Last Updated on October 21, 2025 by mcelik

Fibromyalgia affects millions of people worldwide and is characterized by widespread pain and fatigue. Recent studies suggest a strong link between fibromyalgia and autoimmune conditions. This has sparked debate about its classification.
We explore the current understanding of fibromyalgia and its connection to autoimmune diseases. We shed light on whether it’s hereditary and if it’s considered a real disease.
Fibromyalgia is a complex chronic condition. It causes widespread pain, fatigue, and cognitive issues. These problems greatly affect the quality of life for those who have it.
Fibromyalgia is a chronic disorder with various symptoms. These include widespread musculoskeletal pain, fatigue, sleep, memory, and mood issues. The severity of these symptoms can vary, impacting daily life.
The main symptoms are:
Fibromyalgia affects a significant number of people. It is estimated to impact around 4 million adults in the United States. The condition can greatly affect daily life, impacting not just the individual but also their family and social networks.
The high prevalence of fibromyalgia shows the need for awareness and understanding. Recognizing symptoms and their impact can help in better management and support for those affected.
The classification of fibromyalgia has changed over time. It was once seen as a rheumatic condition but is now recognized as a neurological disorder. Understanding its historical classification is key to grasping its current status and how it differs from other conditions, including autoimmune diseases.
In the past, fibromyalgia was often misunderstood. This led to challenges in diagnosis and treatment. Recognizing it as a neurological condition has opened up new research and management avenues.
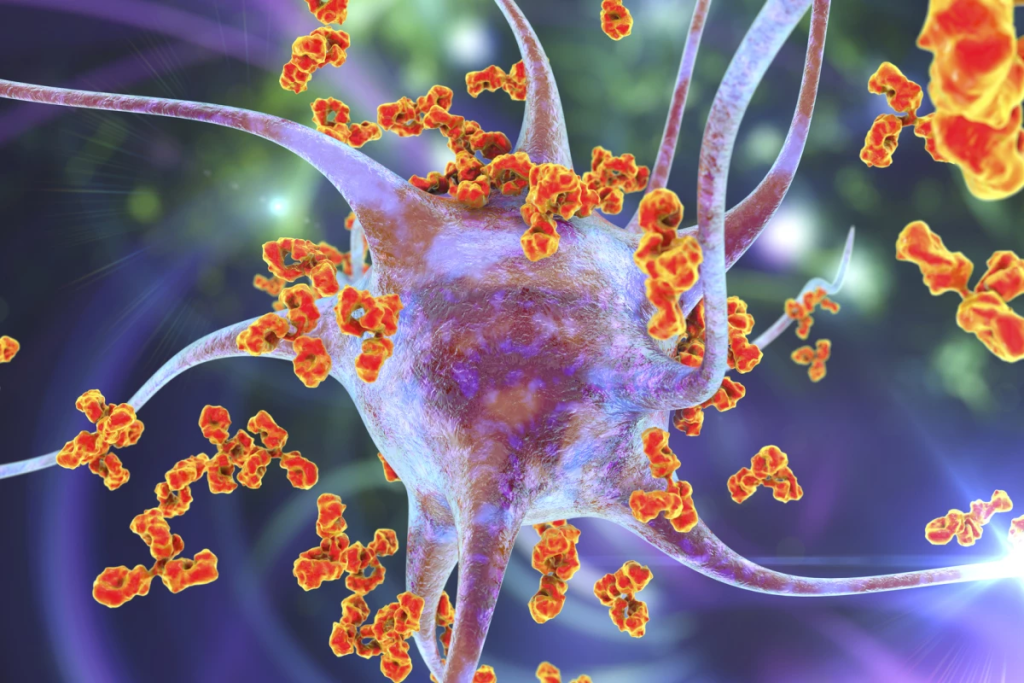
To understand autoimmune diseases, we need to know what they are and how they work. These diseases happen when the body’s immune system attacks its own tissues. This leads to various health problems.
Autoimmune diseases happen when the immune system can’t tell the difference between self and non-self. It attacks the body’s own cells and tissues. This causes inflammation, damage, and symptoms that vary by disease and affected area.
Autoimmune diseases share some key traits. These include:
Knowing these traits helps doctors diagnose and treat autoimmune conditions better.

