
Bisphosphonate medication is a key part of treating osteoporosis. It has been shown to work well over many years. This is thanks to lots of clinical studies.Guide on how to use bisphosphonate medication correctly and safely for long-term osteoporosis management.
Bones that are thin or fragile are more likely to break. Osteoporosis treatment often includes bisphosphonates. They help slow down bone loss and lower the chance of fractures.
It’s important to know how bisphosphonates work. This knowledge helps people make better choices for their bone health. By using this medication, people can manage their osteoporosis better and avoid fractures.
Osteoporosis is a condition where bones become weak and break easily. It often goes unnoticed until a bone breaks. This can greatly affect a person’s life quality.
Osteoporosis happens when bones are broken down faster than they are made. Normally, bones are constantly being rebuilt. But in osteoporosis, the breakdown wins, leading to weaker bones.
Many things can cause osteoporosis, like hormonal changes and genetics. Lifestyle choices, like diet and exercise, also play a role. Knowing these factors helps in finding ways to manage the disease.
Osteoporosis can greatly lower a person’s quality of life, mainly after a fracture. Fractures can cause long-term pain and make it hard to move. They can also make a person feel scared and sad.
It’s not just physical health that suffers. Osteoporosis can also hurt a person’s mental and social well-being. Managing osteoporosis well is key to avoiding fractures and keeping overall health.
|
Aspect of Quality of Life |
Impact of Osteoporosis |
|---|---|
|
Physical Health |
Increased risk of fractures, chronic pain, disability |
|
Mental Health |
Anxiety, depression, fear of fractures |
|
Social Well-being |
Loss of independence, reduced social interaction |
Starting treatment early is key to managing osteoporosis. Early treatment can slow down bone loss. Bisphosphonates are important medicines for this.
Early treatment can greatly lower the risk of fractures and improve life quality. It’s important to catch and treat those at risk early to avoid serious problems later.
Bisphosphonates are drugs used to treat osteoporosis and other bone diseases. They work by stopping bone breakdown. This makes them key in managing osteoporosis.
The history of bisphosphonates started in the 19th century. But, they were first used in medicine in the late 20th century. They were first used in industry before being found to affect bone metabolism.
Research led to the development of bisphosphonates as medicines. This research focused on how they work and their use in treating bone diseases. Over time, new bisphosphonates were made, each better and safer.
Bisphosphonates are divided into two main types: nitrogen-containing and non-nitrogen-containing. Nitrogen-containing bisphosphonates, like alendronate and zoledronic acid, are more effective. They are often chosen for treating osteoporosis.
These drugs come in tablets and injections. This gives patients more options for treatment.
Bisphosphonates are key in fighting osteoporosis. They stop bone breakdown, which increases bone density. This reduces the chance of fractures.
Bisphosphonates play a big role in osteoporosis treatment. They help prevent fractures in people at high risk. Their effectiveness and safety are backed by lots of research.
Bisphosphonates work by stopping bone breakdown, which is key in treating osteoporosis. They are a type of medication used to prevent fractures in people with osteoporosis.
Bisphosphonates bind to bone, focusing on areas where bone is being remade. They then get inside osteoclasts, the cells that break down bone. This stops these cells from working.
The mevalonate pathway is important for making cholesterol and isoprenoids. Bisphosphonates block this pathway by stopping the enzyme FPPS. This stops the prenylation of GTPases, which is needed for osteoclasts to work and survive.
By blocking the mevalonate pathway, bisphosphonates reduce osteoclast activity. This leads to less bone breakdown. With less breakdown, bone mass increases, making bones stronger and reducing fracture risk.
This reduction in bone breakdown also makes bisphosphonates effective in the long term. They help keep bone density and structure, preventing osteoporosis complications.
Osteoporosis treatment often uses bisphosphonates. They come in different dosages and ways to take them. This helps doctors find the best treatment for each patient, making it easier to stick to the plan and get better results.
Alendronate and Risedronate are two oral bisphosphonates doctors often prescribe. They are taken once a week or month, depending on the type. Studies show they can greatly lower the chance of bone fractures.
Ibandronate comes in oral and intravenous forms. The oral version is taken once a month. The intravenous form is given every three months.
Zoledronic acid is given intravenously once a year. It helps ensure patients stick to their treatment and lowers fracture risk. It’s great for those with severe osteoporosis or trouble with oral bisphosphonates.
When looking at different bisphosphonates, we consider how well they prevent fractures and increase bone density. This helps doctors choose the best option for each patient.
|
Bisphosphonate |
Administration Route |
Dosing Frequency |
|---|---|---|
|
Alendronate |
Oral |
Weekly |
|
Risedronate |
Oral |
Weekly/Monthly |
|
Ibandronate |
Oral/IV |
Monthly/3 Monthly |
|
Zoledronic Acid |
IV |
Annual |
Bisphosphonates are key in fighting osteoporosis, thanks to lots of research. They help lower the risk of fractures and boost bone health. Many studies have shown their effectiveness.
