Last Updated on December 2, 2025 by Bilal Hasdemir

Inguinal hernias are not just for men; they can also affect women. This condition can really change their life. We’re going to look into why and how it happens to women. What are the female inguinal hernia causes? Get the surprising facts about why women get them and the critical, unique risk factors.
An inguinal hernia is when part of the intestine bulges through a weak spot in the belly muscles. It’s not as common in women, but it can be just as serious. So, it’s important to know why it happens to them.
Knowing the causes and risk factors is key to catching it early and treating it right. We’ll talk about how inguinal hernias impact women and what can be done about it.
Key Takeaways
- Inguinal hernias, though more common in men, can significantly affect women’s health.
- Understanding the specific risk factors for women is important for early detection.
- Effective treatment options are available for women with inguinal hernias.
- Awareness of the condition can lead to better health outcomes for women.
- Early diagnosis is key to preventing complications.
Understanding Inguinal Hernias in Women
Inguinal hernias in women are a bit different from those in men. They happen when tissue bulges through a weak spot in the abdominal muscles. This condition is less common in women but can be serious.
Definition and Basic Anatomy
An inguinal hernia occurs when an organ or tissue bulges through a weak spot in the abdominal wall. This weak spot is in the inguinal canal, located in the groin area. In women, this canal is narrower, but hernias can happen due to congenital conditions or acquired weaknesses.
The abdominal wall muscles and the inguinal canal are key to understanding inguinal hernias. The abdominal wall has several layers of muscle and fascia. The inguinal canal is a weak spot where hernias can occur. Knowing this anatomy helps doctors diagnose and treat inguinal hernias in women.
Prevalence in Women vs. Men
Inguinal hernias are more common in men than in women. Studies show men are up to eight times more likely to get them. This is mainly because men’s inguinal canals are wider and have more weaknesses.
Even though women get fewer inguinal hernias, their symptoms and complications can be different. Women may face unique challenges and symptoms, like different types of hernias or more severe complications due to delayed diagnosis.
Anatomical Differences Between Male and Female Inguinal Regions
It’s important to know how men and women’s bodies differ in the inguinal region. This area is where hernias often happen. The inguinal canal is a key structure in the abdominal wall.
Structure of the Inguinal Canal in Women
In women, the inguinal canal is shorter and narrower than in men. It has the round ligament of the uterus, which links the uterus to the labia majora. This ligament is a leftover from when we were growing inside our mothers.
The layers of the abdominal wall, like the transversalis fascia, are key to the canal’s strength. In women, these layers face extra stress, like during pregnancy. This can weaken the inguinal canal.
How Female Anatomy Affects Hernia Development
The female inguinal region’s unique shape affects hernia risk. Women might get different types of hernias because of their anatomy.
The wider pelvis and different muscle setup in women can change how pressure inside the belly is spread. This might raise the risk of hernias. Also, issues like pelvic floor dysfunction can make hernias more likely.
Anatomical Feature | Description | Impact on Hernia Risk |
Shorter Inguinal Canal | Reduced length of the inguinal canal in women | Potentially lower risk of indirect hernias |
Round Ligament | Presence of the round ligament within the inguinal canal | Possible weakening of the posterior wall |
Broader Pelvis | Different pelvic structure in women | Variations in intra-abdominal pressure |
Knowing these differences helps doctors treat hernias in women better. They can give more focused care by understanding the female inguinal region’s unique features.
Types of Hernias Common in Women
It’s important to know about the different hernias women can get. Hernias can affect anyone, but some types are more common in women. This is because of differences in their body structure and how it works.
Direct vs. Indirect Inguinal Hernias
Inguinal hernias are common in both men and women. But, the way they happen is different. Indirect inguinal hernias happen when part of the intestine bulges through a weak spot in the abdominal muscles. This is more common in both genders.
Direct inguinal hernias happen when tissue pushes through a weak spot in the abdominal wall. This type is less common but just as serious.
Knowing the difference between these types is key. Indirect hernias are often present at birth, while direct hernias develop over time due to muscle weakness.