Many diseases are known to be autoimmune. Examples include:
These examples show how autoimmune diseases can affect the body in different ways. They highlight the need for accurate diagnosis and treatment.
The question of whether fibromyalgia is an autoimmune disease is debated. Different studies show different results. It’s important to look at all sides to understand fibromyalgia.
Some studies link fibromyalgia to immune system problems, common in autoimmune diseases. Key points include:
Despite some evidence, many argue fibromyalgia is not an autoimmune disease. Key points include:
Today, scientists don’t see fibromyalgia as a traditional autoimmune disease. Yet, they believe immune system issues might contribute to it. Fibromyalgia’s causes are complex, involving the brain, hormones, and possibly the immune system.
As research grows, we’ll learn more about fibromyalgia. This could lead to better treatments for this challenging condition.
Recent studies suggest fibromyalgia is a neurological disorder, not just chronic pain. This new understanding is key for research into its causes and treatments.
Fibromyalgia involves altered pain processing, heightened sensitivity, and neurochemical changes. These factors are central to the condition.
Central sensitization is a key feature of fibromyalgia. It makes the central nervous system overly sensitive to stimuli. This sensitivity amplifies pain signals, causing widespread musculoskeletal pain.
Research shows fibromyalgia patients have different pain processing pathways. These changes affect how the brain handles pain signals, leading to chronic pain.
Neuroimaging has shed light on fibromyalgia’s neurological basis. Techniques like fMRI have shown brain activity differences between patients and healthy individuals.
These findings indicate changes in brain areas involved in pain processing. The insula and prefrontal cortex are affected. These changes are linked to abnormal pain perception in fibromyalgia.
Neurotransmitter imbalances are also key in fibromyalgia. Studies have found changes in serotonin and dopamine levels in patients.
These neurotransmitters are vital for pain and mood regulation. Their imbalance contributes to fibromyalgia’s chronic pain and mood issues.
Seeing fibromyalgia as a neurological disorder helps us understand its complex nature. This understanding is essential for developing effective treatments that target its neurological roots.
Research shows fibromyalgia and the immune system are closely linked. This connection is key to understanding fibromyalgia symptoms. It’s clear that problems with the immune system play a big role.
Studies found fibromyalgia patients have abnormal inflammatory markers. These markers show how the body’s immune system is working. High levels of these markers mean the immune system is always on, leading to pain and discomfort.
Some important findings are:
Cytokines are proteins that control the immune system. In fibromyalgia, cytokine levels are off balance. This imbalance affects how the immune system works.
The importance of cytokine problems is huge. They can:
Fibromyalgia isn’t an autoimmune disease, but the immune system is not working right. This wrong immune response causes chronic inflammation. It’s a big part of why fibromyalgia symptoms happen.
Grasping this part of fibromyalgia is key. It helps in finding new treatments. These treatments aim to fix the immune system problems, helping patients feel better.
The link between fibromyalgia and autoimmune diseases is complex. Studies show people with fibromyalgia often have other autoimmune diseases. This makes diagnosis and treatment harder.
Research has found several autoimmune diseases that often go hand in hand with fibromyalgia. These include:
These diseases share symptoms with fibromyalgia. This makes it tough to diagnose and treat both conditions well.
Fibromyalgia and autoimmune diseases have similar symptoms. These include chronic pain, fatigue, and brain fog. This similarity can cause delays or wrong diagnoses if not checked carefully.
For example, someone with fibromyalgia might also get lupus. This could add symptoms like skin rashes and swollen joints. Doctors need to watch for these extra conditions.
Having other autoimmune diseases can really affect a person’s life with fibromyalgia. It’s key to understand these conditions to manage fibromyalgia better.
By seeing how fibromyalgia and autoimmune diseases interact, doctors can give better care. They can meet both the physical and emotional needs of their patients.
Fibromyalgia and lupus are two chronic conditions that share similar symptoms. This makes it hard to tell them apart. Both can really affect a person’s life, so knowing their differences is key to managing them well.
Both fibromyalgia and lupus can cause pain, tiredness, and brain fog. But lupus is a disease that attacks the body’s organs, like the kidneys and skin. Fibromyalgia mainly causes widespread pain and sensitivity to pain.
The main differences in symptoms are:
Even though there are differences, the symptoms can overlap. This makes it important to do a detailed check-up to diagnose correctly.
