Last Updated on December 1, 2025 by Bilal Hasdemir

Nearly 1 in 3 people with epilepsy have uncontrolled seizures despite trying many treatments. For these individuals, epilepsy surgery may offer a chance to significantly reduce seizure frequency. It can also improve their quality of life.Who is eligible for Epilepsy surgery? Our essential guide reveals the critical criteria for candidates and the hopeful, life-changing benefits.
Drug-resistant epilepsy is a condition where seizures persist despite adequate trials of two or more anti-seizure medications. For people living with this condition, epilepsy surgery can be a viable treatment option. This is when seizures originate from a single area in the brain.
Key Takeaways
- Epilepsy surgery is considered for individuals with uncontrolled seizures.
- Drug-resistant epilepsy is a key indicator for surgical eligibility.
- The surgery is most effective when seizures occur in a single brain area.
- Seizure frequency can be significantly reduced through surgical intervention.
- Improving quality of life is a primary goal of epilepsy surgery.
Understanding Epilepsy and When Surgery is Considered
Living with epilepsy means facing a daily battle to manage seizures. This can greatly affect a person’s life. Epilepsy is a brain disorder that causes seizures. These are sudden electrical activity in the brain.
If medication doesn’t work, other treatments like surgery are considered. This is a big decision for both patients and doctors.
The Impact of Uncontrolled Seizures
Seizures that can’t be controlled pose serious risks. Physical injuries, drowning, and even sudden death are possible. Seizures can also affect a person’s mental health.
They can lead to depression, anxiety, and developmental delays in kids. Here are some complications of uncontrolled seizures:
| Complication | Description | Impact |
| Physical Injuries | Injuries sustained during a seizure | Immediate physical harm |
| Drowning | Seizure occurring in water | Risk of drowning |
| Developmental Delays | Impact on children’s development | Long-term cognitive and behavioral effects |
Defining Drug-Resistant Epilepsy
Drug-resistant epilepsy, or refractory epilepsy, is when seizures don’t stop with medication. It’s when two or more anti-seizure drugs don’t work. People with this condition might need surgery to help control their seizures.
Primary Candidates for Epilepsy Surgery
People with focal seizures that don’t respond to medication might be good for epilepsy surgery. Focal seizures start in one part of the brain. To qualify, seizures must start in a specific, safe area that can be removed or changed without harming the brain.
Patients with Focal Seizures
Those with focal seizures are often considered for surgery. These seizures start in a specific brain area. Surgery might stop or lessen these seizures.
Patients with Identifiable Seizure Focus
Having an identifiable seizure focus is key for surgery. Tests like MRI and EEG help find if the seizure start is clear and safe for surgery.
“The ability to identify the seizure focus is critical for determining suitability for epilepsy surgery.”
Pediatric Candidates
Kids with drug-resistant epilepsy might also get surgery. Doctors carefully weigh the surgery’s benefits and risks. They consider how it might affect the child’s growth and life quality.
| Candidate Group | Key Characteristics |
| Patients with Focal Seizures | Seizures originate in one part of the brain |
| Patients with Identifiable Seizure Focus | Seizure origin is localized and identifiable |
| Pediatric Candidates | Drug-resistant epilepsy, significant surgery benefits |
The Complete Evaluation Process
A thorough evaluation is key in the epilepsy surgery process. It involves many tests to see if surgery is right for a patient.
This process happens at a special epilepsy center. A team of experts works together to check the patient’s condition.
Neurological Assessment
A detailed neurological assessment is done. It checks the brain’s function and looks for surgery risks.
This includes a full medical history, physical check-up, and tests of brain function. It helps understand the patient’s brain health.
Imaging Studies (MRI, PET, SPECT)
Imaging studies are vital in this process. They help find the seizure’s source and how it affects the brain.
MRI, PET, and SPECT scans give clear brain images. They help doctors plan the surgery.
- MRI shows detailed brain anatomy.
- PET scans spot brain metabolism changes.
- SPECT scans check brain blood flow.
