Last Updated on December 1, 2025 by Bilal Hasdemir

Nearly 1 in 26 people in the United States will develop seizure disorders at some point. For some, surgical intervention is a necessary treatment option Epilepsy surgery.
The time it takes for epilepsy surgery can vary a lot. This depends on the type of procedure and the patient’s condition. Usually, these surgeries can last from a few hours to a whole day.
The complexity of the case and the surgical team’s experience are key. Knowing these factors helps patients and their families get ready for the surgery and recovery.
Key Takeaways
- The duration of epilepsy surgery varies based on the procedure type.
- Surgical complexity and team experience influence the surgery length.
- Seizure treatment surgery can last from a few hours to a full day.
- Understanding the factors that influence surgery duration can aid in preparation.
- Patients and families should be prepared for the procedure and recovery.
What is Epilepsy Surgery and Who Needs It
For those with drug-resistant epilepsy, surgery is a possible solution. It’s considered when medicines don’t work, affecting their quality of life.
Definition and Purpose of Surgical Intervention
Epilepsy surgery is a surgical intervention to reduce or stop seizures. Its main goal is to improve a patient’s quality of life. This is done by reducing seizures, allowing them to live more normally.
Candidates for Epilepsy Surgery
Not everyone with epilepsy can have surgery. The choice to have epilepsy surgery depends on a detailed evaluation. This includes how severe the seizures are and their impact on the patient’s life.
Drug-Resistant Epilepsy Criteria
Those with drug-resistant epilepsy might be considered for surgery. This means their seizures can’t be controlled with medication. They need other treatments.
Quality of Life Considerations
The benefits of epilepsy surgery on a patient’s quality of life are big. It can lead to better thinking, more independence, and a more active life.
.
Types of Epilepsy Surgery Procedures
Epilepsy surgery has evolved to include many procedures. Each one is tailored to meet the needs of patients. These surgeries aim to help those with drug-resistant epilepsy.
Resective Surgery Options
Resective surgery removes the brain part where seizures start. It’s considered when the seizure focus is clear and can be safely removed.
Temporal Lobe Resection
Temporal lobe resection is common. It’s for patients with seizures in the temporal lobe. This surgery often greatly reduces or stops seizures.
Extratemporal Resections
Extratemporal resections remove seizure foci outside the temporal lobe. These surgeries are complex. They require brain function mapping to avoid damage.
Disconnection Procedures
Disconnection procedures stop seizures from spreading. They’re for patients who can’t have resective surgery.
Corpus Callosotomy
Corpus callosotomy cuts or clamps the corpus callosum. It’s used for drop attacks in some epilepsy cases.
Hemispherectomy
Hemispherectomy removes or disconnects one brain half. It’s for severe epilepsy affecting one hemisphere.
Neuromodulation Techniques
Neuromodulation changes brain activity to reduce seizures. It’s used when other surgeries aren’t right.
Vagus Nerve Stimulation
Vagus nerve stimulation implants a device that sends electrical impulses. It can lower seizure frequency in some.
Responsive Neurostimulation
Responsive neurostimulation implants electrodes in the seizure focus. It detects abnormal activity and stops seizures.
These surgeries offer hope for those with drug-resistant epilepsy. The right procedure depends on the seizure focus and the patient’s health.
Duration of Different Epilepsy Surgery Types
Epilepsy surgeries vary in how they’re done and how long they take. The time needed depends on the surgery type, how complex the case is, and if tests are done during surgery.
Standard Resections (2-4 hours)
Standard resections, like those in the temporal lobe, are common. They usually last 2 to 4 hours. This is because the focus of the epilepsy is clear and the surgery is straightforward.
Complex Resections (4-6 hours)
Complex resections need more detailed work and take longer, from 4 to 6 hours. They might cover more brain areas or have complex structures, needing careful planning.
Hemispherectomy and Major Disconnections (5-8 hours)
Hemispherectomy and major disconnections are bigger and take longer, often 5 to 8 hours or more. These surgeries remove or disconnect big parts of the brain, needing precise and careful work.
Minimally Invasive Procedures (1-3 hours)
Minimally invasive methods, like Laser Interstitial Thermal Therapy (LITT) and Stereotactic Procedures, are quicker. They last from 1 to 3 hours. These use advanced tech to target the focus with less damage and quicker recovery.
