Last Updated on November 25, 2025 by Ugurkan Demir
Chest pain is a common clinical symptom with many possible causes. These include heart, lung, stomach, muscle, and mental health issues. At Liv Hospital, we know how important it is to find the right cause of chest pain.
Chest pain doesn’t always mean a heart attack. But, it’s a serious sign that doctors check first. We’ll look at why chest pain happens, from heart problems to stomach issues or muscle pain.

Chest pain comes from a mix of factors. It involves nociceptors, neural pathways, and how the brain sees these signals. Pain can come from the heart, lungs, pleura, and muscles in the chest.
Pain in the chest starts with nociceptors feeling damage. These special receptors notice mechanical, thermal, or chemical harm. They send signals to the spinal cord and then to the brain, where it’s felt as pain.
The heart has these receptors too. They can feel pain from lack of blood flow or inflammation. The pleura and pericardium can also hurt due to inflammation or irritation.
Referred pain happens when pain feels like it’s coming from somewhere else. This is because different parts of the body send pain signals to the same spinal neurons. For example, pain from the diaphragm might feel like it’s in the shoulder or neck. Heart pain can feel like it’s in the arm or jaw.
Knowing about these patterns helps doctors figure out what’s causing chest pain. Things like heart attacks, lung clots, and inflammation around the heart have specific pain patterns. These patterns help doctors diagnose these conditions.
Understanding chest pain helps doctors tell serious problems from minor ones. This knowledge helps them choose the right treatment.
Assessing chest pain requires a detailed strategy. We start by taking a thorough medical history. This step is key to spotting serious conditions.
We ask specific questions to gather important info. These include:
Red flags like acute onset, severe intensity, or syncope mean we need to act fast.
Sorting out the risk level of acute chest pain is essential. We use tools and scores to group patients. This guides how we’ll check and treat them.
The HEART score is a common tool. It looks at history, ECG, age, risk factors, and troponin levels to sort patients.
Telling apart serious and harmless chest pain is key. Serious causes include heart attacks, blood clots, and aortic tears. Less serious causes might be muscle pain or acid reflux.
We use clinical checks, blood tests, and scans to figure this out. This way, we can spot and treat high-risk patients quickly.
By taking a detailed approach to chest pain, we can better identify and treat serious cases. This improves patient outcomes.
The physical exam is key in checking chest pain. It gives important clues for diagnosis and treatment. We use inspection, palpation, percussion, and auscultation, along with vital signs.
Inspection looks for signs of distress or oddities. We check for visible signs of respiratory distress like fast breathing or using extra muscles. Palpation feels the chest for tenderness or oddities.
We look for reproducible chest wall tenderness to spot musculoskeletal issues. During palpation, we also check for abnormal pulsations or heaves. These can hint at heart problems like ventricular hypertrophy or aneurysms.
Percussion taps on the chest to find underlying issues. We listen for dullness or hyper-resonance to spot conditions like pleural effusion or pneumothorax.
Auscultation listens to heart and lung sounds. We look for abnormal heart sounds like murmurs or rubs, and lung sounds like crackles or wheezes. These sounds help us understand cardiac and respiratory causes of chest pain.
Vital signs tell us about the patient’s health. We check heart rate, blood pressure, respiratory rate, and oxygen saturation. Odd readings can show how serious the issue is and guide treatment.
| Vital Sign | Normal Range | Significance in Chest Pain |
| Heart Rate | 60-100 bpm | Tachycardia or bradycardia can indicate cardiac or systemic causes |
| Blood Pressure | 90-120/60-80 mmHg | Hypertension or hypotension can suggest cardiovascular stress or shock |
| Respiratory Rate | 12-20 breaths/min | Tachypnea can indicate respiratory distress or disease |
| Oxygen Saturation | 95-100% | Hypoxemia can indicate respiratory or cardiac issues |
By combining findings from inspection, palpation, percussion, auscultation, and vital signs, we get a full picture of the patient’s health. This info is key in figuring out chest pain causes and how to treat it.
It’s important to know why chest pain happens to get the right treatment. Chest pain can be from many things, some serious and some not. We’ll look at the main reasons, which are heart-related and not heart-related, and how they show up differently in people.
Chest pain can come from two main areas: the heart or other parts of the body. Heart-related causes include things like heart attacks and inflammation around the heart. On the other hand, non-heart causes include stomach problems, muscle pain, and anxiety.