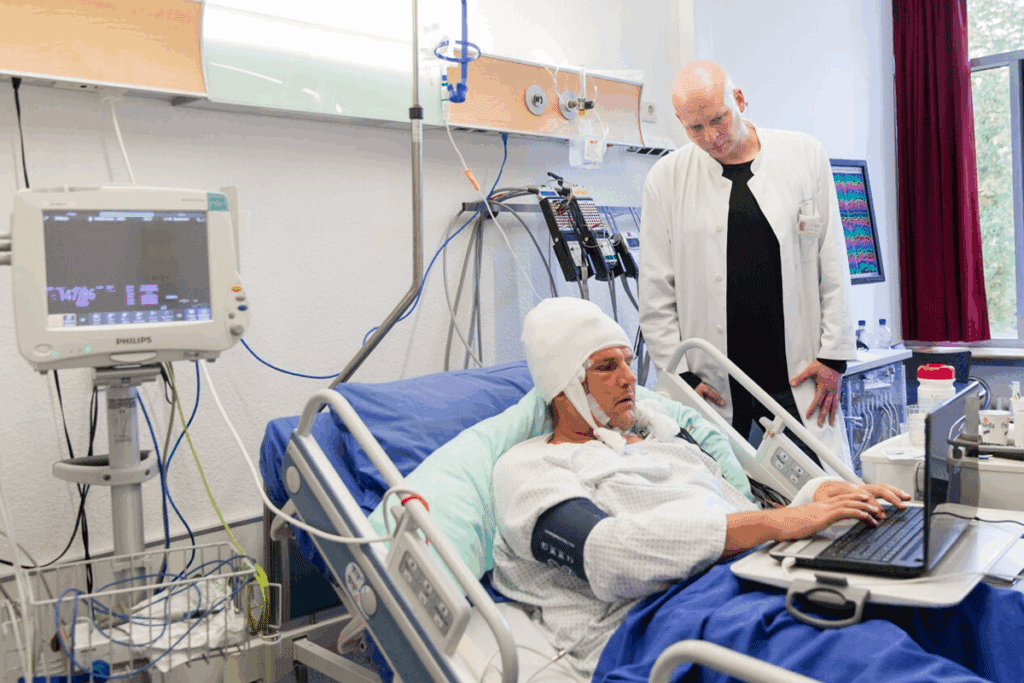
EEG Monitoring and Video Telemetry
EEG monitoring and video telemetry are key tools. They record seizures and link them to brain activity.
This info is key to finding the seizure source. It helps decide if surgery is a good option.
Together, EEG and video telemetry give a full picture of seizure patterns.
Advanced Diagnostic Techniques
Advanced diagnostic techniques are key in checking if a patient is right for epilepsy surgery. They help doctors find where seizures start and how the brain works.
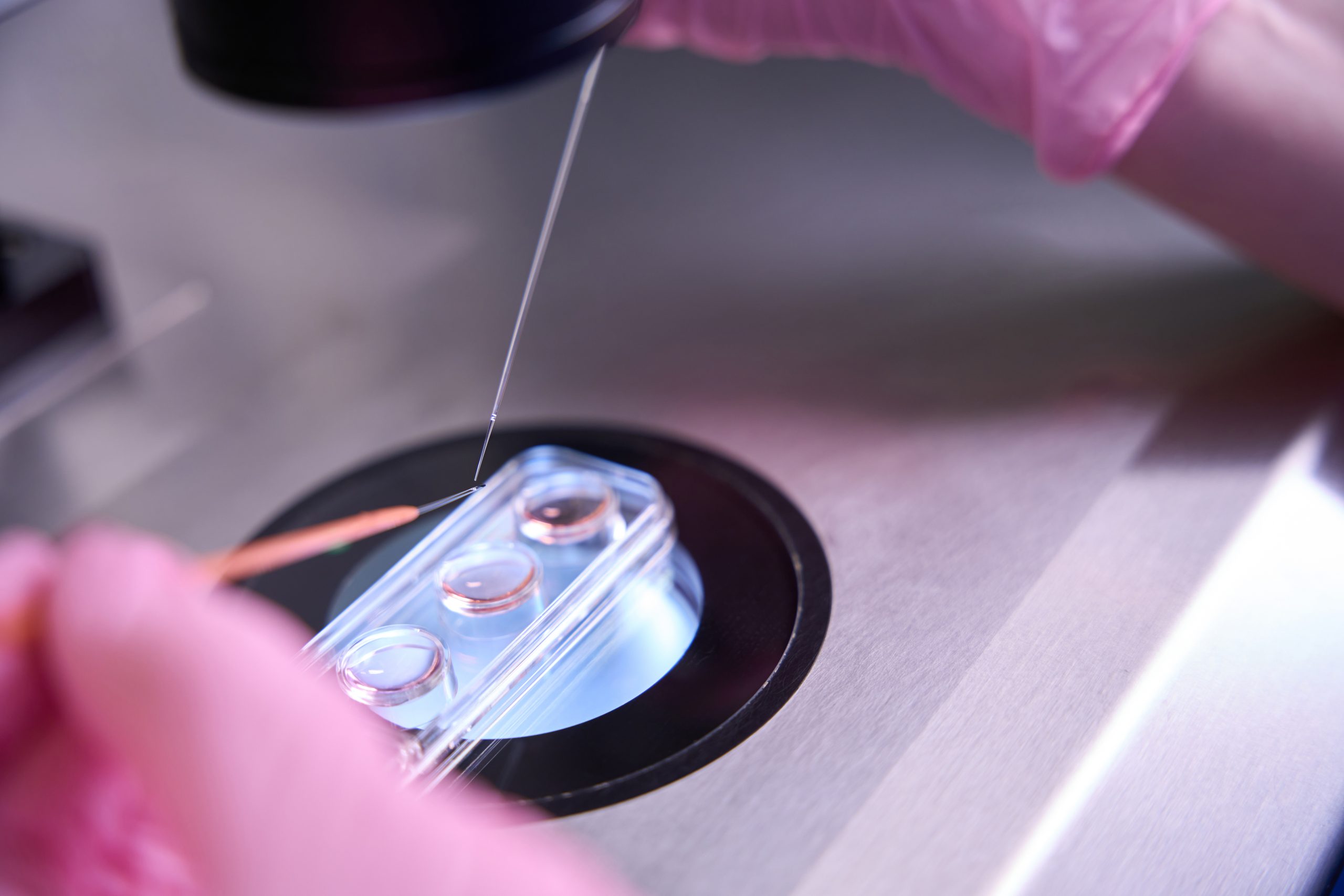
Functional MRI and Brain Mapping
Functional MRI (fMRI) is a big help in checking patients. It shows which parts of the brain are active when doing certain things. This is important for seeing how seizures relate to important brain areas.
Brain mapping uses tiny electrodes to measure electrical signals in the brain. It helps find where seizures start and how close it is to important brain parts.
fMRI and brain mapping together give a full picture of brain function and seizure activity. This helps doctors plan surgery better, which can lead to better results for patients.