Laser Interstitial Thermal Therapy (LITT)
LITT uses laser heat to kill the focus. It’s done under MRI, allowing for precise and less damage to nearby tissue.
Stereotactic Procedures
Stereotactic procedures use a frame to locate and treat the focus. They are very accurate and can fit the patient’s anatomy.
| Surgery Type | Typical Duration | Key Characteristics |
| Standard Resections | 2-4 hours | Common, well-defined epileptic focus |
| Complex Resections | 4-6 hours | Involves multiple brain areas or complex anatomy |
| Hemispherectomy and Major Disconnections | 5-8 hours | Extensive, involves disconnecting or removing large brain portions |
| Minimally Invasive Procedures | 1-3 hours | Less intrusive, uses advanced technology for precision |
The time needed for epilepsy surgery is key in planning. Knowing how long each surgery takes helps prepare the patient and the team for what’s ahead.
The Multidisciplinary Approach to Epilepsy Surgery
Epilepsy surgery is a team effort. It involves many medical experts. Success depends on a multidisciplinary approach. This means experts from different fields work together to plan and do the surgery.
The Epilepsy Surgery Working Group
The epilepsy surgery working group includes many specialists. These are epileptologists, neurologists, neurosurgeons, and more. Each one is key in checking the patient, planning the surgery, and doing it.
Role of Different Specialists
The team has many specialists. Each one brings their own skills to the surgery.
Epileptologists and Neurologists
Epileptologists and neurologists are vital. They help find out what’s wrong and if surgery is right. They do tests, read the results, and decide if surgery is needed.
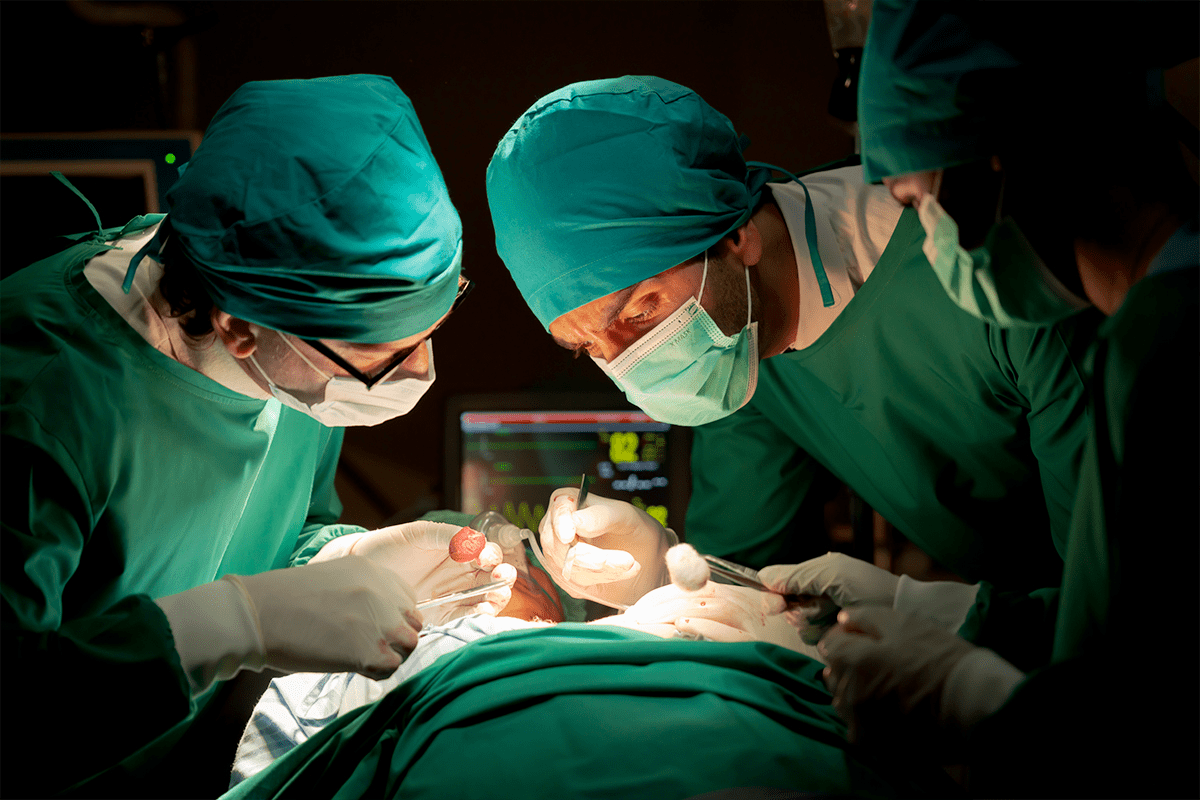
Neurosurgeons and Support Staff
Neurosurgeons do the surgery. Nurses and technicians help a lot before, during, and after.