Many trials have proven bisphosphonates cut fracture risk in osteoporosis patients. For example, alendronate has cut vertebral and non-vertebral fractures by up to 50% in postmenopausal women.
Key findings from major studies:
|
Study |
Bisphosphonate |
Fracture Risk Reduction |
|---|---|---|
|
FIT Study |
Alendronate |
47% reduction in vertebral fractures |
|
HORIZON Study |
Zoledronic Acid |
70% reduction in vertebral fractures |
Bisphosphonates not only lower fracture risk but also boost bone mineral density (BMD). They increase BMD at sites like the lumbar spine and hip.
For example, risedronate has been shown to increase BMD by up to 5% over three years.
Many studies have looked at bisphosphonates’ long-term effects. They show these drugs are effective and safe for long use.
Long-term data highlights:
Bisphosphonates are used for more than just treating postmenopausal osteoporosis. They are a type of medication that helps prevent bone loss. This increases bone density.
Postmenopausal osteoporosis is a common reason for using bisphosphonates. After menopause, women lose estrogen. This leads to more bone loss and a higher risk of fractures. Bisphosphonates help lower the risk of fractures in these women.
Osteoporosis in men is also treated with bisphosphonates. While less common than in women, it can cause serious problems. These drugs help increase bone density and reduce fracture risk in men.
Long-term use of steroids can cause osteoporosis. Bisphosphonates are effective in treating this condition. They help by reducing bone loss.
Bisphosphonates are also used for Paget’s disease and hypercalcemia of malignancy. Paget’s disease involves abnormal bone growth. Bisphosphonates help manage symptoms. In hypercalcemia, they help lower calcium levels.
|
Condition |
Bisphosphonate Use |
Benefits |
|---|---|---|
|
Postmenopausal Osteoporosis |
Reduces bone resorption |
Increases BMD, reduces fracture risk |
|
Osteoporosis in Men |
Increases BMD |
Reduces fracture risk |
|
Glucocorticoid-Induced Osteoporosis |
Prevents bone loss |
Reduces fracture risk |
|
Paget’s Disease |
Reduces bone turnover |
Alleviates symptoms |
It’s important to know the risks of bisphosphonates for treating osteoporosis. These drugs are key in managing osteoporosis but come with dangers.
Some conditions make bisphosphonates unsafe. These include:
Some conditions might not completely rule out bisphosphonates but need careful thought and watch. These include:
Kidney disease is a big worry for those on bisphosphonates. Zoledronic acid, given by vein, is not okay for those with very low kidney function. For other bisphosphonates, doses might be changed or other treatments considered based on kidney health.
Doctors must weigh the benefits against the risks for each patient. They must think about the need for osteoporosis treatment and any dangers or precautions.
To get the most out of oral bisphosphonates, patients need to follow certain guidelines. It’s important to administer these medications correctly. This ensures they work well and safely for osteoporosis treatment.
Oral bisphosphonates should be taken on an empty stomach. This is usually in the morning with a full glass of plain water. The exact dosage and how often you take it will depend on your medication.
Always follow the dosing instructions given by your healthcare provider or pharmacist.
Don’t eat, drink, or take other medications for at least 30 minutes after taking oral bisphosphonates. Drinks like coffee and orange juice can affect how well the medication is absorbed.
|
Beverage |
Effect on Absorption |
|---|---|
|
Coffee |
Reduces absorption |
|
Orange Juice |
Decreases bioavailability |
|
Mineral Water |
May interfere with absorption |
After taking oral bisphosphonates, stay upright for at least 30 minutes. This can be sitting or standing. Avoid lying down or bending over to prevent esophageal irritation.
Staying upright is key to avoiding esophageal problems.
If you miss a dose, take it as soon as you remember. But if it’s almost time for the next dose, skip the missed one. Just stick to your regular schedule.
Don’t take two doses at once.
For those who can’t take oral bisphosphonates, IV treatment is a good option. Zoledronic acid is given through an IV in a clinic. This ensures a safe and controlled setting for treatment.
Before starting IV bisphosphonate therapy, patients get a detailed medical check-up. They check kidney function and dental health. This is to avoid problems like osteonecrosis of the jaw (ONJ).
Pre-treatment assessments are key. They help find any issues and make sure the patient is safe during the treatment.
The IV treatment happens in an outpatient clinic. The drug is given slowly, usually over 15 to 30 minutes for zoledronic acid.