| Diagnostic Technique | Purpose | Benefits |
| Functional MRI | Identify brain activity areas | Precise localization of seizure focus |
| Brain Mapping | Measure electrical activity | Delineates seizure onset zone |
| Invasive EEG Monitoring | Record seizures directly | Accurate diagnosis and localization |
Invasive EEG Monitoring
Invasive EEG monitoring puts electrodes right into the brain to catch seizure activity. It’s very useful when other methods don’t work. It gives detailed info on where seizures start, which is key for surgery planning.
Techniques like laser interstitial thermal therapy (LITT) are also options. They are less invasive and might be used in some cases.
The info from these advanced tests is vital for deciding if a patient can have epilepsy surgery. It also helps plan the best surgery approach.
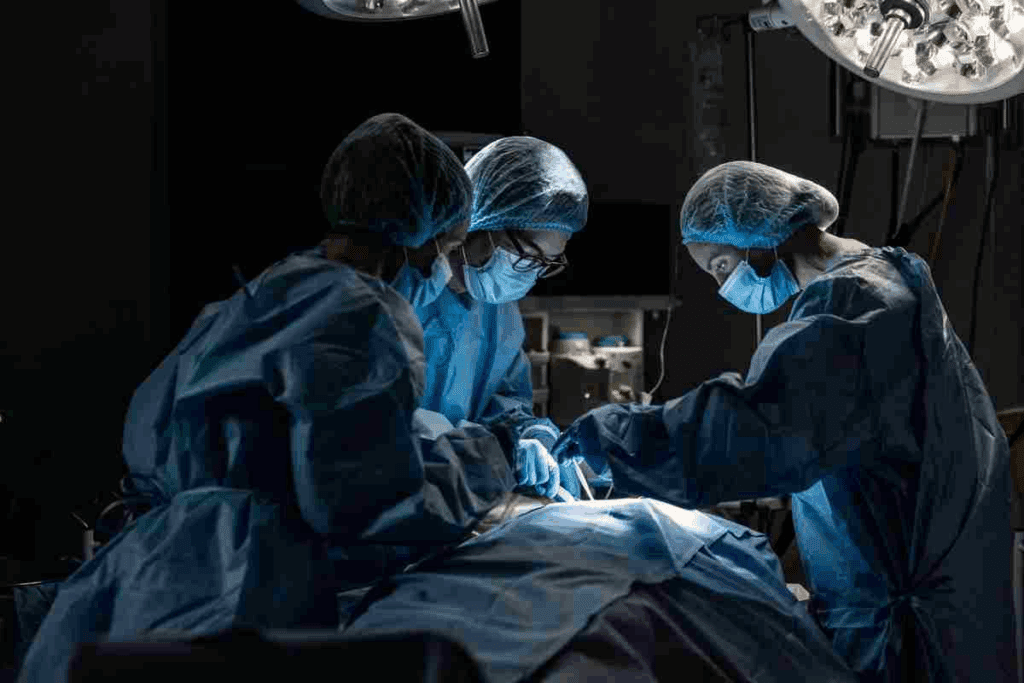
Types of Epilepsy Surgery Procedures
Epilepsy surgery offers many options for those with drug-resistant seizures. The right procedure depends on several factors. These include the seizure’s location, the patient’s health, and the surgery’s benefits and risks.
