Hemophilia is a genetic disorder that makes it hard for the body to form blood clots. It affects thousands of people worldwide. A lot of people with hemophilia face serious problems that can shorten their lives. Thanks to new treatments, life expectancy for those with hemophilia has gotten better.
It’s important to know what hemophilia is and its possible complications. While there’s no cure, managing it well can greatly improve life quality for those affected.
Key Takeaways
- Hemophilia is a genetic disorder affecting blood clotting.
- Advancements in treatment have improved life expectancy.
- Proper management is key to a better life quality.
- Hemophilia complications can be serious and life-threatening.
- Understanding hemophilia is essential for effective management.
Understanding Hemophilia: A Blood Clotting Disorder
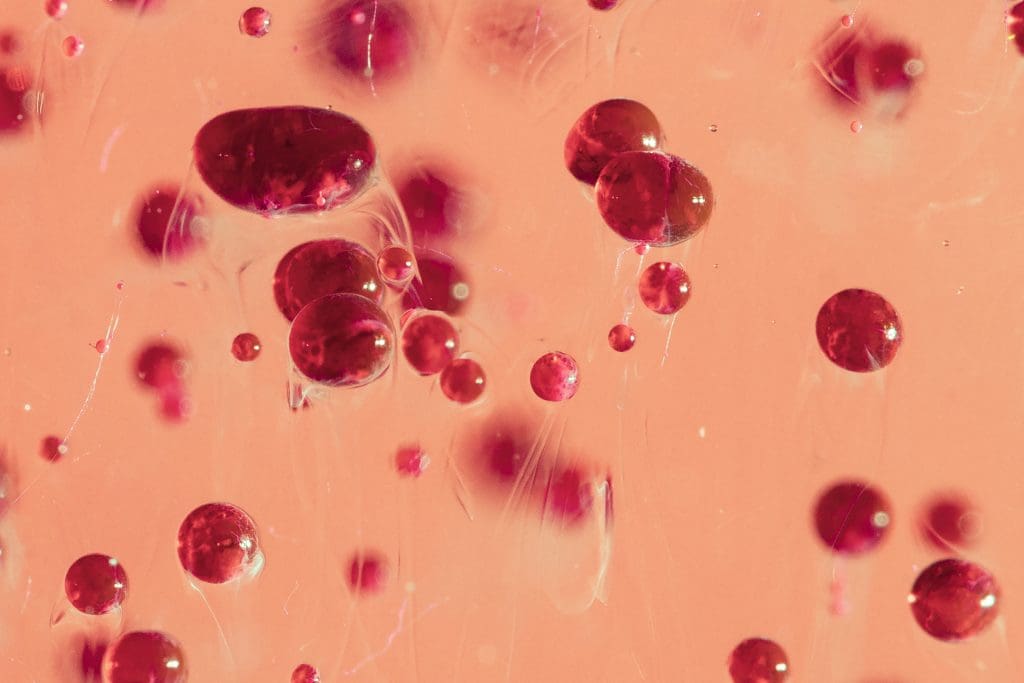
Hemophilia is a complex disorder that affects blood clotting. It’s caused by genetic factors. People with hemophilia can’t stop bleeding as easily as others.
The Mechanism of Blood Clotting
Blood clotting is a detailed process. It involves many proteins called clotting factors. When a blood vessel gets hurt, these factors work together to form a clot.
The clotting process has three stages: initiation, amplification, and fibrin formation. Hemophilia A and B happen when there’s not enough factor VIII or IX. These are key for clotting.
| Clotting Factor | Associated Condition | Role in Clotting |
| Factor VIII | Hemophilia A | Crucial for the amplification stage of clot formation |
| Factor IX | Hemophilia B | Essential for the amplification stage of clot formation |
Genetic Basis of Hemophilia
Hemophilia is caused by genetic mutations. These mutations affect the genes for clotting factors VIII and IX. This can lead to a non-functional or missing protein, causing bleeding.
