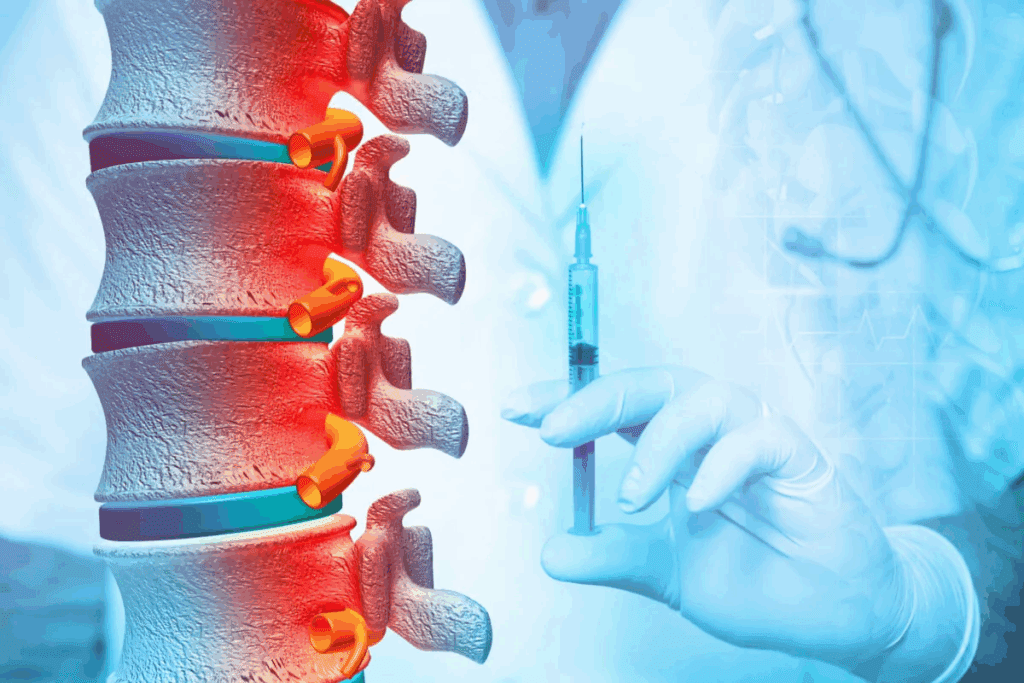
At Liv Hospital, we know how hard radicular pain can be. It’s caused by inflammation or compression of the spinal nerves in the cervical region. To help, we offer cervical epidural steroid injections. This is a safe, small procedure that puts corticosteroids right where they need to be. Understand how esi injections cervical spine work, including needle size, pain relief, and safety.
Cervical epidural steroid injections help with chronic pain from nerve root inflammation. They put corticosteroids into the epidural space. This can really help with pain and discomfort. We aim to give top-notch healthcare, with full support for international patients.
Key Takeaways
- Cervical epidural steroid injections are a valuable treatment option for radicular pain caused by inflammation or compression of the spinal nerves.
- The procedure involves delivering corticosteroids directly into the epidural space to alleviate pain and discomfort.
- Our specialists at Liv Hospital are dedicated to providing comprehensive care and support to international patients.
- Cervical ESI injections are a minimally invasive procedure with a focus on patient safety and comfort.
- We utilize the latest medical techniques to ensure effective pain relief and optimal clinical outcomes.
Understanding Cervical Epidural Steroid Injections

Cervical epidural steroid injections are a key treatment for neck pain and radiculopathy. They involve putting corticosteroids into the epidural space around the spinal cord in the neck. This aims to cut down inflammation and ease pain.
What Is a Cervical ESI?
A cervical epidural steroid injection (CESI) is a small procedure. Corticosteroids are injected into the epidural space of the cervical spine. It’s meant to lessen inflammation and swelling around the spinal nerves, helping to reduce pain.
The epidural space is filled with fat and is between the bone and the sac (dura mater) that covers the spinal cord. By targeting this area, CESI can lower pressure on the spinal nerves. This gives patients a lot of pain relief.