Cardiac Causes: These are linked to the heart’s health. Heart attacks and unstable angina are serious and need quick help. Other heart issues include inflammation of the heart sac and inflammation of the heart muscle.
Non-Cardiac Causes: These can be broken down further. Stomach issues like acid reflux are common. Muscle pain and anxiety can also cause chest pain.
| Cause | Category | Common Conditions |
| Cardiac | Cardiovascular | ACS, Pericarditis, Myocarditis |
| Non-Cardiac | Gastrointestinal | GERD, Esophageal Disorders |
| Non-Cardiac | Musculoskeletal | Costochondritis, Muscle Strains |
| Non-Cardiac | Psychological | Anxiety, Panic Disorders |
Chest pain can come on suddenly or over time. Sudden pain might mean a serious problem like a heart attack. Pain that lasts longer is often not as serious but can really affect your life.
Acute Presentations: These need quick action. They can be heart attacks, blood clots in the lungs, or air leaks in the chest. Severe pain that comes on fast needs to be seen right away.
Chronic Presentations: These might be from things like acid reflux, muscle pain, or anxiety. They’re not as urgent but can really impact your daily life.
Who gets chest pain can depend on age and gender. Younger people often have non-heart causes, while older folks are more likely to have heart problems. Some conditions are more common in one gender than the other.
Knowing these differences helps doctors give better care. It helps them figure out what’s going on and how to treat it.
Acute coronary syndrome (ACS) is a serious condition caused by a sudden drop in blood flow to the heart. It’s a major cause of illness and death worldwide. Quick and effective treatment is needed.
ACS happens when a plaque in a heart artery ruptures or erodes. This leads to a blood clot and blockage of the artery. It can cause a range of symptoms, from unstable angina to non-ST-elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI).
It’s important to know the symptoms of ACS. People often feel chest pain or discomfort that can spread to the arm, neck, or jaw. The pain feels like pressure or tightness. They might also feel dyspnea, nausea, or diaphoresis.
Knowing the risk factors and warning signs is key to catching ACS early. Risk factors include hypertension, hyperlipidemia, diabetes mellitus, smoking, and family history of heart disease. Warning signs that need urgent medical help include recurrent or worsening chest pain, syncope, or symptoms of heart failure.
| Risk Factor | Description | Impact on ACS Risk |
| Hypertension | High blood pressure | Increases risk due to vascular stress |
| Hyperlipidemia | Elevated levels of lipids in the blood | Contributes to plaque formation |
| Diabetes Mellitus | Chronic condition affecting blood sugar regulation | Enhances atherosclerotic process |
Managing ACS starts with medical therapy and timely intervention. Doctors use antiplatelet agents, anticoagulants, beta-blockers, and nitrates. Depending on the situation, they might do percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
Handling ACS well needs teamwork from emergency services, cardiology, and more. By understanding ACS, spotting symptoms, knowing risk factors, and using the right treatments, we can help patients better.
Vascular emergencies like pulmonary embolism and aortic dissection are serious and need quick medical help. They can cause chest pain and other symptoms that are not clear. This makes it hard to diagnose and treat them fast.
Pulmonary embolism is a serious issue for those with chest pain, trouble breathing, and fast breathing. It’s even more concerning if they have risk factors for blood clots. Symptoms can range from mild to severe, even leading to sudden heart stop.
Key symptoms and signs include:
To assess, doctors use clinical scores, D-dimer tests, and imaging like CT scans.
Aortic dissection happens when there’s a tear in the aorta’s lining. This lets blood flow between the aorta’s layers. It’s marked by severe chest pain that goes to the back.
Classic risk factors include:
Doctors use CT scans, TEE, or MRA to evaluate it.
Managing pulmonary embolism and aortic dissection starts with stabilizing the patient. For pulmonary embolism, treatment might include blood thinners and clot dissolvers. Aortic dissection treatment focuses on controlling blood pressure and heart rate, often leading to surgery.
Key management principles include:
It’s important to know the signs and how to diagnose pericarditis and myocarditis. These conditions can cause chest pain and need the right treatment to avoid serious problems.
Pericarditis often starts with sharp, stabbing chest pain. This pain gets better when sitting up and leaning forward. But, it gets worse when lying down or taking deep breaths. A doctor can tell if you have pericarditis by listening to your heart and looking at your ECG. Early treatment is very important.
