospital to watch for any problems. Close monitoring is key to catch and fix any issues quickly.
In the hospital, patients get medicine to ease any pain or issues. The medical team also teaches them about post-procedure care. This includes what activities to do, how to take medicine, and when to come back for more checks.
Follow-Up Imaging Schedule and Why It’s Critical
Follow-up imaging is a crucial part of the recovery plan. It lets doctors check if the coiling worked and if the aneurysm is stable. The usual schedule for these scans includes:
| Timeframe | Imaging Modality | Purpose |
| 6 months | Angiogram or MRA | Check if the aneurysm is closed and the coils are stable |
| 1 year | MRA or CTA | Watch for any signs of the aneurysm opening up again or coils moving |
| 2-5 years | MRA or CTA | Keep an eye on the aneurysm’s status over time |
As one expert says, “Regular scans are key to make sure the aneurysm stays closed and to spot any problems early.”
“The goal of follow-up imaging is to confirm that the aneurysm is completely occluded and that there are no signs of coil compaction or recanalization.”
Lifestyle Adjustments and Long-Term Prognosis
Patients also need to make lifestyle changes to help their recovery. This includes managing blood pressure, avoiding hard activities, and quitting smoking. These changes can greatly improve their long-term health.
In conclusion, recovery and ongoing checks are essential for endovascular coiling success. By following the recommended steps, patients can recover well and avoid complications.
Conclusion: Navigating Your Brain Aneurysm Treatment Journey
Brain aneurysm treatment has changed a lot with endovascular coiling. This method is less invasive and offers a new way to handle brain aneurysms. Knowing about endovascular coiling helps patients feel more in control of their treatment.
Choosing the right treatment is key, and a healthcare team can help with this. Endovascular coiling is a good choice for many, using coils to stop the aneurysm from bursting. It helps patients recover faster because of its precise method.
When starting treatment, it’s important to know the good and bad sides of endovascular coiling. Working with doctors helps make the best choice for each person. This way, patients can get the best results from their treatment.
Understanding endovascular coiling helps patients be more involved in their care. It leads to a treatment plan that’s more tailored to their needs.
FAQ
What is endovascular coiling, and how does it treat brain aneurysms?
Endovascular coiling is a minimally invasive procedure. It treats brain aneurysms by filling them with coils. This stops blood from entering and prevents rupture. Advanced imaging guides the precise placement of these coils.
What are the benefits of choosing endovascular coiling over surgical clipping?
Endovascular coiling has many benefits. It causes less physical trauma and leaves less scarring. Recovery is faster than with surgical clipping. It’s also safer for high-risk and elderly patients.
How do doctors determine if I’m a suitable candidate for endovascular coiling?
Doctors consider several factors to decide if you’re a good candidate. These include the aneurysm’s size, shape, and location. They also look at your overall health and medical history. Our team works with you to find the best treatment plan.
What are the possible risks and complications of endovascular coiling?
While safe, endovascular coiling has risks. These include immediate complications and long-term issues like recanalization and rebleeding. Our team takes steps to manage these risks.
What can I expect during the endovascular coiling procedure?
During the procedure, advanced imaging guides the coil placement. Patients are usually under sedation or anesthesia to reduce discomfort.
How long does it take to recover from endovascular coiling, and what follow-up care is required?
Recovery times vary, but most patients can resume normal activities in a few days. Follow-up imaging is key to check the aneurysm’s status. We provide personalized care guidance and follow-up schedules.
Can endovascular coiling prevent aneurysm rupture, and how effective is it?
Yes, endovascular coiling can prevent rupture by filling the aneurysm with coils. Success rates vary based on individual factors. Our team will discuss expected outcomes with you.
Are there any lifestyle adjustments I need to make after endovascular coiling?
After endovascular coiling, some lifestyle changes may be needed. Our team offers personalized guidance on care and lifestyle modifications.
What is the difference between conventional coiling, stent-assisted coiling, and balloon-assisted coiling?
These are different coiling techniques. Conventional coiling fills the aneurysm with coils. Stent-assisted coiling uses a stent to support the coils. Balloon-assisted coiling uses a balloon to place the coils. The choice depends on the aneurysm and patient factors.
How do aneurysm characteristics influence the decision to undergo endovascular coiling?
Aneurysm characteristics, like size and location, are key in deciding on endovascular coiling. Our team assesses these factors to choose the best treatment plan.
References:
- Molyneux, A. J., Kerr, R. S. C., Yu, L. M., Clarke, M., Sneade, M., Yarnold, J. A., Campbell, M. K., Rischmiller, J., Stratton, I. M., & Sandercock, P. (2015). International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2,143 patients with ruptured intracranial aneurysms: a randomized comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. The Lancet, 366(9488), 809–817.