Last Updated on November 14, 2025 by
Managing pediatric diabetes needs a detailed plan. This plan includes the latest medical tech, care tailored to each child, and education. Knowing the normal blood sugar levels in infants is key to managing it well.
Treatment for pediatric diabetes involves a team of experts. They work together to give insulin, check sugar levels in infants, and teach healthy habits. At LivHospital, we focus on creating care plans that meet each child’s specific needs.

We mix pediatric diabetes treatment methods with the latest tech and caring support. This way, we help kids stay healthy and live well. fasting blood sugar 20 months old may reveal pediatric diabetes. Learn about treatment, diet, and medical care options.
Key Takeaways
- Effective pediatric diabetes management requires a detailed approach.
- Understanding normal blood sugar levels in infants is key.
- A team of experts is vital for successful treatment.
- Custom care plans meet each child’s unique needs.
- Modern diabetes tech is a big part of treatment today.
Understanding Pediatric Diabetes: Types and Diagnosis
It’s important to know about pediatric diabetes early. Type 1 diabetes is a common condition in kids. It happens when the body can’t make insulin, leading to high blood sugar.

Differentiating Between Type 1 and Type 2 Diabetes in Children
Type 1 diabetes is when kids can’t make insulin. Type 2 diabetes is when the body doesn’t use insulin well. Knowing the difference helps doctors treat it right.
Each type of diabetes has its own signs. Type 1 diabetes shows sudden symptoms like extreme thirst, frequent urination, and weight loss. Type 2 diabetes might start slowly.
Early Signs and Symptoms Parents Should Know
Spotting early signs is key. Look out for high blood sugar, thirst, fluid loss, and blurred vision. Catching it early can make a big difference.
Diagnostic Criteria and Testing Procedures
Diagnosing diabetes in kids involves tests and doctor checks. Doctors use blood tests to see how much sugar is in the blood. They also look at how well the body makes insulin.
Knowing how doctors test for diabetes helps parents and doctors work together. This makes managing diabetes better for kids.
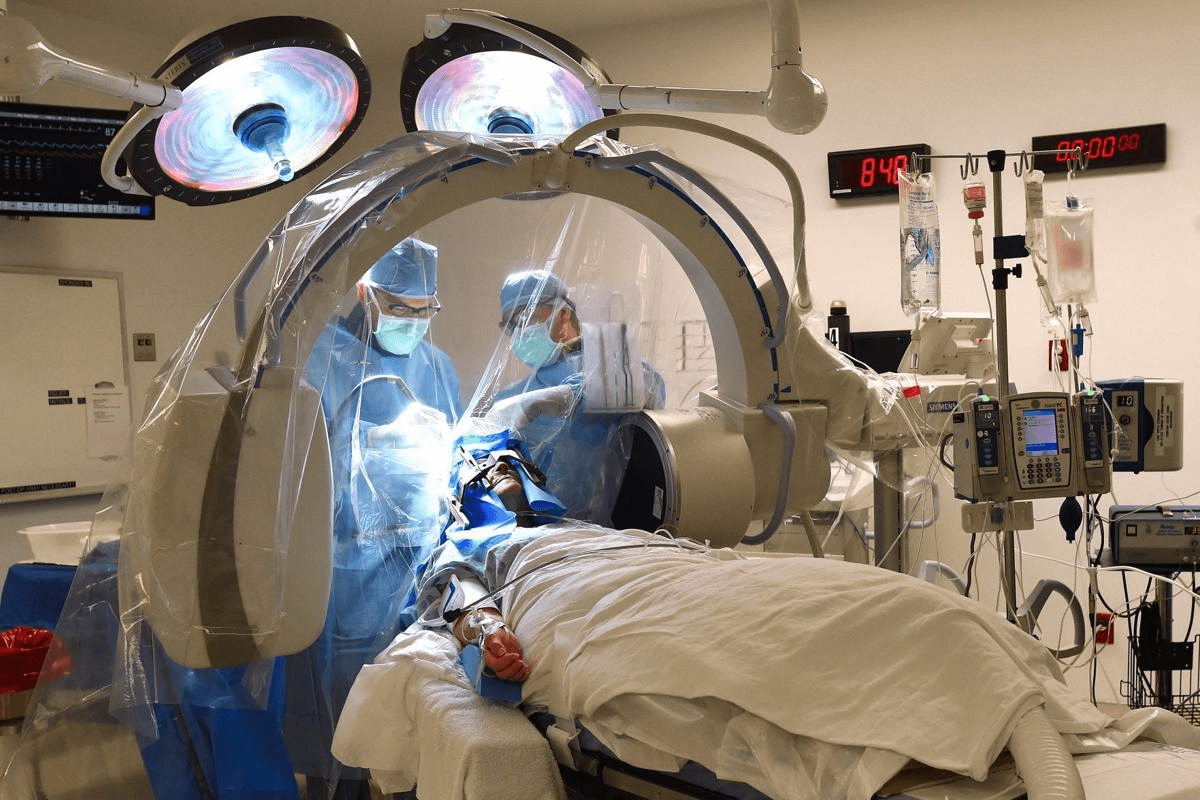
The Multidisciplinary Approach to Pediatric Diabetes Management
Managing pediatric diabetes needs a team of healthcare experts. We think a team effort is key for the best care for kids with diabetes.
The Pediatric Diabetes Care Team
A team of experts is essential for managing pediatric diabetes. This team includes doctors, diabetes educators, dietitians, and more. Each team member plays a vital role in diabetes care.
- Pediatric endocrinologists and healthcare providers who specialize in diabetes care
- Certified diabetes care and education specialists who educate families on diabetes management