While getting the treatment, doctors watch for any bad reactions. Symptoms like flu can happen.
After treatment, patients are watched for a bit to see if they have any immediate side effects. It’s important for them to drink plenty of water and know about possible side effects later.
Follow-up care is vital. It helps manage long-term side effects and checks if the treatment is working.
Bisphosphonates are usually safe, but they can cause side effects. It’s important to manage these side effects well. This helps keep treatment going and keeps patients healthy.
Oral bisphosphonates often cause stomach problems. These include dyspepsia, esophagitis, and abdominal pain. To lessen these issues, take the medicine with a full glass of water. Stay upright for at least 30 minutes after taking it.
Here’s a table with common stomach side effects and how to handle them:
|
Side Effect |
Management Strategy |
|---|---|
|
Dyspepsia |
Take medication with food or switch to IV administration |
|
Esophagitis |
Avoid lying down after taking medication, elevate head of bed |
|
Abdominal Pain |
Consider alternative medication or adjust dosing schedule |
IV bisphosphonates can cause acute phase reactions. These include flu-like symptoms, fever, and muscle pain. These usually happen in the first 24-48 hours after the infusion and often go away on their own.
Bisphosphonates can lead to serious issues like osteonecrosis of the jaw (ONJ) and atypical femoral fractures. ONJ is when the jaw bone is exposed and doesn’t heal. Atypical fractures are breaks in the thigh bone with little or no trauma.
To lower the risk of these problems, keep your teeth clean, see your dentist regularly, and tell your doctor if you notice anything unusual.
If you’re taking bisphosphonates, know when to seek help. Look out for severe stomach issues, allergic reactions, jaw pain, and thigh or groin pain.
Knowing about the side effects and complications of bisphosphonates helps patients work with their doctors. This way, they can manage these issues well and get the best results.
Keeping an eye on how well treatment works and its safety is key when using bisphosphonates for osteoporosis. Regular checks help doctors make the best treatment plans. This way, they can get the best results and lower risks.
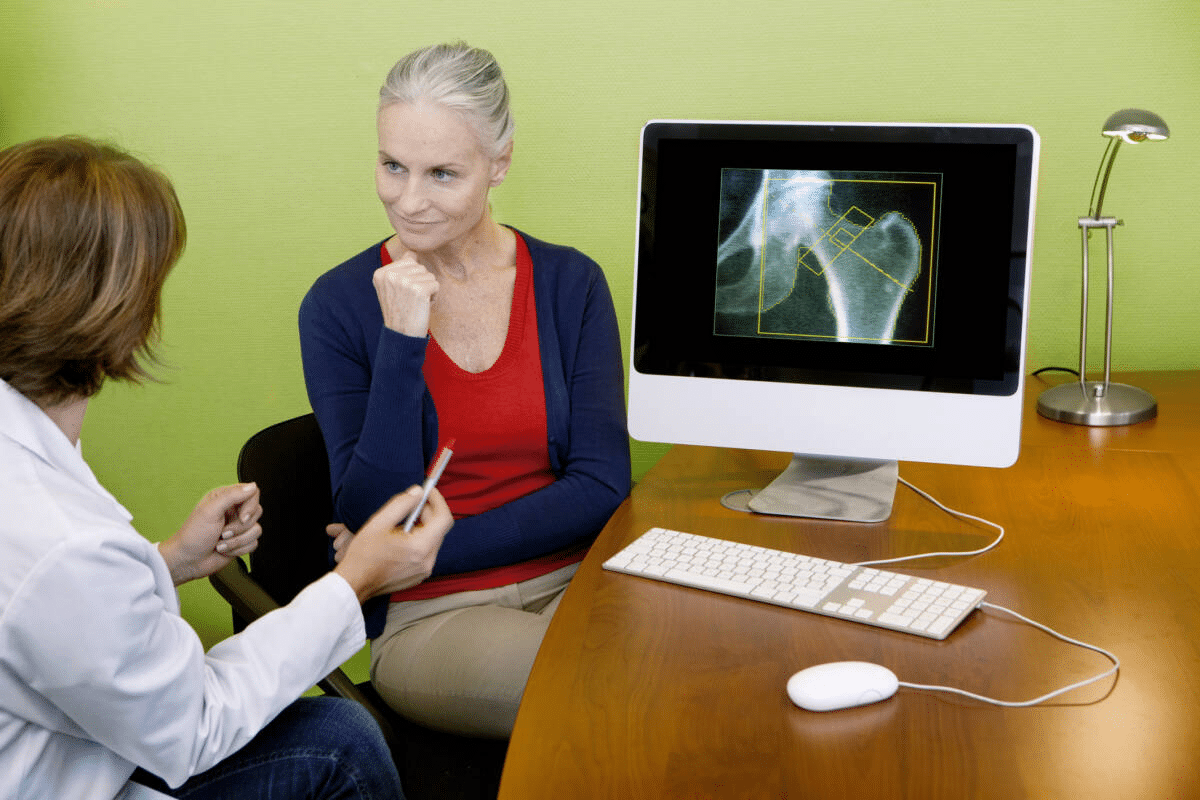
Bone mineral density (BMD) tests are vital for checking if bisphosphonates are working. How often these tests are done depends on several things. These include the patient’s starting BMD, risk factors, and how long they’ve been on treatment.