Collaborative Surgical Planning
Planning the surgery is a team effort. The whole neurosurgical team works together. This makes sure everything is thought of, leading to a better and safer surgery.
The multidisciplinary approach to epilepsy surgery improves care. It makes sure all important things are considered. This teamwork is key to the best surgical results.
Pre-Surgical Evaluation and Planning Timeline
The journey to epilepsy surgery starts with a detailed pre-surgical evaluation and planning timeline. This phase includes many tests to see if surgery is right for a patient. It also helps plan the surgery.
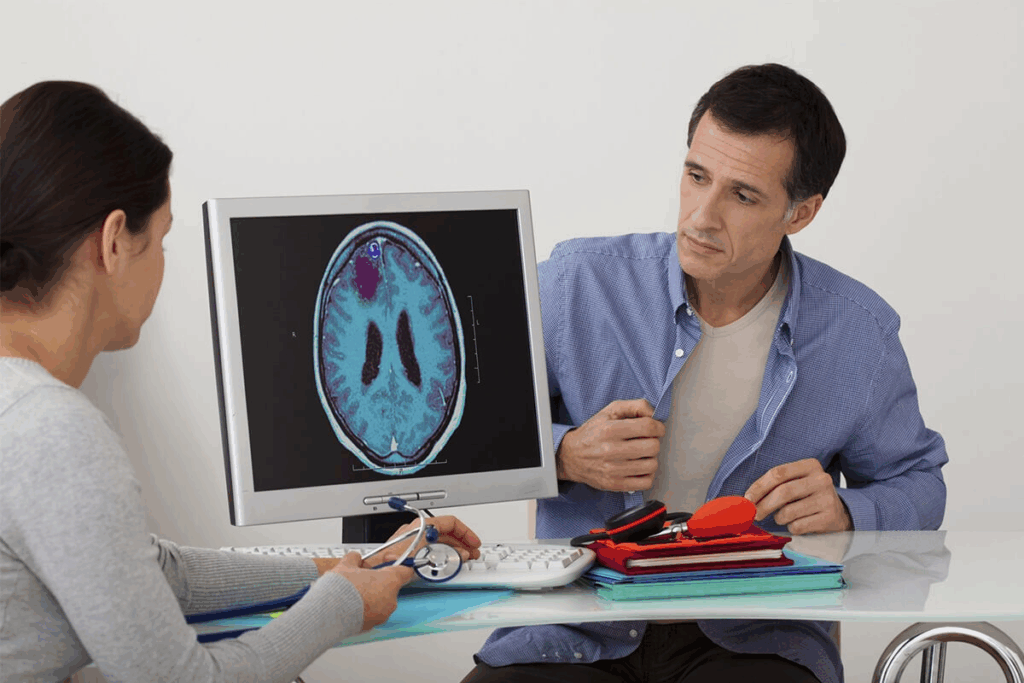
Non-Invasive Diagnostic Tests
Non-invasive tests are key in the early stages. They find the seizure focus and check brain function without surgery.
MRI, EEG, and PET Scans
MRI (Magnetic Resonance Imaging), EEG (Electroencephalogram), and PET (Positron Emission Tomography) scans are used. MRI shows brain structure, EEG records brain activity, and PET scans check brain function and metabolism.
Neuropsychological Testing
Neuropsychological testing is also important. It checks memory, language, and problem-solving skills. This helps predict how well a patient will do after surgery and finds any concerns.