Femoral Hernias: More Common in Women
Femoral hernias are more common in women than in men. They occur just below the inguinal ligament. Femoral hernias are more likely to become trapped or cut off, which can cause serious problems.
The female body’s wider pelvis and larger femoral ring increase the risk of femoral hernias. This makes it easier for parts of the intestine to bulge through the femoral ring.
It’s important to recognize the symptoms of these hernias. Some may not show symptoms, but others can cause a lot of pain or discomfort. Femoral hernias can be hard to spot because they are deep inside the body.
Understanding these differences is key to proper care and treatment. The type of hernia, where it is, and the patient’s health will determine the treatment plan. This could be surgery or other non-surgical methods.
Female Inguinal Hernia Causes: Primary Factors
Inguinal hernias in women come from congenital and acquired factors. Knowing these causes helps in creating better prevention and treatment plans.
Congenital Weakness in Abdominal Wall
Congenital weaknesses in the abdominal wall are a big reason for inguinal hernias in women. These weaknesses are there from birth and can show up later in life. The abdominal wall has muscle and connective tissue layers, and defects in these can lead to hernias.
A common congenital issue is a patent processus vaginalis. This is when the processus vaginalis doesn’t close after birth. It can leave a weak spot where intestines or other tissues can bulge out, causing a hernia.
Acquired Weakness Over Time
Acquired weaknesses in the abdominal wall also cause inguinal hernias in women. These weaknesses come from various factors over a person’s life. Age-related changes, physical strain, and certain medical conditions can weaken the abdominal wall.
For example, as women get older, their connective tissues lose strength and elasticity. Conditions like chronic coughing, obesity, or repetitive heavy lifting can also increase pressure inside the abdomen. This can stress the abdominal wall and lead to hernias.
Understanding both congenital and acquired factors helps healthcare providers create better treatment plans. These plans are tailored to each patient’s needs.
Pregnancy and Its Impact on Hernia Development
Pregnancy brings big changes to the body, including a higher risk of inguinal hernias. The growing fetus puts extra pressure on the belly. This can lead to hernias due to the strain on the muscles.
Increased Abdominal Pressure
The uterus grows and puts more pressure on the belly. This can weaken the muscles and cause hernias. Women with twins or multiple babies face even more risk because of the extra stress.
Hormonal changes during pregnancy also play a part. They can make the connective tissue relax. This can weaken the belly wall and increase the risk of hernias.
Postpartum Complications and Hernia Risk
The time after giving birth can also raise hernia risks. Women with complications like cesarean sections or difficult deliveries are at higher risk. Childbirth can also cause hernias, mainly if there’s a big tear.
“The postpartum period is critical for monitoring and addressing complications. This includes the development of inguinal hernias, which is important for ensuring the health and well-being of new mothers.”
Expert Opinion
Healthcare providers need to know about these risks. Women should also be aware of hernia signs and symptoms during and after pregnancy. Early detection and treatment can help avoid serious problems.
Hormonal Influences on Hernia Formation in Women
Estrogen’s role in connective tissue is key to understanding hernias in women. Hormonal shifts, mainly estrogen changes, can weaken connective tissue. This might lead to hernias.
Estrogen Effects on Connective Tissue
Estrogen can make connective tissue stronger or weaker. It affects collagen, a key part of connective tissue. Collagen disorders can make tissue weak, raising hernia risk.
Estrogen receptors are found in tissues like the abdominal wall. This interaction can change how genes work in tissue repair. This might affect how likely women are to get hernias.
Hormonal Changes Throughout Life
Women’s hormones change a lot, like during pregnancy, menstruation, and menopause. These changes can affect connective tissue and hernia risk.
Pregnancy brings big hormonal shifts, including more estrogen and relaxin. These changes can relax muscles and weaken tissue. This might increase hernia risk.
“Hormonal fluctuations during pregnancy can lead to changes in connective tissue, potentially increasing the risk of hernia formation.”
