Last Updated on December 1, 2025 by Bilal Hasdemir

Approximately 3.4 million people in the United States are living with epilepsy. This is a neurological disorder that causes recurrent seizures.Our guide to amazing, hopeful epilepsy treatment. Discover the critical facts about surgery and if it can offer a permanent cure.
For many, seizures can be controlled with medication. But about 30% of individuals continue to have seizures, even after trying different anti-seizure medications. For these people, epilepsy surgery might be an option.
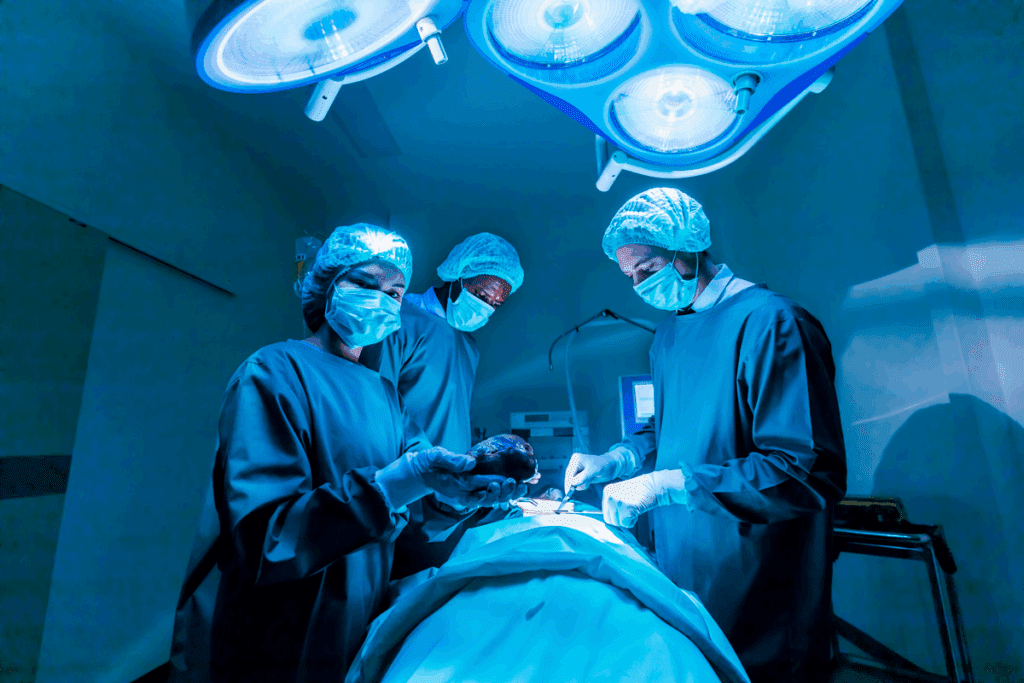
Epilepsy surgery is a surgical procedure. It aims to remove or alter the brain part causing seizures. The goal is to reduce or stop seizures, improving life quality.
Key Takeaways
- Epilepsy affects approximately 3.4 million people in the United States.
- About 30% of individuals with epilepsy continue to experience seizures despite medication.
- Epilepsy surgery is a viable option for those who do not respond to medication.
- The goal of epilepsy surgery is to reduce or eliminate seizures.
- Surgery involves removing or altering the part of the brain causing seizures.
Understanding Epilepsy and Its Impact
It’s important to understand epilepsy to manage its effects and improve life quality. Epilepsy is a complex neurological condition needing thorough care and management.
What is Epilepsy?
Epilepsy is a neurological disorder causing recurring, unprovoked seizures. These seizures happen due to abnormal brain electrical discharges. Seizure management is key, using treatments like medications, diets, and sometimes surgery.
The Epilepsy Foundation says about 3.4 million people in the U.S. have epilepsy. Around 150,000 new cases are diagnosed each year. It can be caused by genetics, head trauma, infections, or developmental disorders.
