Last Updated on October 31, 2025 by

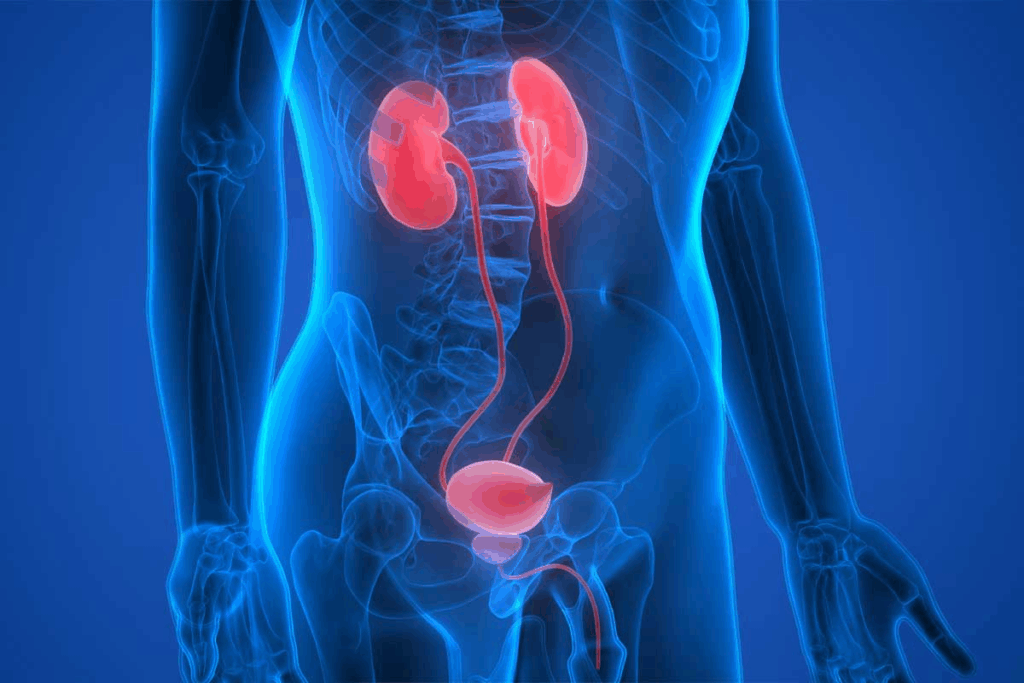
A prolapsed bladder happens when the bladder bulges into the vagina. This is called cystocele. It’s a type of pelvic organ prolapse, as the National Institute of Diabetes and Digestive and Kidney Diseases says.Fallen bladder surgery: A guide to the surgical procedures available to repair a cystocele (prolapsed bladder) and restore normal anatomy.
It’s important for patients to know about the treatment options, like bladder repair surgery. We’ll look at the different surgeries. We’ll also talk about the new, less invasive methods that help patients heal faster and have fewer problems.
At Liv Hospital, we mix top-notch surgical care with care that focuses on the patient. This ensures we give the best support to international patients getting bladder prolapse repair.

Learning about a prolapsed bladder means knowing its definition, how common it is, and what causes it. We’ll cover these points to give you a full picture of the condition.
A prolapsed bladder, also known as a cystocele, happens when the bladder bulges into the vagina. It’s a type of pelvic organ prolapse that can really affect a woman’s life.
Research shows that 3 to 6 percent of women have symptoms of pelvic organ prolapse. Up to 50 percent might have some prolapse when checked vaginally. The risk goes up with age, more so during and after menopause.
Many things can lead to a prolapsed bladder. Childbirth, getting older, and conditions that raise abdominal pressure are big factors. Weakened pelvic muscles and tissues also matter a lot.
The severity of bladder prolapse is measured in stages from 1 (mild) to 4 (severe). Knowing the stage helps figure out the best treatment.
Stage | Description |
1 | Mild prolapse, where the bladder is slightly displaced. |
2 | Moderate prolapse, where the bladder reaches the vaginal opening. |
3 | Severe prolapse, where the bladder protrudes beyond the vaginal opening. |
4 | Complete prolapse, where the bladder is fully outside the vagina. |
When thinking about prolapse of the bladder surgery or other treatments, knowing the stage and severity is key. Treatment choices often depend on how bad the prolapse is and the patient’s health.
Understanding symptoms and diagnosis is key to treating a prolapsed bladder. A prolapsed bladder, or cystocele, happens when the bladder bulges into the vagina. This can greatly affect a woman’s life.
The symptoms of a prolapsed bladder vary by severity. Common signs include:
These symptoms can greatly impact daily life. Recognizing them is key to getting the right medical care.
Diagnosing a prolapsed bladder involves a detailed medical check-up. The process starts with a pelvic exam to assess the prolapse. Other tests may include:
These tests help doctors understand the prolapse’s extent and its effect on bladder function.