Myocarditis can cause mild chest pain or even heart failure. Doctors look for signs of heart inflammation on MRI or biopsy. They also check for symptoms and signs of heart problems.
It’s key to tell pericarditis and myocarditis apart from heart attacks. Pericarditis has sharp pain and a rubbing sound in the chest. Myocarditis might seem like a heart attack at first, but it has different signs like heart problems and high inflammation markers.
For pericarditis, doctors often use medicines to reduce swelling and pain. Sometimes, they use steroids too. Myocarditis treatment focuses on helping the heart work better. It’s important to watch for any complications.
| Condition | Key Clinical Features | Diagnostic Tests | Treatment |
| Pericarditis | Pleuritic chest pain, pericardial friction rub | ECG, echocardiogram | NSAIDs, colchicine |
| Myocarditis | Chest pain, cardiac dysfunction | Cardiac MRI, biopsy | Supportive care, heart failure management |
Respiratory conditions like pneumonia and pneumothorax are big causes of chest pain. These issues can be serious and need quick attention for the right treatment.
Pneumonia can make chest pain worse when you breathe deeply or cough. This pain is sharp or pleuritic. It happens because the pleura, the lung’s covering, gets inflamed.
Key characteristics of pneumonia-associated chest pain include:
A pneumothorax is when air gets into the pleural cavity. It causes sudden chest pain and shortness of breath. The pain is sharp and might spread to the shoulder or back.
Clinical assessment for pneumothorax involves:
Treating pneumonia and pneumothorax needs different approaches. For pneumonia, antibiotics and supportive care like oxygen and hydration are used. Pneumothorax treatment depends on its size and symptoms, from watching it to using a chest tube.
General management principles include:
Non-emergency chest pain causes like GERD, musculoskeletal pain, and anxiety need the right diagnosis and treatment. These issues might not be life-threatening but can really affect a person’s life quality.
Gastroesophageal reflux disease (GERD) happens when stomach acid flows back into the esophagus. This can cause heartburn and chest pain. Lying down, eating big meals, or eating certain foods can make the pain worse.
Key characteristics of GERD-related chest pain include:
Costochondritis is when the cartilage between the ribs and sternum gets inflamed. Muscle strains can also cause chest pain. These usually happen from physical strain, injury, or doing the same thing over and over.
Characteristics of musculoskeletal chest pain:
Anxiety can make you feel chest pain or discomfort. You might also feel your heart racing, have trouble breathing, or feel like something bad is going to happen. This pain can come and go or stay for a while.
“Anxiety-related chest pain is often described as a tightness or squeezing sensation in the chest, which can be distressing for the patient.” – Medical Expert, Cardiologist
Management of anxiety-related chest pain involves:
Knowing about these non-emergency chest pain causes is key for doctors to give the right care and comfort to their patients.
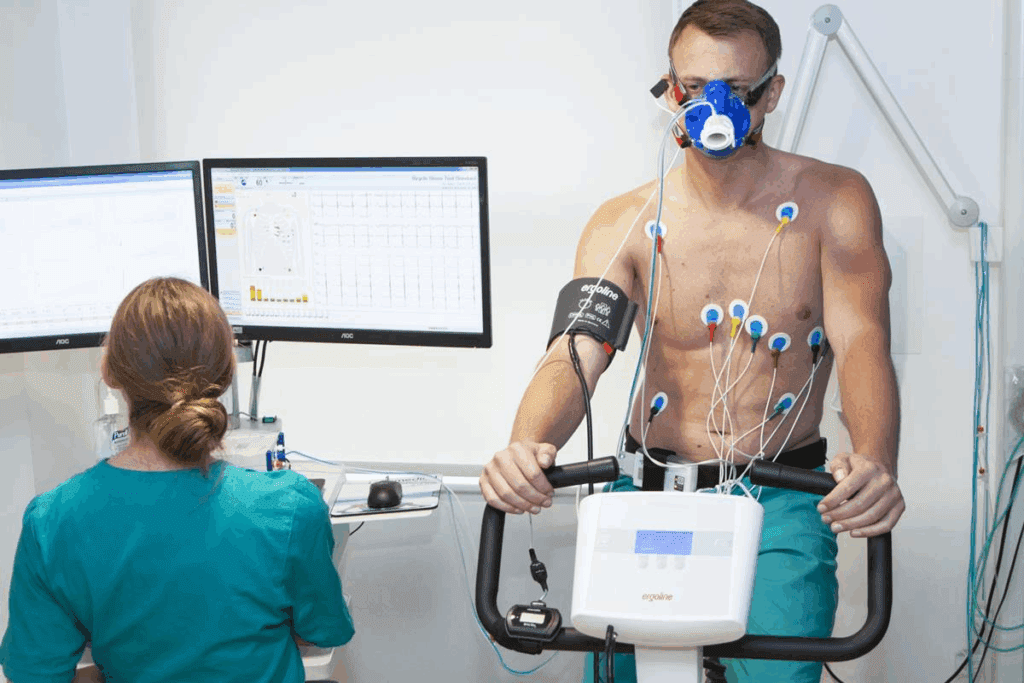
Healthcare providers use many tests to find the cause of chest pain. These tests help them decide the best treatment.