How Epilepsy Affects Daily Life
Epilepsy can greatly affect daily life, making it hard to work, socialize, and do everyday things. People with epilepsy deal with managing medication side effects and the unpredictability of seizures. They also face the psychological impact of their condition.
“Living with epilepsy requires a multifaceted approach to manage seizures and maintain quality of life. It’s not just about controlling seizures; it’s about living a full life.”
Epilepsy Foundation
The impact of epilepsy on daily life varies. Some may face little disruption, while others may struggle a lot. Effective epilepsy management includes medical treatment, lifestyle changes, and support from healthcare, family, and friends.
| Aspect of Life | Impact of Epilepsy | Management Strategies |
| Employment | Seizures can affect job performance and safety. | Disclosure to employers, workplace accommodations. |
| Social Life | Unpredictability of seizures can limit social activities. | Support groups, social planning, and awareness. |
| Daily Activities | Seizures can impact driving, bathing, and other daily tasks. | Lifestyle adjustments, safety measures, and assistive devices. |
Notable individuals like actor Danny Glover and NFL player Greg Grissom have shared their experiences. They help raise awareness and reduce stigma around epilepsy.
Comprehensive Epilepsy Treatment Options
Epilepsy treatment includes many options tailored for each person. It often uses a mix of treatments to control seizures well.
Anti-Seizure Medications
Medicines are usually the first choice for treating epilepsy. They help reduce how often and how severe seizures are. There are many medicines, and the right one depends on the type of epilepsy and the person’s health.
Commonly prescribed anti-seizure medications include carbamazepine, lamotrigine, and levetiracetam. Each can have different side effects, from mild to serious. It’s important for a doctor to watch how the medicine works and adjust it as needed.
Dietary Approaches
Dietary therapies, like the ketogenic diet, are also effective for some. The ketogenic diet is high in fat and low in carbs. It can help reduce seizures in some people.
Other diets, like the modified Atkins diet, offer similar benefits but might be easier to follow. They can help manage seizures without the need for medication.
Seizure Management Plans
Having a good plan for managing seizures is key for those with epilepsy. This plan should cover medication, diet, and lifestyle changes. It should also include what to do during a seizure.
Key components of a seizure management plan include avoiding triggers, keeping a seizure diary, and having a plan for emergencies. By combining these, people with epilepsy can better control their seizures and live a fuller life.
When Is Surgery Considered for Epilepsy?
Surgery is considered for epilepsy when other treatments don’t work. This usually happens when drug-resistant epilepsy is diagnosed.
Drug-Resistant Epilepsy
Drug-resistant epilepsy is when seizures keep happening even with medication. It’s tough for both patients and doctors, leading to the need for other treatments.
Doctors try many medications before considering surgery. If seizures aren’t controlled, surgery becomes an option.
Identifying Surgical Candidates
Finding the right person for epilepsy surgery is a detailed process. It looks at the type and severity of epilepsy, where seizures start, and the patient’s health.
People with seizures that meds can’t stop and a clear seizure source might be good candidates. A team of doctors decides if surgery is right for them.
- Evaluation of seizure type and frequency
- Imaging studies to locate the seizure focus
- Assessment of the patient’s medical history and current health
Doctors carefully check these things to find who might get better with surgery. This could lead to better seizure control and a better life.
Pre-Surgical Evaluation Process
The pre-surgical evaluation is key to see if a patient is right for epilepsy surgery. It’s a detailed check that includes many tests. These tests help find out who might benefit from surgery.
