Last Updated on November 17, 2025 by Ugurkan Demir
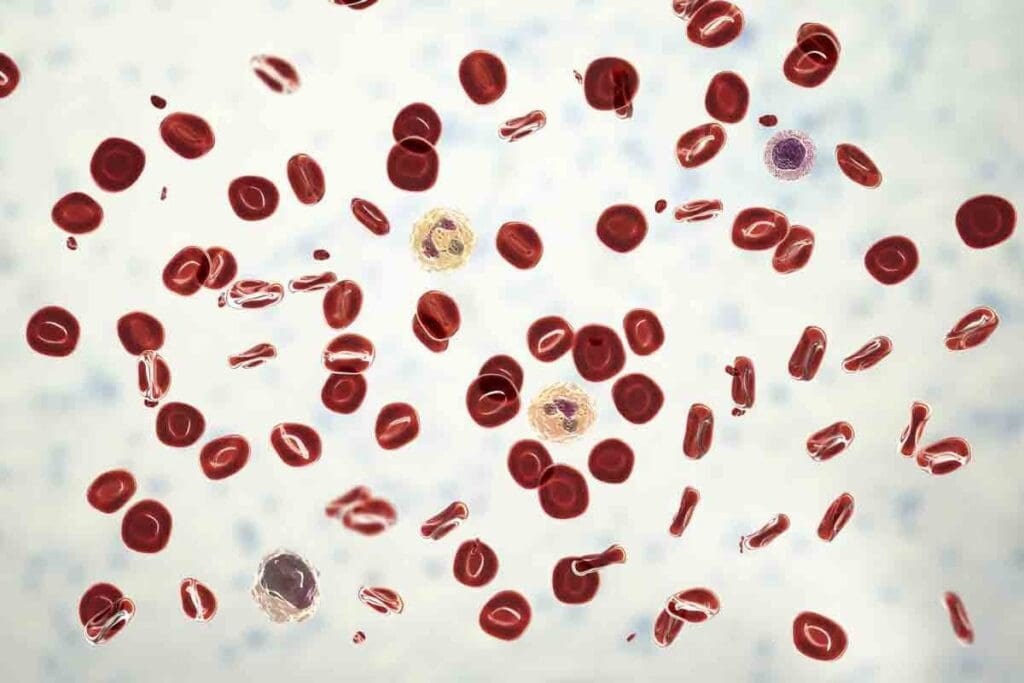
Red blood cell (RBC) problems can really hurt your health. Erythrocyte disorders are a group of conditions. They affect how red blood cells are made, work, or last.
It’s important to know about these red blood cell disorders. Liv Hospital is here to help. They use their knowledge to treat RBC problems in a caring way. This approach helps patients get better.

Disorders of the erythrocytes, or red blood cells, can lead to impaired oxygen delivery, affecting overall health. Red blood cells play a key role in transporting oxygen to the body’s organs and tissues. Understanding these disorders is essential for diagnosing and treating related conditions effectively.
Normal red blood cells are disk-shaped and flexible. This allows them to move through narrow blood vessels. They contain hemoglobin, a protein that binds oxygen in the lungs and releases it into the tissues. The structure and function of red blood cells are critical for maintaining adequate oxygen supply to the body’s tissues.
The normal function of red blood cells is dependent on their:
Erythrocyte disorders disrupt oxygen delivery by altering the structure or function of red blood cells. This disruption can lead to inadequate oxygen supply to tissues and organs, resulting in various clinical manifestations.
The pathophysiology involves:
Common consequences include:
Despite the variety of erythrocyte disorders, there are common symptoms that arise due to impaired oxygen delivery. These include:
Recognizing these symptoms is key for early diagnosis and treatment of underlying red blood cell disorders.
Iron deficiency anemia is the most common anemia worldwide, affecting millions. It happens when there’s not enough iron. Iron is key for making hemoglobin, which carries oxygen in red blood cells.
Iron deficiency anemia comes from many reasons. These include not getting enough iron in food, losing blood, and needing more iron during pregnancy. About a quarter of the world’s people have anemia, with iron deficiency being the main cause.
Some places have more anemia due to bad nutrition and less healthcare. Women, children, and people with chronic diseases are at higher risk.
Iron deficiency anemia shows in different ways. Common signs are feeling very tired, looking pale, and sometimes wanting to eat non-food items. These happen because the body can’t carry enough oxygen without enough hemoglobin.
Other signs might be feeling weak, dizzy, or short of breath. In severe cases, it can cause problems like poor pregnancy outcomes and lower brain function in kids.
To diagnose iron deficiency anemia, doctors do a complete blood count (CBC). They check hemoglobin and red blood cell levels. Then, they test serum ferritin and iron levels to confirm.