Laboratory tests are key in the first steps of checking chest pain. Important tests include:
| Laboratory Test | Primary Use in Chest Pain |
| Troponins | Diagnosing myocardial injury/ACS |
| D-dimer | Ruling out pulmonary embolism |
| BNP | Diagnosing heart failure |
Imaging studies are vital for seeing the heart, lungs, and nearby areas. They help find the cause of chest pain.
More tests might be needed based on the symptoms and first findings. These tests help find specific causes of chest pain.
It’s important for doctors to know how and when to use these tests. This helps them make the right diagnosis and treatment for chest pain patients.
Managing chest pain well needs a complete plan. This includes taking a detailed history, doing a physical exam, and using tests. Recent studies show the importance of starting the chest pain check early and focusing on it.
Healthcare workers can tell the difference between serious and not-so-serious chest pain. This helps them act quickly and correctly. We’ve talked about how chest pain can have many causes, from heart problems to other issues. This shows why understanding chest pain’s causes and how it shows up is key.
Managing chest pain effectively depends on using clinical skills wisely. This is backed up by tests that are proven to work. By using this method, doctors can improve how well patients do. This makes the care process smoother for those with chest pain.
Chest pain can stem from many sources. This includes heart problems like acute coronary syndrome. It can also come from non-heart issues like gastroesophageal reflux disease (GERD). Other causes include musculoskeletal pain and respiratory problems like pneumonia or pneumothorax.
Chest pain’s pathophysiology is complex. It involves how pain is perceived in the thorax. This includes the role of pain receptors and how pain signals reach the brain. It also involves referred pain from other areas.
A detailed approach to assessing chest pain is key. It helps spot life-threatening conditions. This involves a deep history, risk assessment, and distinguishing between high-risk and low-risk patients.
Examining chest pain involves several steps. These include inspection and palpation, percussion, and auscultation. Also, vital signs are checked. This gives valuable insights into the cause of chest pain.
Chest pain etiology is divided into heart and non-heart causes. Each has its own presentation and considerations based on age and gender.
Acute coronary syndrome is a serious heart-related cause of chest pain. It needs immediate attention. It has specific pathophysiology, clinical presentation, risk factors, and warning signs.
Pulmonary embolism and aortic dissection are serious vascular emergencies. They require quick recognition and evaluation. Specific presentation, assessment, and immediate management are key.
Pericarditis and myocarditis are inflammatory heart conditions. They have distinct clinical signs and diagnostic criteria. They need to be differentiated from acute coronary syndrome and treated appropriately.
Pneumonia and pneumothorax are respiratory causes of chest pain. They have specific presentations and need to be recognized and assessed. Management principles are also important.
Non-emergency causes of chest pain, like GERD, musculoskeletal pain, and anxiety-related chest pain, have unique characteristics. They require specific management approaches.
Tests for chest pain include lab tests like troponins, D-dimer, and BNP. Imaging tests like ECG, Chest X-ray, CT, and specialized tests are also used. They help diagnose specific causes.
Effective chest pain management combines clinical skills. This includes a detailed history, physical exam, and diagnostic tests. It provides a complete approach to assessment and management.
Risk stratification is critical in acute chest pain. It helps identify high-risk and low-risk patients. This guides further diagnosis and treatment.
Age and gender are important in diagnosing chest pain. Certain causes are more common in specific age groups or genders.
Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!