Hormonal Change | Effect on Connective Tissue | Hernia Risk |
Estrogen Increase | Modulates collagen production | Potential increase |
Relaxin During Pregnancy | Relaxes abdominal muscles | Increased risk |
Menopause | Decrease in estrogen | Potential weakening |
It’s important to understand how hormones affect hernias. Knowing this helps doctors give better care to women at risk. By focusing on hormonal factors, healthcare can be more effective.
Genetic Predisposition to Hernias in Females
Genetic predisposition is a big risk for hernias, mainly in women with a family history. We’ll look at how hereditary factors and collagen disorders increase the chance of inguinal hernias in females.
Hereditary Factors in Hernia Development
Hereditary factors are key in hernia development. Studies show people with a family history of hernias are more likely to get them. This is because genetics can weaken connective tissue, making some more prone to hernias.
Key hereditary factors include:
- A family history of hernias
- Genetic conditions that affect connective tissue
- Inherited traits that influence abdominal wall strength
Collagen Disorders and Tissue Weakness
Collagen disorders are also vital in genetic predisposition to hernias. Collagen is a protein that strengthens connective tissue. Disorders that harm collagen production or quality can weaken tissue, raising hernia risk.
Examples of collagen disorders include:
- Ehlers-Danlos syndrome
- Osteogenesis imperfecta
- Marfan syndrome
These conditions show the role of genetics in hernia development. They stress the need for awareness in those with a family history of such conditions.
Age-Related Factors Contributing to Female Hernias
As women age, their bodies go through changes that make them more likely to get inguinal hernias. We’ll look at how age affects hernias in women.
Changes in Tissue Strength Over Time
One key factor is the natural drop in tissue strength with age. As women get older, their collagen levels go down, and their connective tissue gets weaker. This weakness can raise the risk of hernias because the abdominal wall’s strength is lost. The decrease in tissue strength makes it harder for the body to handle internal pressures, raising the chance of a hernia.
Also, aging often means less physical activity and muscle loss. This weakens the abdominal wall even more. Staying active and keeping a healthy weight can help some, but aging is a risk factor.
Menopause and Its Effects on Abdominal Wall Integrity
Menopause is another big factor in hernias for women. The drop in estrogen levels can cause a loss of collagen and weaken connective tissue. This hormonal change can really hurt the integrity of the abdominal wall, making it more likely to get hernias.
Menopause affects the abdominal wall in many ways. The drop in estrogen weakens tissue and can also change body composition, like adding fat around the belly. This extra belly fat can put more pressure on the abdominal wall, making hernias more likely.
It’s important to understand these age-related factors for prevention and treatment. By knowing the risks of aging and menopause, women can take steps to keep their abdominal health strong and lower their risk of inguinal hernias.
Lifestyle Factors Increasing Hernia Risk in Women
Many lifestyle choices can raise the risk of getting an inguinal hernia in women. These choices are tied to daily habits and health conditions. Knowing and changing these factors can help prevent hernias.
Impact of Obesity and Weight Fluctuations
Being overweight is a big risk for hernias in women. Extra body weight strains the abdominal muscles, making hernias more likely. Also, big weight changes can weaken these muscles, making them more prone to hernias.
Keeping a healthy weight with a good diet and exercise can lower this risk. It’s wise to talk to a healthcare provider about a weight loss plan.
Effects of Heavy Lifting and Physical Strain
Heavy lifting and physical strain also up the risk of hernias. Doing heavy lifting or straining the abdominal muscles can cause hernias over time.
To lessen this risk, use the right lifting methods and take breaks during hard tasks. Doing exercises that strengthen the core can also help.
Chronic Coughing and Increased Abdominal Pressure
Chronic coughing, often from smoking or lung issues, raises abdominal pressure. This increases the risk of hernias.
Managing chronic cough with medical help and avoiding smoking can lower this risk. Good respiratory health habits are also important.
Pelvic Floor Dysfunction and Its Relationship to Hernias
Pelvic floor weakness is a common issue that affects women’s health. The pelvic floor muscles support the abdominal organs. When these muscles are weak, it can cause problems like hernias.