Resective Surgeries
Resective surgery removes the brain area where seizures start. It’s chosen when the seizure focus is in one spot and can be safely taken out without harming the brain too much.
Temporal Lobe Resection
Temporal lobe resection is a common surgery for temporal lobe epilepsy. It removes the part of the temporal lobe where seizures begin.
Other Lobe Resections
Other surgeries target different brain lobes. These include frontal lobe resection, parietal lobe resection, and occipital lobe resection. Each surgery aims at the specific lobe where seizures start.
Disconnection Procedures
Disconnection procedures aim to stop abnormal electrical pathways in the brain. They don’t remove the seizure focus itself.
Corpus Callosotomy
Corpus callosotomy involves cutting or partially sectioning the corpus callosum. This major brain connection is severed to treat generalized seizures that meds can’t control.
Hemispherotomy
Hemispherotomy is a more complex procedure. It disconnects or removes one brain hemisphere. It’s for patients with severe, one-sided seizure onset.
Minimally Invasive Approaches
Minimally invasive surgeries are newer options. They offer less risk and quicker recovery times compared to traditional surgeries.
Laser Interstitial Thermal Therapy (LITT)
Laser interstitial thermal therapy (LITT) uses laser heat to destroy the seizure focus. It’s guided by MRI for precision.
Stereotactic Radiosurgery
Stereotactic radiosurgery uses high radiation doses to reduce or stop seizures over time. It’s non-invasive and good for hard-to-reach targets.
Each epilepsy surgery has its own benefits and risks. The right surgery depends on a detailed evaluation and discussion with the patient and their healthcare team.
Neurostimulation Options for Epilepsy
Neurostimulation is a new way to treat epilepsy when medicines don’t work. It uses devices that send electrical signals to the brain. The goal is to cut down on seizures.
Vagus Nerve Stimulation (VNS)
Vagus Nerve Stimulation (VNS) is a well-known treatment for epilepsy. A device is implanted to send electrical signals to the vagus nerve. It can help lower seizure frequency in some people, mainly those with hard-to-treat epilepsy.
- Implantable device that delivers electrical impulses to the vagus nerve
- Can reduce seizure frequency in some patients
- Suitable for patients with drug-resistant epilepsy
Responsive Neurostimulation (RNS)
Responsive Neurostimulation (RNS) is a more advanced therapy. It involves putting a device right into the brain. This device watches for abnormal brain activity and stops seizures with electrical signals.
- Directly implanted into the seizure focus in the brain
- Detects and responds to abnormal electrical activity
- Can be adjusted post-implantation to optimize seizure control
Deep Brain Stimulation (DBS)
Deep Brain Stimulation (DBS) involves putting electrodes in certain brain spots. For epilepsy, it targets areas thought to cause seizures. It has shown to reduce seizures in some studies.
- Targets specific brain areas involved in seizure generation
- Can be adjusted to optimize therapeutic benefit
- Shows promise in lowering seizure frequency
These treatments offer hope for those with epilepsy who haven’t found relief with medicines. Each has its own benefits and things to consider. Choosing the right treatment should be done with a doctor’s advice.
Factors That May Disqualify Candidates
Epilepsy surgery can change lives, but some conditions might stop people from getting it. The choice to have surgery depends on many factors.
Multiple Seizure Foci
Having multiple seizure foci is a big issue. Seizures from different brain areas make it hard to find one spot for surgery. This raises the chance of seizures continuing after surgery.
Seizure Origin in Critical Brain Areas
Seizures in critical brain areas are a big problem. These areas handle important tasks like speech and movement. Surgery here could lead to serious problems, so the risks must be weighed carefully.
Medical Comorbidities
Having medical comorbidities can also affect surgery eligibility. Issues like heart disease or diabetes can make surgery riskier. It’s important to check a person’s health before surgery.
Knowing these factors helps decide if surgery is right. Doctors look at each case carefully. They aim to improve quality of life for those with epilepsy, balancing risks and benefits.
- Multiple seizure foci complicate surgical targeting.