The genetics of hemophilia are complex. It’s inherited in an X-linked recessive pattern. This means the genes are on the X chromosome.
Is Hemophilia a Sex-Linked Disease?
Yes, hemophilia is a sex-linked disease. The genes for clotting factors VIII and IX are on the X chromosome. Males are more likely to have hemophilia because they have only one X chromosome.
Females can be carriers. They might have mild symptoms. Understanding the genetics is key for managing hemophilia.
Types and Classification of Hemophilia
Hemophilia is a genetic disorder with two main types and several rare forms. It’s classified based on the clotting factor that’s missing or not working right.
Hemophilia A (Factor VIII Deficiency)
Hemophilia A, also known as classic hemophilia, is caused by a lack of clotting factor VIII. It’s the most common type, making up about 80% of cases. Symptoms include frequent bruising, joint pain, and prolonged bleeding.
Hemophilia B (Factor IX Deficiency)
Hemophilia B, also known as Christmas disease, is caused by a lack of clotting factor IX. It’s less common than Hemophilia A but has similar symptoms, like prolonged bleeding and joint damage. The treatment for Hemophilia B is similar to Hemophilia A, focusing on replacing the missing clotting factor.
Rare Forms of Hemophilia
Besides Hemophilia A and B, there are other rare forms of hemophilia, including:
- Hemophilia C: Caused by a deficiency in factor XI.
- Acquired hemophilia: A rare condition where antibodies develop against clotting factors.
These rare forms need specific diagnosis and treatment. They often require a team of healthcare professionals to manage.
Epidemiology: How Common is Hemophilia?
Understanding hemophilia’s spread is key to knowing its health impact. It’s a genetic disorder that makes blood clotting hard. It affects those with it and healthcare systems around the world.
Global Prevalence Statistics
About 1 in 5,000 males worldwide have hemophilia. It’s rare but has a big impact because it needs lifelong care. Without proper treatment, serious problems can happen.
Prevalence rates change in different places. This is because of genetics, how well doctors can diagnose, and how often it’s reported. Hemophilia A is more common than B globally.
Distribution Across Populations
Hemophilia’s spread varies by genetics. Some groups have more cases because of their genetic makeup. It’s mostly found in males because of how it’s inherited.
Women can also have hemophilia, but it’s rare. They might show symptoms if they have two affected X chromosomes. Research is growing to understand female cases better.
Hemophilia Registry Data
Hemophilia registries track its spread, treatment results, and problems. They help researchers, doctors, and policymakers improve care for those with hemophilia.
Registries show treatment has gotten better over time. This is thanks to new clotting factor therapies and better care plans. Keeping up with data is important for understanding and improving healthcare for hemophilia patients.
Severity Levels and Their Impact on Prognosis
Knowing the different severity levels of hemophilia is key to managing it well. The amount of clotting factor in the blood determines how severe it is. This affects how well someone with hemophilia can live and their quality of life.
Mild Hemophilia (5-40% Clotting Factor)
Mild hemophilia has clotting factor levels between 5% and 40% of normal. People with mild hemophilia might bleed after surgery, injuries, or dental work. But, they rarely bleed on their own.
The outlook for mild hemophilia is usually good. Most people with it can live active lives with little treatment.
Treatment Approach: Mild hemophilia often gets treated as needed. This means the clotting factor is given when it’s needed.
Moderate Hemophilia (1-5% Clotting Factor)
Moderate hemophilia has clotting factor levels between 1% and 5%. Those with it might bleed sometimes on their own, aside from after injuries or surgeries. How often they bleed can affect their life and treatment needs.
Prophylactic Treatment: For moderate hemophilia, regular treatment is sometimes suggested. This helps reduce how often they bleed.
Severe Hemophilia (Less than 1% Clotting Factor)
Severe hemophilia has clotting factor levels below 1%. People with severe hemophilia often bleed a lot, often into joints and muscles. This can cause long-term joint problems and disability if not treated right.