Treatment usually means taking iron, either by mouth or through a vein. It depends on how bad the deficiency is and how well the patient responds. Eating more iron-rich foods and vitamin C is also important to help the body absorb iron better.
It’s key to keep track of how well treatment is working and fix any underlying issues. This helps manage iron deficiency anemia effectively.
Understanding sickle cell disease’s genetic roots is key to finding treatments. It’s caused by a mutation in the HBB gene. This mutation leads to abnormal hemoglobin, known as sickle hemoglobin or HbS.
Sickle cell disease is inherited in an autosomal recessive pattern. This means a person needs two defective HBB genes to have the disease. Carriers have one normal and one defective gene. They usually don’t show the disease’s full symptoms but can pass the mutated gene to their kids.
The genetic mutation causes HbS production. Under low oxygen, HbS polymerizes, making red blood cells sickle-shaped. This shape makes it hard for cells to move through small blood vessels, causing vaso-occlusive crises.
“Sickle cell disease is a complex condition with a wide range of clinical manifestations, from mild to severe.”
Dr. Jane Smith, Hematologist
Vaso-occlusive crises are a key feature of sickle cell disease. They cause sudden pain due to blood vessel blockage by sickled red blood cells. These episodes can be triggered by dehydration, infection, and extreme temperatures.
Chronic organ damage is another big problem. It comes from repeated episodes of ischemia and infarction. Organs like the spleen, kidneys, and lungs are often affected. For example, splenic sequestration can cause sudden spleen enlargement and severe anemia.
| Organ/System | Complications |
| Spleen | Splenic sequestration, autosplenectomy |
| Kidneys | Chronic kidney disease, renal failure |
| Lungs | Acute chest syndrome, pulmonary hypertension |
Managing sickle cell disease has improved a lot. Now, we focus on preventing complications and improving life quality. Hydroxyurea is a key drug used to reduce crisis frequency by boosting fetal hemoglobin production.
Gene therapy is a promising new area. It aims to fix the genetic defect, restoring normal hemoglobin production. Recent studies with CRISPR/Cas9 show great promise.
The future of sickle cell disease management is in research and innovation, mainly in gene therapy. As we learn more about the disease’s genetics, we’ll be able to develop better treatments.
Thalassemia syndromes are a group of inherited conditions. They affect how the body makes hemoglobin. This is because of changes in genes that code for hemoglobin’s parts.
Thalassemia syndromes are split into alpha and beta types. Alpha thalassemia happens when there’s a problem with genes for alpha-globin chains. Beta thalassemia is caused by issues with genes for beta-globin chains.
Alpha Thalassemia: The severity of alpha thalassemia varies. If one gene is affected, people might not show symptoms. But, if all four genes are affected, it’s a severe form called Homozygous Alpha Thalassemia or Hydrops Fetalis. This is usually fatal without special care during pregnancy.
Beta Thalassemia: Beta thalassemia major, or Cooley’s anemia, happens when both genes are affected. It causes severe anemia. Beta thalassemia intermedia is less severe, with milder anemia and fewer transfusions needed.
Thalassemia symptoms range from none to severe anemia. Symptoms include tiredness, pale skin, and slow growth in kids. Severe cases can cause bone changes and organ damage from too much iron.
“The clinical spectrum of thalassemia is broad, necessitating a tailored approach to management based on the severity of the disease.”
Dr. Jane Smith, Hematologist
Managing thalassemia major includes regular blood transfusions. This keeps hemoglobin levels up and stops the body from making too many red blood cells. But, it causes iron buildup, which is treated with iron chelation therapy.
| Management Strategy | Description | Benefits |
| Regular Blood Transfusions | Maintaining hemoglobin levels above 9-10 g/dL | Suppresses ineffective erythropoiesis, improves quality of life |
| Iron Chelation Therapy | Use of chelators like deferoxamine, deferiprone, or deferasirox | Reduces iron overload, prevents organ damage |
It’s important to keep an eye on and adjust transfusions and chelation therapy. This helps patients with thalassemia syndromes get the best care.
Red blood cell membrane defects are key in hereditary spherocytosis. This genetic disorder changes the proteins in the red blood cell membrane. It makes the cells round and less flexible.
Hereditary spherocytosis is caused by mutations in genes for membrane proteins. These include spectrin, ankyrin, and band 3. The mutations cause the loss of membrane lipid and the formation of spherocytes.
The condition is usually inherited in an autosomal dominant manner. But, autosomal recessive forms also exist. The genetic defects lead to a range of clinical severities, from mild to severe hemolytic anemia.
Understanding the molecular basis is key for diagnosing and managing the condition effectively.