- Registered dietitians who guide nutrition and meal planning
- Other specialists, such as mental health professionals and social workers, who support the family’s overall well-being
Importance of Coordinated Care
Coordinated care is key to managing pediatric diabetes. A team working together offers comprehensive and consistent care. This care meets the child’s medical, nutritional, and emotional needs.
Advances in diabetes technology, like continuous glucose monitors (CGMs), have greatly improved care. For example, the Omnipod 5 system has helped kids stay in the target glucose range more often.

Family Education and Support Systems
Teaching families is a big part of managing pediatric diabetes. We teach families how to manage their child’s diabetes. This includes monitoring blood glucose, giving insulin, and living a healthy lifestyle.
Support systems, like digital health tools and mobile apps, are also important. They help families manage their child’s diabetes. By giving families the knowledge and tools they need, we empower them to be active in their child’s care.
Some key aspects of family education include:
- Understanding normal glucose ranges for infants and young children
- Learning how to use diabetes technology, such as CGMs and insulin pumps
- Developing skills for managing diabetes during illness or special events
By using a team approach to manage pediatric diabetes, we can improve care. This approach helps kids with diabetes live better lives. It also supports families with the help they need.
Insulin Therapy: The Foundation of Type 1 Diabetes Treatment
Insulin therapy is key for managing type 1 diabetes in kids. It helps control blood sugar levels, which is vital for their health.
Types of Insulin Used in Pediatric Patients
Children with type 1 diabetes use different types of insulin. These include:
- Rapid-acting insulin: Works fast, within 15 minutes, and lasts 2 to 4 hours.
- Short-acting insulin: Starts working in 30 minutes and lasts 3 to 6 hours.
- Intermediate-acting insulin: Takes 1 to 2 hours to start and lasts 12 to 18 hours.
- Long-acting insulin: Works slowly and keeps blood sugar levels stable for 24 hours.
These insulins help doctors create personalized treatment plans for kids.
Insulin Delivery Methods for Children
There are several ways to give insulin to kids. Each method has its own benefits:
- Insulin pens: Portable and easy to use, great for kids.
- Insulin pumps: Give insulin all day and can dose up at meals.
- Tubeless pumps: Make insulin pump therapy easier without tubing.
- Syringes: A traditional way to give insulin, sometimes used.
The best method depends on the child’s needs and family preferences.
Calculating and Adjusting Insulin Doses
Finding the right insulin dose is important. It depends on:
- Carbohydrate intake: The amount of carbs you eat affects your blood sugar.