Diagnosing lupus and fibromyalgia requires different methods. Lupus diagnosis uses a mix of clinical findings and lab tests, like:
Fibromyalgia diagnosis, on the other hand, relies more on clinical judgment, using:
Getting the right diagnosis is essential for the right treatment.
Lupus treatment aims to control the immune system with drugs like corticosteroids and DMARDs. Fibromyalgia treatment focuses on managing symptoms with:
Knowing how to treat each condition differently is important for doctors to provide the best care.
Doctors are debating if chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is an autoimmune condition. We need to look at how CFS/ME and fibromyalgia are similar and different. This helps us understand these conditions better.
CFS/ME is a serious condition that makes you feel extremely tired all the time. This tiredness doesn’t get better with rest. Doctors diagnose it based on what the patient says and by ruling out other possible causes. The main signs include:
Fibromyalgia and CFS/ME share many symptoms like chronic pain, fatigue, and brain fog. Both are more common in women and often happen together. This has led to discussions about whether they are different conditions or just different sides of the same coin.
Whether CFS/ME is an autoimmune disease is a topic of debate. It shares some traits with autoimmune diseases, like ongoing inflammation and immune system problems. But, it doesn’t fit the traditional definition of an autoimmune disease because there’s no clear proof of autoantibodies or direct immune damage.
Studies have found that the immune system in CFS/ME patients is not working right. This includes issues with cytokines and immune cells. But, whether this is an autoimmune process is something scientists are trying to figure out.
Some important points in this discussion are:
As research keeps going, we’ll learn more about CFS/ME. We’ll see how it fits into the world of autoimmune diseases and other conditions. For now, CFS/ME is a complex condition that doesn’t fit neatly into one category.
Research shows a link between fibromyalgia and genetics. This means hereditary factors might play a big role in getting the condition. Learning about its genetic roots helps us understand its causes and treatments better.
Studies found that fibromyalgia often runs in families. Family members of those with fibromyalgia are more likely to get it. This suggests a genetic link. It’s not just about the environment, as certain genetic markers increase the risk.
Genetic markers linked to fibromyalgia include genes for pain and neurotransmitters. Research found polymorphisms in serotonin and dopamine genes. These are key for pain control, showing how genetics can influence fibromyalgia risk.
These markers help us understand fibromyalgia’s causes. They also guide treatment. By matching treatments to genetic profiles, care can be more effective.
Genetics are important, but the environment also plays a part. Stress, infections, and physical trauma can start fibromyalgia in those at risk. Knowing how genes and the environment interact helps in prevention and early treatment.
Understanding the mix of genetics and environment helps explain why some get fibromyalgia and others don’t. This is true even in the same family.
Fibromyalgia’s status as a real disease has long been debated. Patients have struggled to get a proper diagnosis and treatment. This is due to doubts about the condition’s legitimacy.
Fibromyalgia has faced skepticism for decades. This skepticism comes from a lack of understanding about its causes. In the past, some thought it was a psychosomatic disorder, not a real physical condition.
But, as research has grown, our understanding of fibromyalgia has too. Studies have shown it’s a complex condition. It involves changes in pain processing and neurotransmitter imbalances.
Recent studies have found solid evidence for fibromyalgia’s legitimacy. Neuroimaging studies have shown brain activity differences in those with fibromyalgia. Research has also found biomarkers like certain cytokines and changes in BDNF.
These findings prove fibromyalgia is not just about being sensitive or stressed. It has a biological basis. These markers help legitimize fibromyalgia, paving the way for better diagnosis and treatment.
Dismissing fibromyalgia can harm patients. It can lead to delayed diagnosis and inadequate treatment. Patients may feel misunderstood, which can worsen their symptoms and quality of life.
Healthcare providers must approach fibromyalgia with compassion and understanding. Recognizing its legitimacy is key to improving patient outcomes. This can greatly enhance the lives of those with fibromyalgia.
New research is changing how we see fibromyalgia. It’s moving us away from old views. Studies are now diving into the disease’s complex nature. This is key for better treatments and tests.
2024 research has made big strides in understanding fibromyalgia. It shows that fibromyalgia makes our nervous system too sensitive. This is why people with fibromyalgia feel constant pain and discomfort.