Patients with hereditary spherocytosis often have jaundice due to hemolysis. They also have splenomegaly from sequestration of abnormal red blood cells. An increased risk of gallstones is due to chronic bilirubin overload.
| Clinical Feature | Description | Prevalence |
| Jaundice | Yellowing of the skin and eyes due to hemolysis | Common |
| Splenomegaly | Enlargement of the spleen due to sequestration of spherocytes | Frequent |
| Gallstones | Formation of stones in the gallbladder due to chronic bilirubin overload | Common |
The diagnosis of hereditary spherocytosis is based on clinical findings, laboratory tests, and genetic analysis. Splenectomy is considered in severe cases to reduce hemolysis. It’s not without risks and is typically reserved for transfusion-dependent patients or those with significant symptoms.
The decision to perform splenectomy is made on a case-by-case basis. It considers the severity of the condition and the patient’s overall health. Partial splenectomy has emerged as an alternative approach to reduce the risks associated with total splenectomy.
Polycythemia vera is a condition where the bone marrow makes too many red blood cells. This leads to thicker blood and can cause blood clots.
Most people with polycythemia vera have a JAK2 gene mutation. This mutation turns on a pathway that makes blood cells grow too much. It helps the disease grow.
“The JAK2V617F mutation is a key driver in the pathogenesis of polycythemia vera, making it a target for treatment,” studies say.
Too many red blood cells make blood thicker. This can cause headaches, dizziness, and tiredness. It also raises the risk of blood clots, like deep vein thrombosis and stroke.
Common symptoms include:
Phlebotomy is a key treatment for polycythemia vera. It helps lower red blood cell count and blood thickness. It also reduces the risk of blood clots. Hydroxyurea is another treatment that slows down blood cell growth.
Doctors often use a mix of phlebotomy and medicines to treat the condition well.
Autoimmune hemolytic anemia happens when the body attacks its own red blood cells. This leads to their early destruction. It shows through different symptoms and is split into types based on the antibodies.
This condition is mainly divided into two types: warm and cold antibody hemolytic anemia. Warm antibody anemia is more common. It involves antibodies active at body temperature, causing damage mainly in the spleen.
Cold antibody anemia is caused by antibodies active at cooler temperatures. It’s often linked to infections or certain cancers.
Symptoms of autoimmune hemolytic anemia include jaundice, fatigue, and dark urine. These happen because red blood cells are destroyed quickly. Patients might also have an enlarged spleen and, in severe cases, heart problems.
The start of symptoms can be sudden or slow. It depends on how fast red blood cells are destroyed and how well the body can cope.
The first treatment is usually corticosteroids, like prednisone. They help reduce the immune system’s attack on red blood cells. Most patients see improvement within a few weeks.
If corticosteroids don’t work or are needed for a long time, other treatments are considered. These include drugs like rituximab. In some cases, removing the spleen might be an option for those with warm antibody anemia who don’t respond to other treatments.
| Treatment Option | Description | Response Rate |
| Corticosteroids | First-line treatment to suppress immune system | 70-80% |
| Rituximab | Second-line immunosuppressive therapy | 60-70% |
| Splenectomy | Surgical removal of spleen for refractory cases | 50-60% |
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is a genetic disorder. It affects red blood cells, making them vulnerable to oxidative stress. This condition happens when the glucose-6-phosphate dehydrogenase enzyme doesn’t work right.
G6PD deficiency is common in Africa, the Mediterranean, and Asia. It’s interesting because it might protect against malaria in these areas. The genetic makeup of G6PD deficiency is complex, with many mutations.
This protection against malaria might explain why G6PD deficiency is more common in some places. But, it also means people with this deficiency are more likely to have hemolytic episodes under certain conditions.
People with G6PD deficiency can have hemolytic episodes triggered by things like medications, infections, and certain foods. These episodes can cause jaundice, fatigue, and dark urine. This is because their red blood cells are destroyed quickly.
Common triggers include antimalarial drugs, sulfonamides, and some antibiotics. It’s important to avoid these triggers to manage the condition and prevent crises.
Managing G6PD deficiency means avoiding known triggers and being careful with medications. Patients should tell their doctors about their condition to get safe treatments.
When a hemolytic episode happens, treatment focuses on easing symptoms and watching for complications. In serious cases, blood transfusions might be needed to replace lost red blood cells.
Megaloblastic anemias are caused by a lack of vitamin B12 or folate. These deficiencies stop red blood cells from maturing right. This leads to the production of big, abnormal red blood cells.
Macrocytosis is a key sign of megaloblastic anemia. It means red blood cells are too big. This happens because DNA synthesis is off, which is needed for cell division.
Vitamin B12 and folate are vital for this process. Without enough, cells can’t divide right. This results in the large red blood cells seen in this anemia.