The outlook for severe hemophilia is tough. It needs a lot of treatment and careful watching.
| Severity Level | Clotting Factor Level | Bleeding Episodes | Prognosis |
| Mild | 5-40% | Rare, post-trauma or surgery | Good, minimal treatment |
| Moderate | 1-5% | Occasional spontaneous | Variable, prophylaxis may be used |
| Severe | <1% | Frequent spontaneous | Requires intensive treatment |
A leading hematologist says, “The severity of hemophilia greatly affects treatment and outlook. Knowing these differences is key to managing it well.”
“The different levels of hemophilia help tailor treatments to each person. This improves their life quality.”
” Expert in Hematology
The severity of hemophilia greatly affects how well someone can live. Understanding each level’s needs helps doctors give better care. This improves life for those with hemophilia.
Historical Perspective: The “Royal Disease”
Hemophilia, known as the “Royal Disease,” has a long history with European royal families. It’s a condition where blood can’t clot properly. This has been a big health problem for royalty for centuries.
Hemophilia in European Royal Families
Hemophilia is well-known in European royal families, like the British and Russian ones. Queen Victoria, who had hemophilia, spread it to many families through her kids.
Queen Victoria’s descendants married into many royal families. This meant hemophilia spread to Spain, Germany, and Russia, among others.
Historical Treatment Limitations
Old treatments for hemophilia were very limited. They often didn’t work well, leading to a lot of suffering and death. Before modern treatments, doctors could only try blood transfusions and keeping patients in bed.
Without good treatments, people with hemophilia had many bleeding episodes. This caused lasting damage to their joints and other problems.
Famous People with Hemophilia
Many famous people have had hemophilia. Tsarevich Alexei Nikolaevich of Russia, the son of Tsar Nicholas II, is one example. His condition was a big deal for the Russian royal family.
Another well-known person is Ryan White, an American boy. He became famous for his fight against AIDS and for helping people with hemophilia.
Life-Threatening Complications of Hemophilia
It’s important to know about the serious problems that can happen with hemophilia. This genetic disorder makes it hard for blood to clot. If not treated right, it can cause severe and even deadly issues.
Intracranial Hemorrhage
Intracranial hemorrhage is a very serious problem. It happens when blood bleeds inside the brain. This can be due to a small head injury or even just because the blood doesn’t clot right. Quick action is needed to avoid brain damage or death.
Symptoms of Intracranial Hemorrhage:
- Severe headache
- Confusion or altered mental status
- Nausea and vomiting
- Seizures
- Weakness or numbness in parts of the body
Gastrointestinal and Internal Bleeding
Bleeding in the stomach and inside the body is another big problem. It can happen anywhere and is very dangerous if not treated fast.
| Type of Bleeding | Common Symptoms | Treatment Approach |
| Gastrointestinal Bleeding | Abdominal pain, black tarry stools, vomiting blood | Factor replacement therapy, endoscopy |
| Internal Bleeding | Pain and swelling in the affected area, decreased hemoglobin levels | Factor replacement therapy, supportive care |
Throat and Neck Bleeding
Bleeding in the throat and neck is very dangerous. It can block the airway, which is a big emergency. Signs include trouble swallowing, swelling in the neck, and voice changes.
Dealing with these serious issues needs a full plan. This includes regular treatment to prevent bleeding, quick action when it happens, and watching for early signs. By knowing these risks and acting early, people with hemophilia can live longer and healthier lives.
Hemophilia Prognosis: From Past to Present
Thanks to new treatments, people with hemophilia now have a better outlook. In the past, hemophilia was very serious and often deadly. But today, thanks to modern medicine, patients are living longer and healthier lives.
Evolution of Treatment Approaches
Hemophilia treatment has changed a lot over the years. At first, doctors could only offer basic care. But in the 1960s, clotting factor concentrates were introduced, making it easier to manage bleeding.
Later, recombinant clotting factors made treatments safer and more available. Now, regular infusions of clotting factors are key to preventing bleeding.