- Seizures in critical brain areas risk neurological deficits.
- Significant medical comorbidities increase surgical risks.
Preparing for Epilepsy Surgery and Recovery
The path to epilepsy surgery is filled with steps to get ready. It’s key to work with your healthcare team. This ensures you’re ready for the surgery and the recovery that comes next.
Pre-Surgical Preparation
Getting ready for surgery is a big step. It includes tests and checks to see if surgery is right for you. Neurological tests, MRI scans, and EEG monitoring are part of this. Also, talk to your doctor about your medicines. Some might need to change or stop before surgery.
Hospital Stay Expectations
How long you stay in the hospital after surgery varies. It depends on the surgery and your health. Usually, it’s a few days to start recovering. The team will watch you closely and help with any pain or issues.
Long-Term Recovery and Follow-Up
Recovering from surgery takes time. You’ll see your healthcare team often to check on you. It’s important to follow their advice and tell them about any changes. It might take weeks or months to get back to normal.
| Recovery Phase | Expected Outcomes | Patient Actions |
| Pre-Surgical | Complete evaluation and preparation | Follow healthcare provider’s instructions |
| Hospital Stay | Monitoring and initial recovery | Rest and follow hospital guidelines |
| Long-Term Recovery | Gradual return to normal activities | Attend follow-up appointments and report any concerns |
Expected Outcomes After Epilepsy Surgery
Epilepsy surgery can change lives for the better. Many patients see a big drop in seizures or even stop having them altogether. This is thanks to new surgical methods and a deeper understanding of epilepsy.
Seizure Freedom Rates
Research shows that a lot of people stop having seizures after surgery. The exact number depends on the surgery type and the patient’s situation. But, the trend is clear: fewer seizures for most people.
Quality of Life Improvements
Epilepsy surgery does more than just reduce seizures. It also boosts quality of life in many ways. Patients often feel healthier, more independent, and can do things they couldn’t before.
These gains aren’t just physical. Many also feel less anxious and depressed. This makes their lives more rewarding.
Conclusion: Making an Informed Decision About Epilepsy Surgery
Epilepsy surgery is a good option for those with drug-resistant epilepsy. Knowing the criteria and outcomes helps patients decide. The evaluation process finds the right candidates, and surgery can greatly improve seizure control.
The main goal of epilepsy surgery is to stop seizures. Many studies show it can greatly improve life quality. People who have surgery may see fewer seizures, better thinking, and overall happiness.
Choosing epilepsy surgery needs a talk with a healthcare expert. They can explain the good and bad sides. Knowing about surgery options and new advancements helps those with drug-resistant epilepsy. It’s a step towards better seizure control and a better life.
FAQ
What is epilepsy surgery?
Epilepsy surgery is a procedure to help people with epilepsy. It aims to stop or reduce seizures. The surgery removes or disconnects the brain part causing seizures.
Who is a candidate for epilepsy surgery?
People with drug-resistant epilepsy might be candidates. They have seizures that medicines can’t stop. Their seizures usually start in one area of the brain.
What is the evaluation process for epilepsy surgery?
The process includes many steps. It starts with neurological exams and imaging like MRI. EEG and sometimes invasive tests are used to find the seizure source.
What are the different types of epilepsy surgery?
There are several surgeries. Some remove parts of the brain, like the temporal lobe. Others, like corpus callosotomy, disconnect brain areas. Laser therapy is a newer, less invasive option.
What are neurostimulation options for epilepsy?
Options include vagus nerve stimulation (VNS) and responsive neurostimulation (RNS). Deep brain stimulation (DBS) is also available. These can help control seizures in those who don’t respond to drugs.
Can children undergo epilepsy surgery?
Yes, kids can get surgery if they have hard-to-control seizures. The process is similar to adults, but kids get extra care.
What are the expected outcomes after epilepsy surgery?
Results vary. Many see a big drop in seizures or even stop having them. Quality of life often improves, but it depends on the person.
What is the recovery process like after epilepsy surgery?
Recovery starts with a hospital stay. Then, rest and slow return to daily life. Follow-up visits are key to keep seizures under control.
Are there risks associated with epilepsy surgery?
Surgery carries risks like infection and bleeding. Neurological problems can also happen. The risks are weighed against the benefits during evaluation.
How effective is epilepsy surgery in achieving seizure freedom?
Effectiveness depends on the surgery type and where the seizures start. Some surgeries, like removing part of the temporal lobe, work better than others.
Can epilepsy surgery be repeated if seizures return?
Sometimes, a second surgery or neurostimulation is considered if seizures come back. Each case is looked at individually to decide the best next step.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/18472487/