Common Conditions Treated with Cervical ESI
Cervical epidural steroid injections help with radicular pain or neck pain caused by disc problems. They treat several conditions, including:
- Cervical spondylosis: Wear and tear on the discs in the neck.
- Disc herniation: When the soft inner gel of the disc leaks out through a tear in the outer disc.
- Spinal stenosis: Narrowing of the spaces within the spine, which can put pressure on the nerves.
- Radiculopathy: Disease or injury of the nerve roots, often causing pain, numbness, or weakness.
In summary, cervical epidural steroid injections are a valuable treatment for many cervical spine disorders. They offer relief from pain and inflammation. Understanding CESI and what it treats helps patients make better choices about their care.
ESI Injections in the Cervical Spine: Mechanism of Action

The way cervical ESI injections work is quite complex. They reduce inflammation and target specific pain pathways. To grasp how they help, we must look at their effects on the body and their targets.
How Corticosteroids Reduce Inflammation
Corticosteroids, found in ESI injections, cut down inflammation and swelling around irritated nerve roots. According to Pioneer Spine and Sport Physicians, they ease pain by stopping the inflammatory process. This anti-inflammatory action is key in easing nerve root pressure and reducing pain.
The process starts with corticosteroids binding to receptors. This stops the production of pro-inflammatory cytokines. As a result, the swelling around the nerves goes down, bringing pain relief. This is why cervical ESI injections help patients feel better.
Targeting the Epidural Space
The epidural space is a key area for cervical ESI injections. It’s around the dural sac, which holds the spinal cord and nerve roots. By putting corticosteroids here, we can tackle the inflammation of the nerves. Getting the injection to the right spot is vital for success.
Let’s look at why targeting the epidural space is so important. It’s between the bony vertebrae and the dural sac. Injecting corticosteroids here means they can reach the inflamed nerves directly, making the treatment more effective.
Pain Relief Pathways
Pain relief from cervical ESI injections comes through several ways. First, less inflammation around the nerves means less pressure on them. This reduces pain signals to the brain. Second, corticosteroids can directly calm down the nerves, making them less sensitive to pain.
To understand how corticosteroids help, let’s see their effects on inflammation and pain:
| Effect | Description | Outcome |
| Anti-inflammatory action | Reduces swelling around nerve roots | Decreased pressure on nerves |
| Direct effect on nerve roots | Reduces the excitability of nerve roots | Diminished pain perception |
| Inhibition of pro-inflammatory cytokines | Suppresses the inflammatory process | Reduced inflammation |
By knowing these mechanisms, we see how cervical ESI injections offer targeted pain relief. Their anti-inflammatory effects and direct action on nerves make them a good treatment for neck pain.
Cervical Epidural Steroid Injection Needle Size and Selection
Choosing the right needle size for cervical ESI is key. The correct size and type are essential for accurate placement and to avoid complications.
Standard Needle Dimensions
Needle sizes for cervical epidural steroid injections range from 25G to 2-3.5 inches. The exact size depends on the patient’s anatomy and the procedure’s approach. StatPearls notes that the right needle size and type are critical for a successful and safe procedure.
Common needle sizes include:
- 25G, 2.5 inches for most cervical ESI procedures
- 25G, 3.5 inches for patients with larger body mass or specific anatomical considerations
Factors Influencing Needle Selection
Several factors affect needle size choice for cervical ESI:
- Patient Anatomy: The size and shape of the patient’s neck and spine influence needle selection.
- Approach: Different approaches (e.g., interlaminar vs. transforaminal) may need different needle sizes and types.
- Practitioner Preference: The practitioner’s experience and preference also play a role in needle selection.
Safety Considerations in Needle Selection
Safety is a top concern when choosing needle size for cervical ESI. The right needle size helps to:
- Minimize the risk of dural puncture
- Avoid nerve root injury
- Ensure accurate placement of corticosteroids
Medical professionals stress that “The key to a successful cervical ESI procedure lies in the careful selection of needle size and type, coupled with precise technique and imaging guidance.”