Invasive Monitoring When Necessary
Sometimes, invasive monitoring is needed to find the seizure focus. This means putting electrodes in or on the brain to record activity directly.
Stereo-EEG and Grid Placement
Stereo-EEG and grid placement are used for detailed brain activity monitoring. Stereo-EEG puts electrodes deep in the brain, and grid placement places them on the brain’s surface.
Duration of Monitoring
Invasive monitoring lasts from 5 to 14 days. This time is needed to gather enough data to pinpoint the seizure focus.
Epileptic Focus Localization Process
The epileptic focus localization process is key for successful surgery. It uses data from tests to find the seizure area in the brain.
Knowing exactly where the seizures start helps neurosurgeons plan a precise surgery. This increases the chance of success and reduces risks for the patient.
Brain Function Mapping Techniques
Electrical Stimulation Mapping
This method uses electrical stimulation on the brain’s surface. It helps find areas for important functions like movement, language, and feeling. This way, surgeons can avoid harming these areas during surgery.
Time Required for Accurate Mapping
The time needed for brain mapping varies. It depends on the case’s complexity and the methods used. Usually, it takes several hours. This is because it involves careful stimulation and recording.
| Mapping Technique | Time Required | Precision Level |
| Electrical Stimulation Mapping | 2-4 hours | High |
| Functional MRI Integration | 1-2 hours | Very High |
Awake Brain Surgery vs. General Anesthesia
It’s important to know the difference between awake brain surgery and general anesthesia for epilepsy surgery. The choice depends on the surgery’s needs and the patient’s health.
When Awake Surgery is Necessary
Awake brain surgery is needed when intraoperative testing of language and motor functions is required. This method lets surgeons check the patient’s brain functions in real-time. It helps them avoid harming important brain areas.
Language and Motor Function Testing
During awake surgery, patients do tasks to test their language and motor skills. This helps surgeons find and avoid brain areas that control these functions.
Patient Selection Criteria
Choosing patients for awake surgery depends on their ability to cooperate. The patient’s health and the surgery’s complexity also play a role.
The Awake Surgery Process
The awake surgery process is carefully planned and executed. Intraoperative testing duration changes based on the surgery’s complexity and the patient’s response.
Intraoperative Testing Duration
Intraoperative testing can last from a few minutes to hours. It depends on the surgery’s needs and the patient’s response.
Patient Experience During Awake Surgery
Patients may feel discomfort or anxiety during awake surgery. But, medical staff helps them manage these feelings.
General Anesthesia in Epilepsy Surgery
General anesthesia is used for surgeries where intraoperative testing is not necessary. It allows for more complex surgeries, as the patient is completely asleep.
Types of Procedures Performed Under General Anesthesia
General anesthesia is used for complex epilepsy surgeries like hemispherectomy or major disconnections.
Monitoring Brain Activity During Anesthesia
It’s vital to monitor brain activity during general anesthesia. This ensures the patient’s safety and the surgery’s success. Techniques like EEG and neuromonitoring are used for this.
Choosing the right anesthesia approach helps surgeons achieve better results in epilepsy surgery. This improves the patient’s quality of life.
Surgical Day Timeline and Process
The day of epilepsy surgery has many important stages, from getting ready to recovering. Knowing about these steps helps patients and their families get ready for the surgery and the time in the hospital.
Pre-Operative Preparation (2-3 hours)
Getting ready for surgery is a key part that takes 2 to 3 hours. This includes:
Anesthesia Preparation
The team that handles anesthesia makes sure the patient is comfortable and pain-free during the surgery.
Surgical Site Preparation
The area where the surgery will happen is cleaned and made sterile. This is to lower the chance of infection.
The Actual Surgical Procedure (2-8 hours)
The surgery can last from 2 to 8 hours. This depends on how complex the case is.
Craniotomy and Access
The surgery starts with a craniotomy. This is when the neurosurgeon takes out a part of the skull to get to the brain.
Resection or Implantation Phase
Next, the surgeon removes the part of the brain causing seizures or puts in a device to help control seizures.
Closure and Completion
After finishing the surgery, the surgeon closes the hole in the skull. They might put the bone flap back.