This problem isn’t just for red blood cells. It also affects other cells that grow fast, like those in the gut and bone marrow.
Megaloblastic anemia can cause fatigue, weakness, and neurological changes. The brain effects are more common with vitamin B12 deficiency. They can lead to nerve damage and problems with thinking.
Other signs include anemia, low white blood cells, and low platelets.
Treating megaloblastic anemia means replacing the missing vitamin. Vitamin B12 is often given through injections. Folate is taken by mouth.
It’s also important to find and fix the reason for the deficiency. This could be a bad diet, trouble absorbing nutrients, or another health issue.
It’s key to watch how the treatment works. Blood counts and symptoms should get better in a few weeks to months.
Chronic diseases can harm how our bodies make and work with red blood cells. This leads to secondary RBC abnormalities. These issues make it harder to manage chronic conditions.
Chronic diseases often cause ongoing inflammation. This can mess with red blood cell production. Inflammatory cytokines play a big role by making it hard to get iron for making new red blood cells.
Inflammation affects iron in several ways:
Chronic kidney disease (CKD) is a big reason for secondary RBC problems. It’s because of a lack of erythropoietin, a hormone that helps make red blood cells. As kidneys get worse, they make less erythropoietin, causing anemia.
The link between kidney disease and less erythropoietin is clear:
| Renal Disease Stage | Erythropoietin Production | Impact on RBC Production |
| Mild CKD | Normal to slightly reduced | Mild anemia |
| Moderate CKD | Reduced | Moderate anemia |
| Severe CKD | Significantly reduced | Severe anemia |
To find secondary RBC problems in chronic diseases, we need to test iron, erythropoietin, and kidney function. Treatments aim to fix the root cause, like fighting inflammation or giving erythropoietin to those with CKD.
Treatment plans might include:
Recent breakthroughs in red blood cell testing have greatly improved our understanding and management of erythrocyte disorders. Conditions like Thalassemia, Sickle Cell Disease, and Hereditary Spherocytosis are now better diagnosed and treated thanks to advances in diagnosis.
Advances in diagnosis, including digital morphology and AI-powered image analysis, have helped healthcare professionals. They can now identify abnormal red blood cell shapes and diagnose conditions more accurately. Treatment options have also expanded, with gene therapy being explored for certain erythrocyte disorders.
The importance of continued research and awareness in managing these conditions cannot be overstated. As our understanding of red blood cell disorders evolves, so too will our ability to provide effective treatment and improve patient outcomes. By staying up-to-date with the latest advances in diagnosis and treatment, healthcare professionals can deliver the best possible care for patients with these conditions.
Erythrocyte disorders, also known as red blood cell disorders, affect how red blood cells are made, work, or last. This can cause health problems.
Iron deficiency anemia is the most common RBC deficiency disease. It happens when there’s not enough iron for hemoglobin.
Sickle cell disease is a genetic disorder. It affects hemoglobin production, making red blood cells misshapen and short-lived. This leads to crises and long-term health issues.
Thalassemia syndromes are genetic disorders affecting hemoglobin production. They cause anemia and other problems, with alpha and beta thalassemia being the main types.
Hereditary spherocytosis is a genetic disorder affecting the red blood cell membrane. It makes cells spherical and prone to breaking down. This can cause jaundice, enlarged spleen, and gallstones.
Polycythemia vera is a disorder where too many red blood cells are made. It’s often caused by a JAK2 gene mutation. This leads to symptoms like thick blood and increased risk of blood clots.
Autoimmune hemolytic anemia is when the immune system attacks and destroys red blood cells. This causes anemia, jaundice, and other symptoms.
Glucose-6-phosphate dehydrogenase deficiency is a genetic disorder. It affects the enzyme protecting red blood cells from damage. This makes them vulnerable to breaking down under certain conditions.
Megaloblastic anemias are conditions where red blood cells are too large. They often result from vitamin B12 or folate deficiency. This impairs DNA synthesis and causes various symptoms.
Diagnosing red blood cell disorders involves a medical history, physical exam, and lab tests. These include complete blood counts, blood smears, and sometimes genetic testing or bone marrow exams.
Treatment options vary by condition. They may include iron replacement, vitamin supplements, blood transfusions, and medications. In some cases, gene therapy or splenectomy may be considered.
Some disorders are genetic and can’t be prevented. But, others can be managed with a balanced diet, avoiding certain medications, and managing health conditions.
Inflammatory cytokines can disrupt iron metabolism and suppress erythropoiesis. They can also promote abnormal red blood cell production, often seen in chronic diseases.
Erythropoietin deficiency, common in renal disease, reduces red blood cell production. This leads to anemia and related symptoms.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!