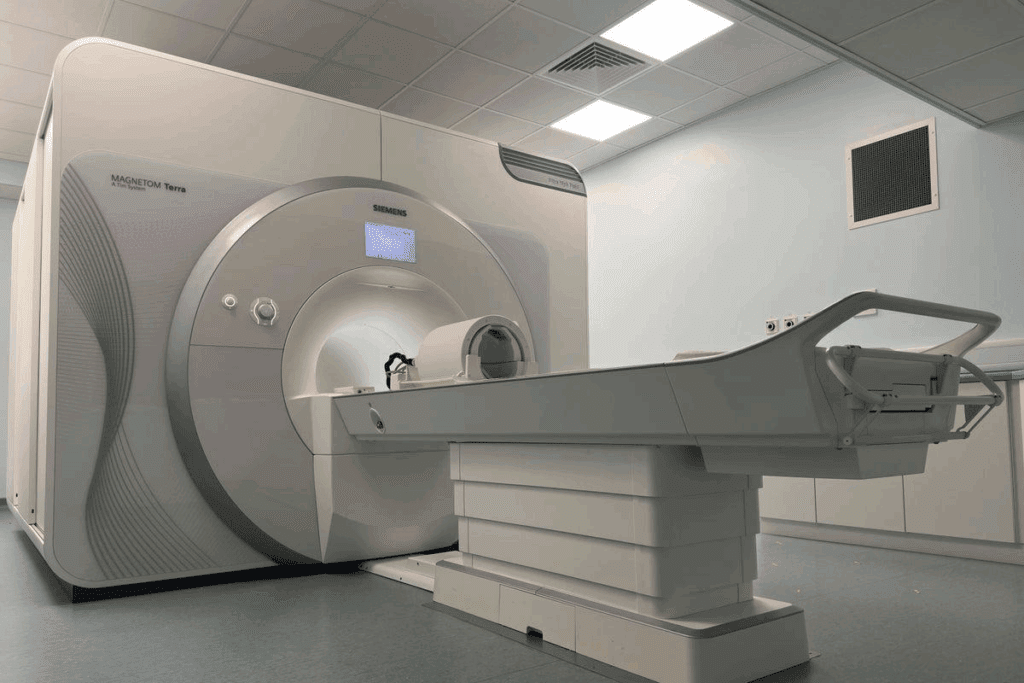
Diagnostic Tests and Imaging
Diagnostic tests are very important in this process. They use imaging techniques like MRI and CT scans. These scans help find where seizures start and how they affect the brain.
- MRI (Magnetic Resonance Imaging): Gives clear pictures of the brain’s structure.
- CT (Computed Tomography) scans: Spot structural issues in the brain.
- Other imaging techniques like PET and SPECT scans check brain function.
Video EEG Monitoring
Video EEG monitoring is a key tool. It records EEG activity and video of the patient at the same time. This helps link seizures with EEG data, giving insights into seizure patterns and where they start.
The WADA Procedure
The WADA procedure, or intracarotid amobarbital test, checks brain function. It tests language and memory in each brain hemisphere. This helps understand the risks of surgery on these important functions.
- The test involves injecting a barbiturate into one carotid artery. This temporarily knocks out one hemisphere.
- Then, language and memory tests are done during this short time.
Healthcare teams use all these test results to decide if surgery is right for a patient. They plan the best surgery approach based on this information.
Types of Epilepsy Surgery: Resective Procedures
Epilepsy surgery, like resective procedures, brings new hope to those with drug-resistant epilepsy. These surgeries remove or change brain tissue that causes seizures. This can lead to a cure or a big drop in seizure frequency.
Temporal Lobectomy
Temporal lobectomy is a common surgery for epilepsy. It removes part of the temporal lobe, where seizures often start. This surgery can greatly reduce or stop seizures in some patients.
Benefits: It has a high success rate in cutting down seizures, improving life quality.
Considerations: There are risks of cognitive and neurological problems.
Anterior Temporal Lobectomy
Anterior temporal lobectomy is similar but focuses on the front part of the temporal lobe. It’s customized for each patient’s seizure area and brain shape.
Advantages: It targets common seizure areas, possibly with fewer brain side effects.
Extratemporal Resections
Extratemporal resections remove brain tissue outside the temporal lobe. This includes areas like the frontal, parietal, or occipital lobes. Success depends on finding and removing the seizure-causing area.
Key Considerations: It needs precise seizure focus location, with outcomes varying by location and extent.
Resective epilepsy surgery, including temporal lobectomy, anterior temporal lobectomy, and extratemporal resections, is a real treatment option for drug-resistant epilepsy. Each surgery is made for the patient’s specific needs, aiming to control seizures and enhance life quality.