Cervical Interlaminar Epidural Steroid Injection Techniques
Interlaminar epidural steroid injections are a key treatment for cervical spine issues. They involve injecting corticosteroids into the epidural space around the spinal cord. This method is safe and effective.
Midline Approach
The midline approach is a common technique for these injections. It involves inserting the needle between two vertebrae in the midline. Precision is key to avoiding problems.
- The patient lies face down during the procedure.
- The skin is cleaned and numbed.
- A needle is guided by X-ray.
Contralateral Oblique Approach
The contralateral oblique approach is another method. It involves inserting the needle at an angle from the midline. This method is useful in some cases.
- The needle is guided by X-ray to ensure it’s in the right spot.
- This approach can help avoid some issues with the midline method.
Patient Positioning and Preparation
Getting the patient’s position right is essential for success. Comfort and safety are top priorities.
- Patients lie face down with their neck slightly bent.
- It’s important to watch their vital signs during the procedure.
Needle Trajectory and Depth
Getting the needle in the right spot is critical. X-ray guidance helps track the needle’s path and depth.
Healthcare providers use these methods to manage pain and swelling in the cervical spine. The choice of technique depends on the patient’s anatomy and the condition being treated.
Transforaminal Approach for Cervical ESI
The transforaminal approach for cervical epidural steroid injections is a targeted solution for cervical spine pain. It delivers medication directly to the affected nerve roots. This helps patients with cervical radiculopathy find relief.
Targeting Specific Nerve Roots
This method targets specific nerve roots with precision. Corticosteroids are injected into the neural foramen. This reduces inflammation and eases pain from cervical spine conditions.
Recent studies show promise in managing pain from cervical disc herniation and spinal stenosis with this approach.
Technical Considerations
Several technical considerations are important for a transforaminal cervical ESI. These include:
- Precise needle placement using fluoroscopic guidance
- Careful selection of the correct neural foramen
- Monitoring for possible complications
Advantages and Limitations
The transforaminal approach offers targeted pain relief and potentially lower corticosteroid doses. Yet, it also has risks like vascular injection or nerve damage.
A comparison of the transforaminal and interlaminar approaches is provided in the table below:
| Approach | Target Area | Advantages | Limitations |
| Transforaminal | Specific nerve roots | Targeted pain relief, potentially lower steroid doses | Risk of vascular injection, nerve damage |
| Interlaminar | Epidural space | Broad coverage of affected areas | Potential for less targeted relief, higher steroid doses |
Patient Selection for Transforaminal Approach
Choosing the right patients is key for success with transforaminal cervical ESI. Ideal candidates have:
- Cervical radiculopathy not helped by other treatments
- Specific nerve root compression is seen on imaging
- No major reasons to avoid steroid injections
Healthcare providers can make transforaminal cervical epidural steroid injections more effective by carefully evaluating patients and using advanced imaging.
The Role of Imaging in Cervical Spine Injections
Imaging technologies, like fluoroscopy, have changed how cervical epidural steroid injections are done. They make sure these procedures are both accurate and safe.
Fluoroscopy Guidance Techniques
Fluoroscopy is key in cervical epidural steroid injections. It uses a fluoroscope to show real-time X-ray images. This lets doctors see where the needle is going and where it is.
Here’s how fluoroscopy works:
- Patients lie on a fluoroscopy table.
- A fluoroscope shows the target area.
- The needle is guided to the epidural space with images.
Contrast Medium Usage
Contrast medium is used with fluoroscopy to check if the needle is in the right spot. It also shows where the medicine goes. We use a small amount to make sure the medicine reaches the right area.
Contrast medium helps by:
- Confirming the needle is in the epidural space.
- Showing if the medicine might go into the blood vessels.
- Seeing how the medicine spreads.