Another area of study is neuroinflammation in fibromyalgia. It seems that inflammation plays a part in the symptoms. Finding out how it works is important for new treatments.
Scientists are searching for reliable tests for fibromyalgia. They’ve found possible markers in inflammatory cytokines and neurotransmitter abnormalities. These could make diagnosing fibromyalgia more precise and straightforward.
| Biomarker | Description | Potential Impact |
| Inflammatory Cytokines | Proteins that promote inflammation | Could indicate presence of neuroinflammation |
| Neurotransmitter Abnormalities | Imbalances in neurotransmitters like serotonin and dopamine | May help explain pain processing alterations |
| MicroRNA Expression | Changes in microRNA levels related to pain regulation | Could serve as a diagnostic or prognostic marker |
Fibromyalgia’s classification is changing. As we learn more, we see it as a multifactorial disorder. It involves the brain, immune system, and mind.
This new view will change how we treat fibromyalgia. We’ll focus more on personalized medicine and multidisciplinary care. This way, treatments will be more effective and tailored to each person.
The link between fibromyalgia and Hashimoto’s thyroiditis is a hot topic in medical research. It’s clear that these two conditions are more than just coincidental. They have a deep connection.
Research shows a strong link between fibromyalgia and Hashimoto’s thyroiditis. Many people with fibromyalgia also have thyroid issues. This suggests a possible connection between the two, but the exact reason is not yet known.
“The high prevalence of thyroid disorders in patients with fibromyalgia highlights the need for thorough testing,” a study notes. This is important because the symptoms of both conditions can be similar. This makes it hard to tell them apart.
Fibromyalgia and Hashimoto’s thyroiditis share symptoms like fatigue and muscle pain. This makes diagnosing them tricky. One condition’s symptoms can hide or worsen the other’s, leading to wrong or late diagnoses.
For example, fibromyalgia’s pain and fatigue might be mistaken for hypothyroidism from Hashimoto’s. Or vice versa. Doctors must do detailed tests and look at a patient’s full medical history to get it right.
Key diagnostic challenges include:
Dealing with fibromyalgia and Hashimoto’s thyroiditis together needs a careful approach. Treatment plans must take into account both conditions.
For instance, thyroid hormone therapy for Hashimoto’s might need to be adjusted to avoid making fibromyalgia worse. On the other hand, treatments for fibromyalgia might need to be tailored based on the patient’s thyroid health.
“A team effort from rheumatologists, endocrinologists, and primary care doctors is key to caring for these patients,” clinical guidelines say.
Understanding the connection between fibromyalgia and Hashimoto’s thyroiditis helps doctors create better treatment plans. These plans can meet the specific needs of patients with both conditions.
Diagnosing fibromyalgia needs a detailed approach. This includes clinical checks and ruling out other conditions. We’ll look at the current criteria, excluding autoimmune diseases, and the use of lab tests.
Fibromyalgia diagnosis focuses on clinical signs. These include widespread pain for over three months and symptoms like fatigue and sleep issues. The American College of Rheumatology (ACR) sets criteria for diagnosis. It’s key to spot the symptoms and see how they affect daily life.
Fibromyalgia can mimic autoimmune diseases like rheumatoid arthritis and lupus. So, it’s vital to rule out these conditions. This is done through medical history, physical exams, and lab tests. Getting the diagnosis right is essential for proper treatment.
Lab tests help in diagnosing fibromyalgia by ruling out other conditions. There’s no specific test for fibromyalgia. But, tests like complete blood counts and thyroid function tests can help. It’s important to understand these tests in the context of the patient’s symptoms.
In conclusion, diagnosing fibromyalgia is a detailed process. By using the right criteria, ruling out other conditions, and using lab tests wisely, we can accurately diagnose and manage fibromyalgia. This improves patient outcomes.
Managing fibromyalgia often means using a mix of treatments. Each plan is made just for the person. It includes medicines and other ways to help, like therapy and lifestyle changes.
Medicines for fibromyalgia aim to ease pain, help sleep, and tackle feelings of sadness and worry. Some common ones are:
It’s important to remember that these medicines might not work for everyone. How well they work can vary a lot.
There are also non-medical ways to manage fibromyalgia. These include:
These methods can be adjusted to fit what each person needs and likes, making them more effective.