A differential diagnosis is important to rule out other conditions. Healthcare providers look for other causes of pelvic discomfort or urinary symptoms. This ensures the treatment plan is effective.
If you’re experiencing symptoms of a prolapsed bladder, seek medical help. Early diagnosis and treatment can greatly improve outcomes. You should see a healthcare provider if you notice:
Timely medical attention can help manage symptoms and prevent complications.
Patients with a prolapsed bladder have many non-surgical options. These treatments can help manage symptoms and improve life quality.
Pelvic floor exercises, or Kegel exercises, are a first choice for many women. They strengthen the muscles that support the bladder and other organs.
Benefits of Pelvic Floor Exercises:
A pessary is a removable device for the vagina to support the bladder. There are different shapes and sizes, and a healthcare provider can help choose the right one.
Type of Pessary | Description | Benefits |
Ring Pessary | A circular device that supports the vaginal walls | Easy to insert and remove, effective for mild prolapse |
Gellhorn Pessary | A rigid, curved device that stays in place with suction | More supportive for advanced prolapse, less likely to shift |
Changing your lifestyle can also help with a prolapsed bladder. This includes staying at a healthy weight, avoiding heavy lifting, and managing chronic coughing or constipation.
Non-surgical treatments work for many, but not all. If symptoms don’t get better or get worse, surgery might be needed.
Indicators that conservative treatments are not working include:
To know if you need fallen bladder surgery, you must look at how bad the problem is. It’s about how it affects your daily life. Surgery is usually needed when symptoms are very bad or when other treatments don’t work.
Surgery for a prolapsed bladder is often needed when:
Surgical intervention aims to make symptoms better, fix the problem, and improve your life.
Before fallen bladder surgery, a detailed check-up is key. This includes:
This helps decide the best surgery for you and what to expect.
Talking openly with your doctor about surgery is very important. You should know what surgery you’ll have, what it can do, any risks, and how you’ll recover. Discussing surgery with your doctor helps you make a good choice and get ready for after the surgery.
It’s important to have realistic hopes for surgery. Surgery can really help, but it might not fix everything. Knowing what surgery can and can’t do helps you feel good about the results.
There are many ways to fix a prolapsed bladder through surgery. These methods are chosen based on what each patient needs. They fall into two main categories: vaginal and abdominal approaches. Each has its own benefits and when it’s best to use it.
Vaginal surgeries are often chosen because they are less invasive. This means patients can recover faster. Colporrhaphy is a common one where the vaginal wall is fixed. It can be done on the front (anterior) or back (posterior) of the vagina.
Using a pessary is another vaginal method. It’s not always a surgery, but a way to manage symptoms before or instead of surgery.
Procedure | Description | Recovery Time |
Anterior Colporrhaphy | Repair of the front vaginal wall | 2-4 weeks |
Posterior Colporrhaphy | Repair of the back vaginal wall | 2-4 weeks |
Abdominal surgeries, like sacrocolpopexy, involve opening the abdomen. This method is good for severe cases. It attaches the vaginal vault to the sacrum with a mesh.
These surgeries are more invasive than vaginal ones. But, they can last longer for some patients.
Procedure | Description | Recovery Time |
Sacrocolpopexy | Attachment of vaginal vault to sacrum using mesh | 4-6 weeks |
The use of surgical mesh in bladder prolapse repair has sparked a lot of debate. This medical device is used to support weakened tissues. We will look at the types of mesh, their benefits and risks, the FDA’s current status, and how they compare to non-mesh repairs.
There are different types of surgical mesh for bladder prolapse repair. Synthetic meshes are made from materials like polypropylene. Biological meshes come from animal tissues or human cadavers.
Using surgical mesh in bladder prolapse repair has its benefits. It can make the repair last longer and may reduce the chance of it happening again. But, it also has risks like mesh erosion, pain, and infection.
Benefits | Risks |
Improved durability | Mesh erosion |
Lower recurrence rates | Pain and discomfort |
Minimally invasive procedures | Infection |
The FDA has warned about using surgical mesh for pelvic organ prolapse, including bladder prolapse. This is because of reported complications. Even so, many surgeons recommend its use in certain cases.
Choosing between mesh and non-mesh repairs depends on several factors. These include the severity of the prolapse, the patient’s health, and the surgeon’s preference. Non-mesh repairs might have fewer complications but could have a higher chance of the prolapse coming back.
Deciding between mesh and other repair methods can be tough. Our healthcare team is here to help you make the right choice. We want to make sure you get the best care for your condition.
Costs and Insurance Coverage for Bladder Prolapse Surgery
It’s important for patients to understand the costs of bladder prolapse surgery. The costs can be high, and knowing about insurance and financial help is key.
In the U.S., the cost of fixing a prolapsed bladder is big. It adds up to about $1.523 billion each year. The price can change a lot based on the surgery type, the doctor’s fees, and where you live.