- Pre-meal blood glucose levels: This helps figure out the dose.
- Physical activity: Exercise can change blood sugar levels, so insulin doses might need to be adjusted.
Keeping blood sugar in check requires constant monitoring and adjustments. Doctors and families work together to make these changes.
Knowing about the different insulins, how they’re given, and how to adjust doses helps families manage type 1 diabetes. This improves the quality of life for kids with this condition.
Monitoring Fasting Blood Sugar in 20-Month-Olds and Other Young Children
It’s key to know what normal blood sugar levels are in babies and toddlers. This knowledge is vital for managing diabetes in young people. We face special challenges when checking blood sugar in very young kids.
Normal Blood Sugar Ranges for Infants and Toddlers
Children’s blood sugar levels change as they grow. For babies and toddlers, a normal fasting blood sugar is between 70 to 100 mg/dL. But these numbers can change based on diet, activity, and health.
Parents and caregivers need to work with their child’s diabetes team. They should learn the specific blood sugar goals for their child. Here are some general guidelines:
- Fasting blood glucose: 70-100 mg/dL
- Pre-meal blood glucose: 70-130 mg/dL
- Post-meal blood glucose (1-2 hours after eating): less than 180 mg/dL
Challenges of Blood Glucose Testing in Very Young Children
Testing blood sugar is important for diabetes care. But it’s hard in young children. Their age, size, and cooperation level can affect testing.
Some common issues include:
- It’s hard to get a blood sample because of small fingers or a lack of cooperation
- Keeping the child calm during testing
- Dealing with the emotional stress of frequent finger pricks
Interpreting Blood Sugar Results in Pediatric Patients
Understanding blood sugar results in kids requires a deep knowledge. Healthcare providers look at diet, activity, and medicine when checking blood sugar.
Important things to consider include:
- How food and insulin affect blood sugar
- Spotting patterns and trends in blood sugar data
- Changing treatment plans based on blood sugar data for better control
By teaming up with healthcare providers and staying updated on pediatric diabetes care, parents and caregivers can help their child manage diabetes well. This helps avoid diabetes-related problems.
Advanced Diabetes Technologies Transforming Pediatric Care
Advanced diabetes technologies are changing how we care for kids with diabetes. These new tools have greatly improved how well kids manage their blood sugar. They also make life better for young patients.
Continuous Glucose Monitoring Systems for Children
Continuous glucose monitoring (CGM) systems are key in managing diabetes in kids. They give real-time blood sugar readings. This helps parents and doctors make better choices about insulin and lifestyle.
CGM benefits include fewer fingerstick tests, better blood sugar control, and spotting trends early. It’s great for kids because it lowers the chance of low blood sugar.
Insulin Pump Therapy and Automated Insulin Delivery
Insulin pump therapy is a more flexible and precise way to give insulin than shots. For kids, pumps can give steady insulin all day and extra doses at meals.
Automated insulin delivery systems go further by linking CGM with insulin pumps. These systems adjust insulin as needed, giving kids the best blood sugar control with less effort.
Digital Health Tools and Mobile Applications
Digital tools and apps are helping kids manage their diabetes. They track blood sugar, insulin, and food, giving a full picture of diabetes care.
These tools also have reminders, data analysis, and sharing options. They help families stay involved and make better choices during doctor visits.
- Improved data tracking and analysis
- Enhanced patient engagement
- Better communication between families and healthcare providers
Using these advanced diabetes technologies can greatly improve care for kids with diabetes. It helps them live healthier, more active lives.
Treating Type 2 Diabetes in Youth: A Growing Challenge
Type 2 diabetes in young people is a big problem in pediatric care. It’s growing fast, and we need to find good ways to treat it. Young patients have special needs that we must focus on.
Dealing with type 2 diabetes in kids means more than just insulin. We must think about their health, lifestyle, and future risks. This helps us create a better treatment plan.
Medication Options Beyond Insulin
Insulin is key, but there are other medicines for type 2 diabetes in kids. These include:
- Metformin is often the first choice for kids with type 2 diabetes
- Sulfonylureas, which help the pancreas make more insulin
- DPP-4 inhibitors, which help control blood sugar
- GLP-1 receptor agonists, which help insulin work better
We can use these medicines alone or together to control blood sugar. It’s important to weigh the benefits and risks when planning treatment.