Impact of Modern Therapies on Survival
Modern treatments have greatly improved life for those with hemophilia. They help reduce bleeding and lower the risk of serious problems like hemophilic arthropathy and intracranial hemorrhage.
| Treatment Era | Life Expectancy | Primary Causes of Mortality |
| Pre-clotting factor concentrates | Bleeding complications | |
| Clotting factor concentrates (1960s-1980s) | 50-60 years | Bleeding, HIV/AIDS |
| Recombinant clotting factors (1990s-present) | Near normal life expectancy | Cancer, cardiovascular disease |
Current Mortality Statistics
Even with all the progress, hemophilia is not without its challenges. Today, people with hemophilia can live almost as long as anyone else. But, certain health issues and complications can shorten their lives.
Studies show that while bleeding is a big concern, other health problems like cardiovascular disease and cancer are becoming more common causes of death in people with hemophilia.
Joint Damage and Long-Term Complications
Hemophilia can cause long-term damage to joints, known as hemophilic arthropathy. This happens because of repeated bleeding into the joints. It leads to inflammation, pain, and permanent damage.
Mechanism of Hemophilic Arthropathy
Blood builds up in the joints, causing inflammation and swelling. Over time, this damages cartilage and bone. It results in chronic pain and limited movement.
Key factors contributing to hemophilic arthropathy include:
- Recurrent hemarthrosis (bleeding into the joints)
- Synovial inflammation and hypertrophy
- Cartilage and bone destruction
Impact on Mobility and Quality of Life
Joint damage greatly affects mobility and quality of life for those with hemophilia. Chronic pain and reduced joint function limit daily activities. Prophylactic treatment and physical therapy are key to managing these issues.
Effective management strategies include:
- Regular factor replacement therapy
- Physical therapy to maintain joint mobility
- Pain management techniques
Secondary Complications from Joint Damage
Advanced hemophilic arthropathy can cause chronic pain, muscle weakness, and reduced range of motion. These issues can lower quality of life and increase the risk of other health problems like osteoporosis and fractures.
Addressing these complications requires a thorough approach, including:
- Multidisciplinary care involving hematologists, orthopedic specialists, and physical therapists
- Advanced imaging techniques to monitor joint health
- Surgical interventions when necessary
Inhibitor Development: A Serious Complication
Inhibitors are a big problem in managing hemophilia. They make it hard to treat bleeding episodes. These are antibodies that the immune system makes when it sees clotting factor concentrates as foreign.
What Are Inhibitors in Hemophilia?
Inhibitors are the body’s way of fighting off what it sees as a foreign substance”the clotting factor. When someone with hemophilia gets inhibitors, these antibodies block the clotting factor. This makes treatment less effective or even useless.
This makes managing hemophilia very hard. It limits the treatment options for bleeding episodes.
Risk Factors for Inhibitor Development
There are several things that can increase the risk of getting inhibitors. These include genetic factors and how often treatment is given. People with severe hemophilia A are more likely to get inhibitors.
Key risk factors for inhibitor development include:
- Genetic mutations that lead to severe hemophilia A
- Intensity and frequency of clotting factor replacement therapy
- Family history of inhibitors
- Ethnicity, with some studies suggesting variability in inhibitor risk among different ethnic groups
Severe Hemophilia A with Inhibitor: Prognosis
For those with severe hemophilia A and inhibitors, the outlook is tough. The presence of inhibitors makes it hard to manage bleeding episodes. This can lead to more problems, like joint damage and other issues from uncontrolled bleeding.
Management strategies include using bypassing agents and immune tolerance induction (ITI) therapy. These aim to get rid of the inhibitors or find ways to manage bleeding despite them.
Life Expectancy with Hemophilia in the Modern Era
Thanks to better healthcare, people with hemophilia are living longer and healthier lives. This is mainly because of new treatments and care plans.
Current Life Expectancy Statistics
Recent studies show a big jump in life expectancy for those with hemophilia. Hemophilia life expectancy statistics now say patients can live into their 60s and beyond. This is a big change from before.