Real-Time Visualization Benefits
Seeing everything in real-time during cervical epidural steroid injections has big advantages. It makes the procedure more accurate and safer. We can adjust the needle as needed to make sure the medicine goes exactly where it should.
The benefits of real-time imaging are:
- It makes the procedure more precise.
- It lowers the chance of harming blood vessels or nerves.
- It makes the patient safer.
Radiation Safety Considerations
Fluoroscopy is great for these injections, but it does involve radiation. We’re very careful about radiation safety. We use special techniques like collimation and pulsed fluoroscopy to keep exposure low.
Here’s how we keep radiation safe:
- We use the least amount of radiation needed.
- We follow strict safety rules for everyone involved.
- We keep an eye on how much radiation everyone gets.
Epidural Injection in Neck C7-T1: The Preferred Site
The C7-T1 area is the top choice for cervical epidural injections. It’s known for its consistent anatomy and lower risk of problems. This makes it a perfect spot for these injections.
Anatomical Advantages of C7-T1
The C7-T1 area has some key anatomical advantages. It’s wider than other cervical spots, making it easier to reach. The ligamentum flavum here is thicker, helping doctors find the right spot during the procedure.
Reduced Complication Risk
The C7-T1 area has a lower risk of complications than other spots. It’s less mobile, which means the needle is less likely to move. Plus, it’s less likely to have serious degenerative changes, making it easier to place the needle accurately.
Technique Specifics for C7-T1 Injections
For C7-T1 injections, fluoroscopy guidance is key. The patient lies on their stomach with their neck slightly bent. The needle is guided under X-ray, using a special technique to make sure it’s in the right place.
Distribution of Medication from C7-T1
The medication from C7-T1 injections works well for cervical spine issues. Studies show it can spread to many levels in the cervical epidural space. This helps more areas, depending on the amount of medication and the patient’s body.
What to Expect During and After Cervical Epidural Injections
When you think about cervical epidural steroid injections, knowing what happens during and after is key. We help our patients get ready for everything they might face.
The Procedure Experience
The procedure takes place in a safe place like a hospital or clinic. Patients lie on their stomach or side for the shot. We use special X-rays to guide the needle.
Patients might feel some pressure or pain, but we use local anesthesia to lessen it. The actual shot is quick, but getting ready can take longer.
Immediate Post-Procedure Effects
Right after, we watch patients for any bad reactions. Some might feel better or worse because of the needle or medicine.
Patients might feel drowsy or numb from the anesthetic. We tell them to have someone drive them home and not to do too much for the rest of the day.
Timeline for Pain Relief
Pain relief usually starts within a week. But some people feel better sooner. Pioneer Spine and Sport Physicians says relief can vary, with some noticing it in just a few days.
Duration of Therapeutic Effect
How long pain relief lasts can differ. Some might only feel better for a few weeks, while others might have months of relief. The exact time depends on the condition, how well the shot was done, and how the body reacts to the medicine.
Knowing what to expect helps patients make better choices about their treatment.
Potential Side Effects and Complications of Cervical Steroid Epidural
Patients need to know about the risks and side effects of cervical ESI. This treatment is usually safe but can have some serious side effects. Knowing these can help patients make informed decisions.
Common Temporary Side Effects
Most people do well with cervical ESI, but some may feel temporary side effects. These can include:
- Temporary numbness or weakness in the arms or legs
- Headache
- Dizziness
- Facial flushing
- Insomnia
- Increased blood sugar levels (for diabetic patients)
These side effects are usually mild and go away in a few days. Many people start feeling better from the pain relief within a week.
Rare but Serious Complications
Even though rare, serious problems can happen with cervical epidural steroid injections. These include:
- Nerve damage
- Infection
- Bleeding
- Spinal cord injury
- Stroke or cerebral vasculature complications
- Allergic reactions to the injected medications
It’s key for patients to be aware of these risks and talk to their healthcare provider about any concerns.