Fibromyalgia treatment is different from that for autoimmune diseases. Autoimmune diseases, like rheumatoid arthritis, often need medicines to stop inflammation and protect tissues. But fibromyalgia treatment focuses on easing symptoms and improving life quality.
| Treatment Aspect | Fibromyalgia | Autoimmune Diseases |
| Primary Focus | Symptom management (pain, sleep, fatigue) | Immunosuppression and inflammation control |
| Common Medications | Pain relievers, antidepressants, anti-seizure drugs | DMARDs, biologics, corticosteroids |
| Lifestyle Recommendations | Exercise, stress management, sleep hygiene | Similar, with additional focus on preventing infections |
It’s key for doctors to know these differences. This helps them create the right treatment plans for fibromyalgia patients, alone or with autoimmune diseases.
As we learn more about fibromyalgia, it’s clear that a full treatment plan is needed to manage it well.
“The management of fibromyalgia requires a multidisciplinary approach, incorporating both pharmacological and non-pharmacological strategies to address the multifaceted nature of the condition.”
” Fibromyalgia Expert
Living with fibromyalgia is tough, affecting both body and mind. It’s clear that managing this condition needs a wide range of strategies.
Patients struggle to find their way through the healthcare system. Many feel like they’re being passed from doctor to doctor without getting help. This shows the need for a better care path.
Doctors should take a holistic view of fibromyalgia. This means looking at both physical and mental health. A team of specialists could help create personalized plans.
Dealing with fibromyalgia requires many strategies. These include medicine, therapy, lifestyle changes, and support groups. Mixing these approaches helps manage symptoms better.
Support groups are key for emotional and practical help. As one patient said, “Meeting others who get it has saved my life.”
Seeing fibromyalgia as a real disease matters a lot to patients. It validates their experiences and opens doors for new treatments.
Understanding fibromyalgia leads to better care. It means doctors can focus on what each patient needs. As research grows, patients will get better care and a better life.
By listening to patients and learning more about fibromyalgia, we can improve care. We aim for a future where those with this condition get the support they need.
Fibromyalgia is a complex condition that can’t be labeled easily. It involves many factors like the brain, immune system, and genes. This makes it hard to understand and treat.
Getting to know fibromyalgia means looking at it from different angles. Some think it’s linked to autoimmune diseases, but others see it as unique. This shows we need a deeper understanding of fibromyalgia.
Research is helping us learn more about fibromyalgia. It’s uncovering how it works and what signs to look for. As we learn more, we can find better ways to help people with fibromyalgia. By accepting its complexity, we can improve care and treatment for those affected.
No, fibromyalgia is not seen as an autoimmune disease. Yet, it shares some traits with them, like immune system issues and other health problems.
Main symptoms include widespread muscle pain, tiredness, brain fog, and tender spots. These can change in how bad they are and how they affect daily life.
Doctors diagnose fibromyalgia by checking symptoms, medical history, and lab tests. This helps rule out other diseases, like autoimmune ones.
Yes, fibromyalgia can happen with autoimmune diseases like lupus, rheumatoid arthritis, and Hashimoto’s thyroiditis. This can make diagnosis harder because symptoms are similar.
Debates exist over whether CFS/ME is an autoimmune disease. It shares some symptoms with fibromyalgia, making it hard to tell them apart.
Yes, genetics play a role in fibromyalgia. Family history and certain genetic markers can increase the risk, mainly in those with a family history.
Treatment for fibromyalgia is a mix of medicine and non-medical methods. This includes managing pain, exercising, and cognitive-behavioral therapy.
Yes, fibromyalgia is a real medical condition. It’s backed by scientific findings, like changes in pain processing and brain scans, despite past doubts.
Fibromyalgia and Hashimoto’s thyroiditis often happen together. They share symptoms like tiredness and pain, making diagnosis and treatment tricky.
Fibromyalgia can greatly affect daily life. It causes ongoing pain, tiredness, and brain fog. These can hurt relationships, work, and overall happiness.
Our understanding of fibromyalgia’s causes involves the nervous, immune, and hormonal systems. Research is ongoing to better understand it.
Yes, researchers are looking into new biomarkers. These include inflammation markers and brain scans to improve diagnosis and understanding of fibromyalgia.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!