Factors Affecting Longevity
Many factors affecting longevity in hemophilia have been found. These include:
- Access to modern clotting factor replacement therapies
- Prophylactic treatment regimens
- Comprehensive care through specialized hemophilia treatment centers
- Advances in gene therapy and other innovative treatments
Comparison with General Population
When comparing hemophilia life expectancy to the general population, a gap remains. But, the gap is getting smaller. New treatments have brought hemophilia patients’ life expectancy closer to the general population, mainly for those with mild or moderate hemophilia.
As treatment options and care strategies keep getting better, life expectancy with hemophilia will likely improve even more. This offers hope for a nearly normal lifespan for those with this condition.
Special Considerations: Women and Hemophilia
Hemophilia affects more than just males. Females can carry the condition and show symptoms due to genetic factors. It’s important to understand the role of women in hemophilia for better care.
Female Carriers and Symptoms
Female carriers of hemophilia usually don’t show symptoms or have mild ones. They have two X chromosomes, one with a normal gene that helps balance the other defective gene. But, some may show symptoms due to:
- Lyonization: When one X chromosome is turned off. If the normal gene is turned off, symptoms can appear.
- X-chromosome abnormalities: Changes in the X chromosome can cause hemophilia in females.
- Inheritance of two defective X chromosomes: Though rare, a female can have two bad X chromosomes, leading to hemophilia.
Diagnosis Challenges in Women
Diagnosing hemophilia in women is hard because symptoms vary and many carriers don’t show them. Challenges include:
- Genetic testing: Finding the hemophilia gene mutation is key for diagnosis.
- Clotting factor assays: Testing clotting factors VIII and IX can diagnose hemophilia A and B.
- Symptomatic evaluation: Checking bleeding symptoms and history is vital for diagnosing hemophilia in females.
Female Hemophilia Statistics and Outcomes
While hemophilia is more common in males, females face unique challenges. Female hemophilia statistics are less common, but studies show:
- Hemophilia is much less common in females than in males.
- Female carriers are at higher risk of bleeding during menstruation and childbirth.
- With the right care, females with hemophilia can live active lives, needing specialized care.
It’s vital to understand hemophilia in women for proper care and support. More research and awareness are needed to help female carriers and those with hemophilia.
Modern Treatment Approaches and Survival Rates
Hemophilia treatment has changed a lot with new methods. These changes have made life better for those with hemophilia. They have also helped people live longer.
Factor Replacement Therapies
Factor replacement therapy is key in treating hemophilia. It adds the missing clotting factor to the blood. There are two types: prophylactic and on-demand.
Prophylactic treatment stops bleeding before it starts. On-demand treatment stops bleeding when it happens.
New factor products are safer and work better. They are made with genetic engineering. This makes them safer from diseases.
Non-Factor Replacement Options
New treatments are being tried for hemophilia. emicizumab is one. It helps blood clot like factor VIII. It works well for hemophilia A, with or without inhibitors.
Other treatments are being looked at too. They target different parts of clotting. These could help those who can’t use traditional treatments.
Gene Therapy: Changing the Prognosis
Gene therapy could cure hemophilia. It puts a working gene in cells. This lets the body make the missing clotting factor.
First tests show promise. Patients are getting better and bleeding less. Gene therapy could change hemophilia treatment forever.
Managing Hemophilia: The Patient Journey
Managing hemophilia well needs a team effort. This includes care centers, custom treatment plans, and smart surgery choices. This approach is key to better lives for those with hemophilia.
Comprehensive Care Centers
Comprehensive care centers are essential for hemophilia management. They have teams of experts like hematologists and nurses. These teams offer complete care to patients.
- Access to specialized care and the latest treatment options
- Personalized treatment plans tailored to the individual needs of each patient
- Coordination of care across different disciplines to ensure complete support
Prophylactic vs. On-Demand Treatment
Hemophilia treatment falls into two main types: prophylactic and on-demand. Prophylactic treatment stops bleeding before it starts. On-demand treatment is for when bleeding happens.