Risk Minimization Strategies
To lower the risks of cervical ESI, several steps are taken:
- Imaging guidance (e.g., fluoroscopy) during the procedure
- Careful patient selection and evaluation
- Precise technique and needle placement
- Use of appropriate needle size and type
- Monitoring of patients during and after the procedure
| Risk Minimization Strategy | Description | Benefit |
| Imaging Guidance | Use of fluoroscopy to guide needle placement | Improved accuracy, reduced risk of complications |
| Patient Selection | Careful evaluation of patient suitability | Reduced risk of adverse reactions |
| Precise Technique | Accurate needle placement and medication delivery | Enhanced efficacy, reduced risk of nerve damage |
When to Seek Medical Attention
If you experience any of these after a cervical ESI, seek medical help right away:
- Severe headache or neck pain
- Progressive weakness or numbness in the arms or legs
- Difficulty controlling bladder or bowel function
- Fever or signs of infection at the injection site
- Any other concerning or worsening symptoms
Knowing these issues and when to get help can greatly improve outcomes for cervical epidural steroid injections.
Conclusion: Making Informed Decisions About Cervical ESI Treatment
Cervical epidural steroid injections (CESI) are a helpful way to manage chronic pain. They are used for conditions affecting the cervical spine. Knowing about CESI can help patients make smart choices about their treatment.
Studies show CESI can reduce inflammation and ease pain. The use of imaging, like fluoroscopy, makes the procedure more precise. This ensures the steroid medication is placed correctly around the spinal cord.
CESI is a proven treatment for many cervical spine issues. Understanding the procedure, including needle size and injection techniques, helps patients. This knowledge lets them explore their treatment options more effectively.
Choosing to have CESI should be a decision made with a healthcare provider. They consider your specific situation and medical history. This way, patients can use CESI to find relief from pain and improve their quality of life.
FAQ
What is a cervical epidural steroid injection?
A cervical epidural steroid injection is a procedure. It involves putting corticosteroids into the space around the spinal cord in the neck. This helps reduce inflammation and eases pain.
What conditions are treated with cervical ESI injections?
Cervical ESI injections are used for several conditions. These include cervical spondylosis, disc herniation, and spinal stenosis.
How do corticosteroids reduce inflammation in cervical ESI injections?
Corticosteroids target the epidural space. They reduce swelling and irritation of the spinal nerves. This helps alleviate pain.
What is the typical needle size used for cervical epidural steroid injections?
The needle size for cervical epidural steroid injections is usually 25G. It is 2-3.5 inches long.
Why is the C7-T1 level preferred for epidural injections in the neck?
The C7-T1 level is preferred for several reasons. It has a wider epidural space. This reduces the risk of complications.
What are the advantages of the transforaminal approach for cervical ESI injections?
The transforaminal approach targets specific nerve roots. This can lead to more effective pain relief.
What are the possible side effects of cervical steroid epidural injections?
Temporary side effects include pain at the injection site and headache. Facial flushing is also common. Rare but serious complications include infection, nerve damage, and spinal cord injury.
How long does it take to experience pain relief after a cervical ESI injection?
Pain relief can vary. Many patients feel relief within a few days to a week after the procedure.
How long does the therapeutic effect of cervical ESI injections last?
The effect can last several months. It depends on the individual and the condition being treated.
What role does imaging play in cervical spine injections?
Imaging, like fluoroscopy, is key. It guides needle placement. This ensures accurate delivery of corticosteroids.
Are there any specific preparations needed before undergoing a cervical ESI injection?
Patients may need to stop certain medications before the procedure. They should also have someone accompany them home after the injection.
Can cervical ESI injections be repeated if necessary?
Yes, injections can be repeated if needed. The frequency and number depend on individual patient needs.
References
- Benzon, H. T., Huntoon, M. A., Rathmell, J. P., & American Academy of Neurology (AAN) Panel. (2023, December). Epidural Steroids for Cervical and Lumbar Radicular Pain: A Systematic Review and Meta-Analysis. Neurology. https://pubmed.ncbi.nlm.nih.gov/39938000/