Weakened Pelvic Floor After Childbirth
Childbirth can weaken the pelvic floor muscles. The strain during pregnancy and delivery can cause pelvic floor weakness. This condition is not only uncomfortable but also raises the risk of hernias.
Every woman’s experience with childbirth is different. But, many women face pelvic floor dysfunction after giving birth. It’s important to recognize this common issue.
Connection Between Pelvic Floor Issues and Hernia Development
Pelvic floor issues and hernia development are linked. Weak pelvic floor muscles put more pressure on the abdominal wall. This increases the risk of hernias.
Also, childbirth complications can make hernia risk higher. Women who had tough deliveries or multiple pregnancies face more strain. This can weaken their pelvic floor and abdominal muscles.
It’s key to address pelvic floor issues to avoid complications like hernias. Understanding the link between pelvic floor dysfunction and hernias helps women take care of their health.
Recognizing Symptoms of Inguinal Hernias in Women
It’s key for women to know the signs of inguinal hernias early. This can greatly improve treatment results. Women’s symptoms might be harder to spot because they can be different from men’s.
Common Signs and Symptoms
Women with inguinal hernias might notice a bulge or lump in their groin. They might also feel pain or discomfort in the groin, thigh, or abdomen. Activities like coughing, lifting, or straining can make these symptoms worse.
At times, symptoms can be mild, like a feeling of weakness or slight discomfort. It’s important for women to watch for any changes in their body.
When Symptoms Differ from Those in Men
While symptoms are similar, women are more likely to have femoral hernias. These occur lower in the groin and need different treatment. Women’s symptoms might be mistaken for other issues, which can delay diagnosis.
Complications and When to Seek Medical Attention
Ignoring inguinal hernias can lead to serious problems. These include incarceration and strangulation. Signs that need urgent care include severe pain, nausea, vomiting, fever, and a hernia that turns red, purple, or dark.
It’s vital for women to seek medical help if they notice unusual or ongoing symptoms in their groin. Early diagnosis and treatment can greatly help women with inguinal hernias.
Diagnosis and Medical Assessment
Diagnosing inguinal hernias in women involves a few steps. First, a physical exam is done. Then, imaging studies are used to confirm the diagnosis. We will explain how these steps help in diagnosing inguinal hernias.
Physical Examination Techniques
Starting with a physical exam is key. Healthcare providers check for hernias using different methods. They ask patients to cough or strain to see if a hernia bulges.
They also feel the inguinal area for any tenderness. Experienced clinicians can often spot hernias just by feeling. But, more tests might be needed to be sure or to see how bad it is.
Imaging Studies and Diagnostic Tools
If the exam isn’t clear, imaging studies are used. Ultrasound is a top choice because it’s safe and shows soft tissue well.
In some cases, MRI or CT scans are used. They help confirm the diagnosis and plan the best treatment. These tests show the size of the hernia and any complications.
In summary, diagnosing inguinal hernias in women combines physical exams and imaging studies. This approach helps doctors create a treatment plan that fits each patient’s needs.
Treatment Options for Female Inguinal Hernias
There are many ways to treat inguinal hernias in women. This includes surgery and non-surgical methods. Each person’s situation is different. So, the best treatment is one that fits their needs.