Prophylactic treatment helps prevent bleeding and joint damage. It’s best for those with severe hemophilia.
On-demand treatment is for mild or moderate hemophilia. It treats bleeding as it happens.
Surgical Considerations for Hemophilia Patients
Surgery for hemophilia patients needs careful planning. This includes:
- Checking the patient’s bleeding risk before surgery.
- Using clotting factor concentrates before, during, and after surgery.
- Watching for bleeding or complications after surgery.
With the right care, treatment, and surgery planning, patients with hemophilia can have better outcomes. Healthcare teams play a big role in this.
Conclusion: The Future Outlook for Hemophilia Patients
Hemophilia patients have seen a big improvement in their outlook. This is thanks to better treatments and care. New research and therapies are on the horizon, promising even more progress.
New treatments like gene therapy and advanced factor replacement are changing how we manage hemophilia. These advancements could lead to a better life and longer life for those with the condition.
The future for hemophilia patients is looking brighter. Thanks to ongoing research and new treatments, their health and quality of life are set to improve. This is a positive sign for the hemophilia community.
FAQ
What is hemophilia?
Hemophilia is a genetic disorder. It makes it hard for the body to make blood clots. Blood clots are needed to stop bleeding.
Is hemophilia a sex-linked disease?
Yes, it is. Hemophilia mostly affects males. This is because it is linked to the X chromosome.
What causes hemophilia disease?
It’s caused by genetic mutations. These mutations lead to a lack of clotting factors. The main factors affected are factor VIII (Hemophilia A) and factor IX (Hemophilia B).
What are the different types of hemophilia?
There are mainly two types. Hemophilia A is caused by a lack of factor VIII. Hemophilia B is caused by a lack of factor IX. There are also rare types.
How common is hemophilia?
It’s rare. Hemophilia A affects about 1 in 5,000 male births. Hemophilia B affects about 1 in 20,000 male births.
What is the life expectancy of someone with hemophilia?
With today’s treatments, people with hemophilia can live almost as long as anyone else. But, some complications can shorten their life.
Can females have hemophilia?
Yes, but it’s rare. Females can have hemophilia if they have two copies of the mutated gene or certain genetic conditions.
What are inhibitors in hemophilia?
Inhibitors are antibodies. They develop in some people with hemophilia. These antibodies can stop clotting factor replacement therapies from working.
How does hemophilia affect quality of life?
It can greatly affect quality of life. Poor management can lead to joint damage and mobility problems.
What is the prognosis for someone with hemophilia?
The prognosis has greatly improved. Modern treatments allow most people with hemophilia to live active lives with managed symptoms.
What are the life-threatening complications of hemophilia?
Serious complications include intracranial hemorrhage and severe internal bleeding. Throat and neck bleeding are also life-threatening and need immediate medical help.
How has the treatment of hemophilia evolved?
Treatment has changed a lot. It now includes factor replacement therapies, non-factor replacement therapies, and gene therapy. These advancements have greatly improved outcomes.
What is hemophilic arthropathy?
Hemophilic arthropathy is joint damage from repeated bleeding into the joints. It leads to chronic pain and mobility issues.
Can males be carriers of hemophilia?
Males can’t be carriers in the usual sense. They have only one X chromosome. But, they can pass the mutated gene to their daughters, making them carriers.
What is the role of comprehensive care centers in managing hemophilia?
These centers offer a wide range of care. They include hematologists, orthopedic specialists, physical therapists, and social workers. They help manage hemophilia in a complete way.
What is gene therapy’s potentia in treating hemophilia?
Gene therapy aims to fix the genetic problem. It introduces a healthy copy of the defective gene into the patient’s cells. This could cure hemophilia or greatly reduce the need for factor replacement therapies.




