Immediate Post-Operative Recovery (2-4 hours)
Right after surgery, the patient is watched for 2 to 4 hours. This is to catch any problems or bad reactions.
| Stage | Duration | Description |
| Pre-operative Preparation | 2-3 hours | Getting ready for surgery, including anesthesia and preparing the surgical site. |
| Surgical Procedure | 2-8 hours | The actual surgery, including opening the skull, removing or implanting, and closing. |
| Post-operative Recovery | 2-4 hours | Watching the patient after surgery for any problems or bad reactions. |
Knowing about the surgical day timeline and process can make some of the anxiety about epilepsy surgery less. By understanding what to expect, patients can prepare better for the surgery and the recovery that follows.
Hospital Stay and Recovery Duration
The time you spend in the hospital after epilepsy surgery depends on several things. These include the surgery type, its complexity, and your health.
Typical Length of Hospital Stay
Most patients stay 1 to 2 days in the Intensive Care Unit (ICU). Then, they move to a regular ward for more recovery time.
ICU Duration (1-2 days)
The ICU is where your immediate post-surgery health is closely watched. It’s also where pain management and complication prevention happen.
Regular Ward Recovery (3-7 days)
Once out of the ICU, you’ll stay in a regular ward. Here, your overall health and brain function are monitored.
Factors Affecting Hospital Stay Duration
Several things can change how long you stay in the hospital. These include:
- Surgery Type and Complexity: More complex surgeries often mean longer stays.
- Patient Age and Health Status: Older patients or those with health issues may need more time to heal.
Postoperative Care in Epilepsy Surgery
Postoperative care is key. It involves managing medications, watching for complications, and ensuring a smooth recovery.
Medication Management
You’ll be given meds to control pain, prevent seizures, and lower infection risk.
Monitoring for Complications
Doctors and nurses will keep a close eye on you for any signs of problems. This includes infections, neurological issues, or bad reactions to meds.
Rehabilitation after brain surgery is also vital. It helps you regain strength and brain function.
Conclusion
Epilepsy surgery is a key treatment for those with drug-resistant epilepsy. Its success relies on finding the right seizure focus and the chosen surgery type.
A well-thought-out epilepsy surgery can greatly reduce or stop seizures. This leads to a life without seizures. After surgery, careful care and ongoing monitoring are vital for the best results.
Understanding epilepsy surgery’s complexities helps patients and families make smart choices. Long-term monitoring after surgery is key to achieving the best outcomes.
FAQ
What is epilepsy surgery?
Epilepsy surgery is a treatment for seizures that don’t respond to medicine. It includes surgeries like resective surgery and neuromodulation. These aim to reduce or stop seizures.
Who is a candidate for epilepsy surgery?
People with drug-resistant epilepsy might be candidates. They must meet certain criteria. The decision to have surgery depends on how severe their seizures are and how they affect their life.
How long does epilepsy surgery typically last?
Surgery time varies. It can be a few hours or a full day. Simple surgeries usually take 2 to 4 hours. More complex ones can take longer.
What is the difference between awake brain surgery and general anesthesia in epilepsy surgery?
Awake surgery is for tests during the procedure. General anesthesia is used when tests aren’t needed. The choice depends on the patient’s ability to cooperate.
How long is the hospital stay following epilepsy surgery?
Stay time varies. It depends on the surgery type and the patient’s health. Usually, patients spend 1 to 2 days in ICU and 3 to 7 days in a regular ward.
What is the role of the multidisciplinary team in epilepsy surgery?
The team includes doctors and support staff. They evaluate patients, plan surgeries, and perform them. Each member is vital to the process.
What are the different types of epilepsy surgery procedures?
There are many procedures, like resective surgery and neuromodulation. Techniques like vagus nerve stimulation are used to manage seizures.
How is the seizure focus localized before epilepsy surgery?
Tests like MRI and EEG are used to find the seizure source. Sometimes, invasive monitoring is needed for precise location.
What is the importance of brain function mapping in epilepsy surgery?
Mapping is key to preserving brain areas. Techniques like electrical stimulation help locate seizure sources without harming brain functions.
What is the typical recovery process after epilepsy surgery?
Recovery starts with 2 to 4 hours of monitoring. Postoperative care manages medications and watches for complications. Rehabilitation is also important for a full recovery.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra1600646