Types of Epilepsy Surgery: Disconnection Procedures
Epilepsy surgery uses different disconnection procedures to stop seizures by cutting off bad electrical paths in the brain. These surgeries are tried when other treatments don’t work well. They are key for people with severe epilepsy, helping to lessen seizure frequency and severity.
Corpus Callosotomy
Corpus callosotomy is a surgery that cuts or clamps the corpus callosum. This is the main bridge between the brain’s two halves. It’s often done for patients with seizures that spread from one side to the other and don’t get better with medicine.
By breaking the link between the hemispheres, it can make seizures less severe and happen less often.
Hemispherectomy
Hemispherectomy removes or disconnects a big part of one brain hemisphere. It’s mainly for those with severe seizures from one side, like hemimegalencephaly or Rasmussen’s encephalitis. The main goal is to stop or greatly reduce seizures by taking away the seizure source.
Even though it’s a big surgery, it can work well for some patients.
Hemispherotomy
Hemispherotomy is like hemispherectomy but doesn’t remove the hemisphere. It aims to keep more brain tissue while controlling seizures. It’s for patients who might have been considered for hemispherectomy but could face fewer risks.
This surgery needs careful planning and doing to get the best results.
In summary, surgeries like corpus callosotomy, hemispherectomy, and hemispherotomy are important for treating epilepsy. Each has its own use and benefits. It’s vital to carefully evaluate each patient to find the best surgery for them.
Minimally Invasive Surgical Approaches
Medical technology has improved a lot, leading to new ways to treat epilepsy. These new methods are safer and can help patients recover faster. They also have fewer complications compared to old surgery methods.
Laser Interstitial Thermal Therapy (LITT)
Laser Interstitial Thermal Therapy (LITT) uses laser heat to treat the brain area that causes seizures. LITT is precise and doesn’t harm much of the brain. It’s done with MRI guidance for accurate placement.
LITT is less invasive and has lower infection risks. Patients also stay in the hospital for less time. But, like any surgery, there are risks, like brain problems, depending on where the laser is used.
Stereotactic Electroencephalography (SEEG)
Stereotactic Electroencephalography (SEEG) is used to find and treat epilepsy. It involves putting electrodes in the brain to record electrical signals. This helps find where seizures start, which is key for surgery planning.
SEEG is very helpful for complex cases or when other tests don’t work. It helps doctors decide if surgery is right and how to do it best for each patient.
LITT and SEEG are big steps forward in treating epilepsy. As technology gets better, these methods will help more people with epilepsy get better care.
Neurostimulation Devices for Epilepsy Treatment
For those with epilepsy, neurostimulation devices offer a new hope. These devices use electrical impulses to control brain activity. This can help reduce seizure frequency and severity.
These devices are key in treating epilepsy, for those who don’t respond to meds or surgery. The main types are Vagus Nerve Stimulation (VNS), Responsive Neurostimulation (RNS), and Deep Brain Stimulation (DBS).
Vagus Nerve Stimulation (VNS)
VNS implants a device that sends electrical impulses to the vagus nerve. This nerve sends signals to the brain. It can help reduce seizures in some patients, often used with meds.
The device is placed under the skin in the chest. A lead wire connects it to the vagus nerve in the neck. Though its exact effect is not fully known, it’s thought to help control abnormal brain activity.
Responsive Neurostimulation (RNS)
RNS is a more advanced method. It uses an implanted device to detect and stop abnormal brain activity before it turns into a seizure.
The RNS system has a neurostimulator in the skull and leads in the brain’s seizure areas. It constantly watches brain activity and sends electrical impulses to stop seizures.
Deep Brain Stimulation (DBS)
DBS involves placing electrodes in the brain and connecting them to a chest-implanted pulse generator. This generator sends electrical impulses to the brain, aiming to reduce seizures.
DBS is for those with severe epilepsy, when other treatments fail. It needs careful adjustment to work best.