Factors influencing the cost include:
Most insurance plans cover bladder prolapse surgery. But, how much they cover can differ a lot. It’s good to check your policy to know what you’ll pay for.
It’s essential to:
When talking to your insurance about bladder prolapse surgery, ask these questions:
If you’re worried about money, there are help programs out there. These include:
Ask your doctor or insurance about these options. They can help you see if you qualify and how to apply.
Recovering from bladder prolapse surgery needs careful post-operative care and a slow return to normal activities. We’ll guide you through this process. It’s key to understand the stages for a successful recovery.
The first recovery phase is critical. Patients are watched in a recovery room for hours after surgery. It’s vital to follow the post-operative instructions from your healthcare team. These may include wound care, medication, and follow-up appointments.
Key aspects of immediate post-operative care include:
Pain management is a key part of recovery. Patients should follow their doctor’s pain medication instructions. This can change based on the surgery type. Good pain management helps patients move back to normal activities more easily.
“Adequate pain control is essential for a smooth recovery. Patients should be aware of their pain management options and discuss any concerns with their healthcare provider.”
Following activity restrictions after surgery is important. We advise avoiding heavy lifting, bending, or strenuous activities for weeks. Gradually increase activities with your healthcare provider’s guidance.
Some general guidelines for activity restrictions include:
The time to return to normal activities varies. It depends on the individual and surgery type. Expect a recovery of weeks to months. Always follow your healthcare team’s specific guidance for a successful recovery.
By carefully following post-operative instructions and adhering to activity restrictions, patients can optimize their recovery after bladder prolapse surgery.
Studies show that bladder prolapse surgery works well for many people. It helps with symptoms and makes patients happy. We look at how well surgery works by checking success rates, how often symptoms come back, and how life improves.
Research shows bladder prolapse surgery is very effective. Most patients see big improvements in their symptoms. This means they can live their lives better and feel better overall.
Many things can affect how well surgery works. These include the patient’s health, how bad the prolapse is, and the surgical method. The surgeon’s skill also matters a lot. We’ll dive deeper into these factors to understand what makes surgery successful.
Even though surgery is often successful, it’s not always permanent. How often symptoms come back depends on many things. We’ll look at the latest data to give you an idea of what to expect.
The main goal of surgery is to make life better. Studies show it can really help with feeling better physically and emotionally. Patients can do more things and feel more confident.
Knowing about success rates and what affects them helps patients choose the right treatment. We aim to give the best care and support for our patients having bladder prolapse surgery.
Treating a prolapsed bladder needs a detailed plan. This plan considers how bad the symptoms are and what the patient prefers. We’ve looked at many ways to treat it, from not needing surgery to using surgical mesh.
It’s key to talk to doctors to find the right treatment. Every person’s situation is different. So, a treatment plan made just for them is very important.
For serious cases, surgery might be needed. But, deciding to have surgery should be a careful choice. It’s important to think about your health, how bad the symptoms are, and the risks and benefits of surgery.
Knowing about all the treatment options and getting advice from doctors helps. This way, people with a prolapsed bladder can make good choices. It can really improve their life.
A prolapsed bladder happens when the bladder pushes into the vagina. This usually happens because the muscles in the pelvic area are weak. We’ll talk about what causes this and the risks involved.
You might feel like your pelvis is full or pressurized. You could also leak urine, have trouble emptying your bladder, or see a bulge in your vagina. We’ll go over these symptoms and when you should see a doctor.
Doctors use a physical exam, your medical history, and sometimes tests like imaging or urodynamic tests. We’ll explain how these steps help confirm the diagnosis.
Options include pelvic floor exercises, using pessary devices, and making lifestyle changes. We’ll discuss the good and bad sides of these methods.
Surgery is needed if symptoms are bad or if other treatments don’t work. We’ll talk about when surgery is a good choice and what happens before the surgery.
There are surgeries done through the vagina or abdomen, with or without mesh. We’ll cover the different methods and when they’re used.
Mesh is a material used to support the bladder. It can be helpful but also has risks. We’ll look at the types of mesh, their benefits and risks, and the FDA’s current view.
Costs vary based on where you are, your insurance, and the surgery type. We’ll give you an idea of costs, insurance help, and financial aid options.
Recovery includes immediate care, managing pain, and slowly getting back to normal. We’ll guide you through the recovery steps and timeline.
Success rates depend on the surgery and individual factors. We’ll share success statistics, what affects success, and how surgery can improve your life.
Yes, there’s a chance it could happen again. We’ll talk about what increases this risk and how to lower it.
Preparing means talking to your doctor, understanding the surgery, and following instructions. We’ll help you get ready for surgery.
Complications can include infection, bleeding, and issues with mesh. We’ll discuss these risks and how to avoid them
World Health Organization. (2025). References. Retrieved from https://www.who.int/publications/i/item/9789240049447
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!