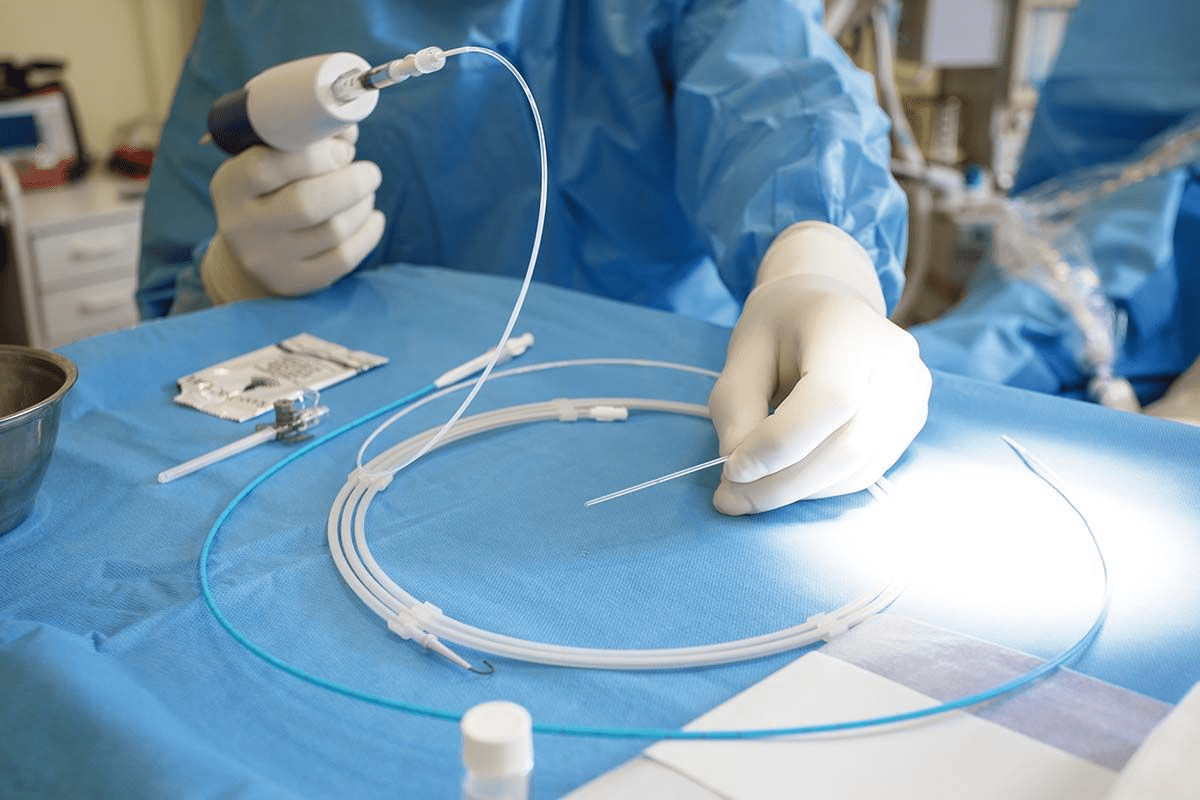
Surgical Approaches Specific to Women
Surgery is often the best choice for women with inguinal hernias. This is true for those with symptoms or big hernias. There are a few surgical options:
- Laparoscopic Repair: This is a small incision method. It uses a laparoscope to fix the hernia.
- Open Repair: This is the traditional way. It involves one big incision to fix the hernia.
- Robotic Repair: This is a laparoscopic method. It uses a robotic system for better precision and control.
These surgeries are effective. Laparoscopic and robotic repairs often mean a faster recovery.
Non-Surgical Management Strategies
Some women might not need surgery. This is true for small, symptom-free hernias or those not fit for surgery. Non-surgical options include:
- Watchful Waiting: Just keeping an eye on the hernia for any changes or symptoms.
- Lifestyle Modifications: Avoiding heavy lifting, staying at a healthy weight, and managing chronic coughing.
- Supportive Garments: Wearing clothes or trusses that offer support to ease discomfort.
Treatment Approach | Description | Benefits |
Laparoscopic Repair | Minimally invasive surgery | Less postoperative pain, quicker recovery |
Open Repair | Traditional surgical method | Effective for complex hernias, straightforward procedure |
Watchful Waiting | Monitoring without immediate surgery | Avoids surgical risks for asymptomatic hernias |
We aim to give each patient the care they need. Whether through surgery or non-surgical methods, our goal is to help women with inguinal hernias get the best results.
Prevention Strategies for Women at Risk
Preventing inguinal hernias is key. Women can lower their risk by making smart lifestyle choices and doing specific exercises. This can greatly reduce their chance of getting a hernia.
Lifestyle Modifications to Reduce Hernia Risk
Changing your lifestyle can help prevent inguinal hernias. Maintaining a healthy weight is important. Extra weight can strain the abdominal muscles, raising hernia risk. Also, avoiding heavy lifting and bending can ease pressure on the abdominal wall.