These devices are a big step forward in treating epilepsy. They offer hope to those who haven’t found relief with traditional treatments. Each device has its own benefits, but they all aim to improve life for those with epilepsy.
Success Rates and Outcomes of Epilepsy Surgery
Looking at how well epilepsy surgery works means checking out many things. This surgery is complex, and its success depends on several factors.
Factors Affecting Surgical Success
Several things can affect how well epilepsy surgery works. These include the type of epilepsy, where the seizures start, and the patient’s health. Getting the diagnosis right and choosing the right patient is key to success.
Other important factors are the surgery method, the surgeon’s experience, and after-care. New surgical methods and technology have helped improve results over time.
Long-Term Seizure Freedom Statistics
Research shows that epilepsy surgery can greatly reduce seizures. It also increases the chance of staying seizure-free for a long time. The exact rate of seizure freedom varies, but many patients see big improvements.
“The goal of epilepsy surgery is not only to reduce seizures but to improve the patient’s quality of life.”
— Epilepsy Specialist
Many patients stay seizure-free after surgery. But, the exact percentage can change based on the study and the patients involved.
Quality of Life Improvements
Epilepsy surgery can greatly improve a patient’s life. It can help people live more independently, enjoy activities, and fully participate in work and social life.
- Improved seizure control
- Enhanced cognitive function
- Better emotional well-being
- Increased independence
The success of epilepsy surgery is not just about stopping seizures. It’s also about how it affects a person’s life overall. This helps doctors give more tailored care and support to patients.
Risks and Complications of Epilepsy Surgery
Epilepsy surgery can bring relief, but it’s important to know the risks. Like any surgery, it has risks that can affect the outcome and life quality.
Common Side Effects
Side effects of epilepsy surgery include temporary swelling, infection, and neurological deficits like weakness or numbness. These are usually treated with medicine or other methods.
Some may face cognitive changes, like memory or language issues. The extent of these changes depends on the brain area involved.
Cognitive and Neurological Impacts
Cognitive and neurological impacts are key in epilepsy surgery. Temporal lobe surgeries can lead to memory decline in some. The risk depends on the surgery type and brain anatomy.
Neurological impacts might include visual field deficits if the surgery affects vision areas. Patients are closely watched for these effects.
Mortality Rates and Serious Complications
Mortality rates for epilepsy surgery are low, but they’re a big concern. Serious complications like stroke, infection, or bleeding can happen. The risk varies with surgery type and patient health.
It’s vital for patients to talk to their healthcare provider about these risks. This helps them understand the possible outcomes and make a well-informed choice about surgery.
Recovery and Rehabilitation After Epilepsy Surgery
Recovering from epilepsy surgery takes a detailed plan. It’s made just for you to help you get better. This is key for the best results.
Immediate Post-Operative Care
Right after surgery, you’ll be in the hospital. You’ll be watched closely for any problems. You’ll also get medicine to help with pain and stop seizures. Close monitoring helps doctors fix any issues fast.
You might feel some discomfort like headaches, tiredness, and swelling. These feelings are usually short-lived and can be managed with medicine. Effective pain management is important for your comfort.
Physical and Cognitive Rehabilitation
Once you’re past the first recovery phase, physical and cognitive rehabilitation starts. This helps you get your strength, mobility, and thinking back. A plan is made just for you, based on your needs and the surgery type.
Physical therapy can help improve your movement and strength. Cognitive therapy works on memory, attention, and other thinking skills that might be affected. Cognitive rehabilitation is customized to fit your needs and is important for independence.
Long-Term Follow-Up Care
Long-term care after surgery is very important. Regular visits with your healthcare team are key. They help track your progress, adjust your medicine, and solve any problems. Ongoing care is essential for the best outcome and a better life.
It’s also important for you and your family to know the signs of complications. If you notice anything unusual, get medical help right away. Education and support are important for managing your condition well.
Patient Experiences and Case Studies
Epilepsy surgery changes patients’ lives in many ways. It’s not just about medical results. It also brings personal and social changes. We need to look closely at what people go through after surgery.