Nutrition and Physical Activity Interventions
Changing how kids eat and exercise is key in managing type 2 diabetes. Good nutrition and exercise can make insulin work better, lower blood sugar, and improve health.
We suggest a diet full of whole foods, fruits, and veggies, but low in sugars and fats. Kids should also do regular exercise like running and lifting weights. This helps with insulin sensitivity and health.
Early Aggressive Treatment to Prevent Complications
Starting treatment early is vital to avoid serious problems later. Tight blood sugar control early on can lower risks of serious health issues.
Aggressive treatment means using lifestyle changes and medicines together. We need to work with kids and their families to make a treatment plan that meets their needs. This helps them stay healthy.
Conclusion: Innovations and Future Directions in Pediatric Diabetes Care
Pediatric diabetes care is changing fast. New technologies and treatments are making a big difference. This means better care for kids with diabetes.
The market for treating diabetes in kids is growing. It’s expected to hit $40.2 billion by 2035. Places like LivHospital are leading the way in this progress.
Looking ahead, we’ll see even more changes. Things like continuous glucose monitoring and insulin pumps will become more common. We’re dedicated to top-notch healthcare and support for families around the world.
By using these new tools and working together, we can make a big difference. We aim to give kids with diabetes the best care and support possible.
FAQ
What are normal blood sugar levels in infants?
Infants’ blood sugar levels usually fall between 70-150 mg/dL. This range can change based on their age, if they’ve eaten, and their health. Newborns often have levels between 50-100 mg/dL in the first hours after birth.
How is type 1 diabetes diagnosed in children?
Doctors use several methods to find type 1 diabetes in kids. They look at the child’s medical history and do tests like fasting blood glucose tests. They also check for autoantibodies linked to type 1 diabetes.
What is the role of continuous glucose monitoring systems in pediatric diabetes management?
Continuous glucose monitoring systems are key for kids with diabetes. They give real-time glucose data and an alert for high or low levels. This helps manage blood sugar and prevent problems.
How is insulin therapy managed in pediatric patients with type 1 diabetes?
Kids with type 1 diabetes use insulin therapy. They might use insulin pumps or inject insulin several times a day. The doctor adjusts the dose based on diet, activity, and blood sugar.
What are the challenges of blood glucose testing in very young children?
Testing blood sugar in young kids is hard. It’s because of their age, size, and ability to cooperate. It also involves frequent testing and can be painful.
What are the benefits of a multidisciplinary approach to pediatric diabetes management?
A team approach to diabetes care is very helpful. It includes doctors, educators, dietitians, and mental health experts. This team provides complete care, education, and support, improving health and life quality.
How can digital health tools improve glycemic outcomes in children with diabetes?
Digital tools like apps and online platforms help with diabetes care. They track data, offer personalized advice, and improve communication with healthcare teams.
What is the normal glucose range for infants?
Infants’ normal blood sugar levels are 70-150 mg/dL. This can vary with age and feeding status. Newborns usually have levels between 50-100 mg/dL in the first hours after birth.
What are the early signs and symptoms of diabetes in children that parents should be aware of?
Look out for signs like increased thirst and urination, weight loss, and fatigue. Blurred vision and frequent infections are also warning signs. If you notice these, get medical help right away.
How does LivHospital support international patients with pediatric diabetes?
LivHospital offers top-notch care for kids with diabetes. They provide diagnosis, treatment, and management. They also support families with education, counselling, and care coordination.
References:
- ISPAD Clinical Practice Consensus Guidelines 2022. (2022). Pediatric Diabetes. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10108244/
- Consensus guidelines covering glycemic targets, monitoring, and pediatric diabetes care recommendations.
- “14. Children and Adolescents: Standards of Care in Diabetes ” 2025. (2025). Diabetes Care. Retrieved from https://diabetesjournals.org/care/article/48/Supplement_1/S283/157559/14-Children-and-Adolescents-Standards-of-Care-in