Usually, BMD tests are done when treatment starts and again after 1-2 years. After that, how often tests are needed depends on how the patient is doing and any changes in their risk factors.
|
Testing Interval |
Patient Profile |
Rationale |
|---|---|---|
|
Initial |
All patients starting bisphosphonate therapy |
Baseline assessment |
|
1-2 years |
Patients with high-risk profile or significant BMD changes |
Assess early response to therapy |
|
2-5 years |
Patients with stable BMD on long-term therapy |
Monitor long-term efficacy |
Biochemical markers of bone turnover give important info on how bisphosphonates work. These markers help see if treatment is working and if the patient is sticking to it.
Markers like serum C-telopeptide (CTX) and procollagen type 1 N-terminal propeptide (P1NP) are often used. Changes in these markers show if bisphosphonates are helping to slow down bone loss.
Regular dental checks are important because bisphosphonates can cause jaw problems. Patients should get dental care before starting treatment, and before any big dental work.
Preventive measures include:
Bisphosphonates are removed by the kidneys, and they can affect kidney health. It’s important to watch kidney function, even more so for those with kidney problems.
Doctors use serum creatinine and estimated glomerular filtration rate (eGFR) to check kidney health. If kidney function is bad, doctors might change the dose of bisphosphonates or choose a different treatment.
Bisphosphonate treatment and drug holidays are key in managing osteoporosis. The aim is to get the most benefits while avoiding risks.
The right time for bisphosphonate therapy varies by patient. Usually, it lasts 3 to 5 years. But, it can change based on bone density and fracture risk.
Long-term use of bisphosphonates can lower fracture risks. Yet, it might raise the chance of rare but serious issues like jaw problems and femur fractures.
A drug holiday means stopping bisphosphonate therapy for a while. It depends on the patient’s fracture risk and bone density.
Deciding to start bisphosphonates again after a break depends on several factors. These include fracture risk and bone density.
Important things to think about are:
Starting treatment again might be needed if bone density drops or fracture risk goes up.
Improving bisphosphonate therapy is key to better bone health. Knowing how to use it right, keeping an eye on side effects, and managing them well helps a lot. This way, patients can get the best results from their medication.
Getting the most out of bisphosphonate therapy means following a few steps. You need to take it as directed, check your bone density often, and handle any side effects that come up. It’s important to work closely with your doctor to make sure you’re getting the best treatment.
By following the advice in this article, you can make bisphosphonate therapy work better for you. This can lower your risk of fractures and help keep your bones strong. Remember, regular doctor visits and talking openly with your healthcare team are key to getting the best results.
Bisphosphonates stop bone resorption by affecting osteoclasts. They block the mevalonate pathway. This is key for osteoclast survival and function.
Bisphosphonates boost bone mineral density by cutting down bone resorption. This lets bone formation outpace resorption. This improves bone health overall.
Types include alendronate, risedronate, ibandronate, and zoledronic acid. Each has its own way of being taken and how often.
They’re used for postmenopausal osteoporosis in women and men. Also for osteoporosis caused by glucocorticoids, Paget’s disease, and high calcium levels.
Don’t use them if you have low calcium or are allergic to bisphosphonates. Avoid if you have severe kidney disease or certain stomach problems.
Take them on an empty stomach in the morning. Drink a full glass of water. Stay upright for 30 minutes after.
Side effects include stomach issues like dyspepsia and esophagitis. Intravenous use can cause acute reactions.
Monitor with bone density tests, markers of bone turnover, and fracture risk assessments.
It varies by patient. Usually, 3 to 5 years. Then, a break from the drug might be considered.
Yes, they can cause jaw osteonecrosis and atypical fractures. This highlights the need for careful patient monitoring.
Different bisphosphonates vary in potency and effectiveness. Some, like zoledronic acid, are more potent and easier to dose.
Patients with kidney disease need close monitoring of their kidney health. Adjust doses as needed to prevent kidney damage.
Consider a drug holiday after 3 to 5 years. This depends on the patient’s risk of fractures and bone density.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3513863/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!