Success Stories
Many patients see big improvements in their lives after surgery. Some stop having seizures altogether. This lets them drive, work, and do things they couldn’t before.
One patient’s story is about how surgery let her go to her child’s school events without fear of seizures. This change greatly improved her family’s life.
These success stories are inspiring. They show the good that can come from surgery. They also highlight the need for careful selection and a tailored approach for each patient.
Challenges and Adjustments
Epilepsy surgery can be very helpful, but it comes with its own set of challenges. Patients often need to recover physically, adjust to new medicines, and deal with emotional changes. Some may face cognitive changes or side effects that are hard to manage.
The journey doesn’t stop after surgery. It continues with rehabilitation and ongoing care. Patients must learn to live with any remaining seizures and side effects. Support from family, healthcare providers, and support groups is key.
- Rehabilitation programs tailored to the individual’s needs can significantly aid in recovery.
- Ongoing medical care is essential for managing side effects and adjusting treatments as necessary.
- Emotional support from family and peers can help patients cope with the psychological impact of their surgery and condition.
Looking at both the successes and challenges helps us understand what epilepsy surgery means. It shows how it changes patients’ lives.
Conclusion
Epilepsy is a complex neurological disorder that needs a full approach to manage. There are many epilepsy treatment options, like medicines, diets, and surgery. These offer hope to those with epilepsy.
Epilepsy surgery is a good choice for those who don’t respond to medicines. Different surgeries can greatly improve seizure control and life quality.
Creating a epilepsy treatment plan involves detailed tests and imaging. This helps find the best treatment. By knowing the options, people with epilepsy can work with their doctors to make a plan that fits their needs.
In conclusion, though epilepsy is tough, today’s treatments offer new ways to manage seizures and improve well-being.
FAQ
What is the success rate of epilepsy surgery?
The success rate of epilepsy surgery varies. It depends on the surgery type, the patient’s condition, and what success means. Studies show that 50% to 80% of patients see a big drop in seizures or even stop having them.
Can epilepsy be cured with surgery?
Surgery can cure or greatly reduce seizures in some. But, calling it a “cure” is tricky. It depends on the epilepsy cause and how well the patient responds to surgery.
What are the risks associated with epilepsy surgery?
Surgery for epilepsy comes with risks. These include infection, bleeding, and problems with thinking or feeling. The risks change based on the surgery type and the patient’s health.
What is a temporal lobectomy?
A temporal lobectomy removes part of the temporal lobe. It’s often used for temporal lobe epilepsy. The goal is to stop seizures by removing the seizure focus.
Are there alternative treatments to surgery for epilepsy?
Yes, there are other treatments. These include medicines, special diets, vagus nerve stimulation, and neurostimulation. The right treatment depends on the patient’s needs and condition.
How is a patient evaluated for epilepsy surgery?
Evaluating a patient for surgery is detailed. It includes looking at medical history, doing a neurological exam, and using imaging like MRI and PET. EEG and sometimes invasive tests are also used to find the seizure focus and assess surgery risks and benefits.
Can children undergo epilepsy surgery?
Yes, children can have surgery for epilepsy. The decision is based on a detailed look at their condition, how bad their seizures are, and the surgery’s benefits and risks.
What is the difference between resective and disconnection epilepsy surgery?
Resective surgery removes the seizure focus. Disconnection surgery cuts the pathways that let seizures spread, without removing brain tissue.
How long does it take to recover from epilepsy surgery?
Recovery time varies. It depends on the surgery, the patient’s health, and how big the procedure was. Patients usually need weeks to months to recover, and some may need ongoing rehab.
Are there any long-term effects of epilepsy surgery?
Surgery can have long-term effects. These might include changes in thinking, mood, or behavior. There’s also a chance of seizures coming back. Regular check-ups are key to managing these effects.
Can epilepsy surgery improve quality of life?
Yes, successful surgery can greatly improve life. It can reduce or stop seizures, letting people do more in daily life, work, and social activities.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJM200108023450501