Quitting smoking is also beneficial. Smoking can cause chronic coughing, which increases abdominal pressure. A high-fiber diet can prevent constipation, a major hernia risk factor. Staying hydrated helps prevent constipation and reduces bowel movement strain.
Exercises to Strengthen Abdominal and Pelvic Floor Muscles
Exercises that strengthen the abdominal and pelvic floor muscles can lower hernia risk. Pelvic floor exercises, such as Kegels, are effective. They strengthen muscles that support the abdominal wall. Gentle core exercises also improve abdominal stability, reducing hernia risk.
Adding low-impact aerobic exercises like walking or swimming is good. These exercises keep you physically fit without straining the abdominal muscles.
By adopting these lifestyle changes and exercises, women at risk can prevent inguinal hernias. They can also keep their abdominal area healthy.
Conclusion
Inguinal hernias in women are a big health issue, often not understood or wrongly diagnosed. We’ve looked at the different parts of inguinal hernias in women. This includes their causes, risk factors, symptoms, how to diagnose them, and treatment options.
Causes of female inguinal hernias include weak spots in the belly wall from birth or developed over time. These can be due to pregnancy, hormonal changes, and lifestyle choices. Knowing these causes helps in preventing and treating them early.
To prevent hernias, women can make lifestyle changes. This includes keeping a healthy weight, not lifting heavy things, and doing exercises to strengthen the belly and pelvic floor muscles. Being aware of the risks can help in getting an early diagnosis and better treatment.
We’ve learned that while less common in women than men, inguinal hernias need a detailed approach for diagnosis and treatment. Understanding the special needs of women with inguinal hernias helps doctors give better care. This improves the health outcomes for female patients.
FAQ
What is an inguinal hernia and how does it occur in women?
An inguinal hernia happens when part of the intestine bulges through a weak spot in the abdominal muscles. This can occur in women due to various reasons. These include congenital weaknesses, pregnancy, and lifestyle factors.
Are inguinal hernias more common in men or women?
Inguinal hernias are more common in men. But women can also get them, mainly due to pregnancy and pelvic floor issues.
How does pregnancy affect the risk of developing an inguinal hernia?
Pregnancy raises the risk of an inguinal hernia due to increased abdominal pressure. Women with multiple pregnancies are at higher risk.
What role do hormonal influences play in hernia formation in women?
Hormonal changes, like the effects of estrogen on connective tissue, can lead to hernias. Hormonal shifts, such as during menopause, can also weaken tissues.
Can genetic predisposition contribute to hernia development in women?
Yes, genetic factors can make tissues weak, raising the risk of hernias in women.
How do lifestyle factors such as obesity and heavy lifting affect hernia risk?
Obesity, heavy lifting, and chronic coughing increase abdominal pressure. This can strain the abdominal wall, raising hernia risk.
What is the connection between pelvic floor dysfunction and hernia development?
Pelvic floor issues, often from childbirth, can weaken muscles. This increases hernia risk. There’s a strong link between pelvic floor problems and hernias.
What are the common signs and symptoms of inguinal hernias in women?
Signs include a bulge in the groin and discomfort, often when coughing, lifting, or bending. Symptoms in women can differ from men’s and may be less typical.
How are inguinal hernias diagnosed in women?
Diagnosis uses physical exams and imaging studies. Accurate diagnosis is key for choosing the right treatment.
What treatment options are available for female inguinal hernias?
Treatments include surgeries tailored for women and non-surgical options. The choice depends on the hernia’s severity, the patient’s health, and other factors.
How can women reduce their risk of developing inguinal hernias?
To prevent hernias, women should maintain a healthy weight, avoid heavy lifting, and do exercises to strengthen abdominal and pelvic floor muscles.
Are there specific exercises that can help prevent inguinal hernias in women?
Yes, exercises like Kegel exercises and certain yoga poses can strengthen muscles. This can help prevent hernias.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4924119/