Last Updated on November 13, 2025 by
Anemia affects over 1.6 billion people globally. Quick and effective treatment is key to their health and happiness. Finding out why and how severe anemia is is very important. What is the first line treatment anemia? Learn the crucial and most powerful steps doctors take to correct low blood cell counts initially.
For iron deficiency anemia, taking oral iron is usually the first step. It works well over 80% of the time if people stick to it and don’t have trouble absorbing it. We’ll look into how oral iron helps in treating anemia.
Starting with oral iron is often the best choice. Iron salts are the top picks for supplements. Studies and global advice back this method, highlighting the need for good anemia management guidelines.
To manage anemia well, knowing its types, causes, and how to diagnose it is key. Anemia is not just one condition. It’s a group of disorders where there are not enough red blood cells or hemoglobin. This makes it hard for tissues to get enough oxygen.
Anemia can be divided into several types based on its causes and signs. The most common types are:
Anemia can be caused by many things. Some common causes include:
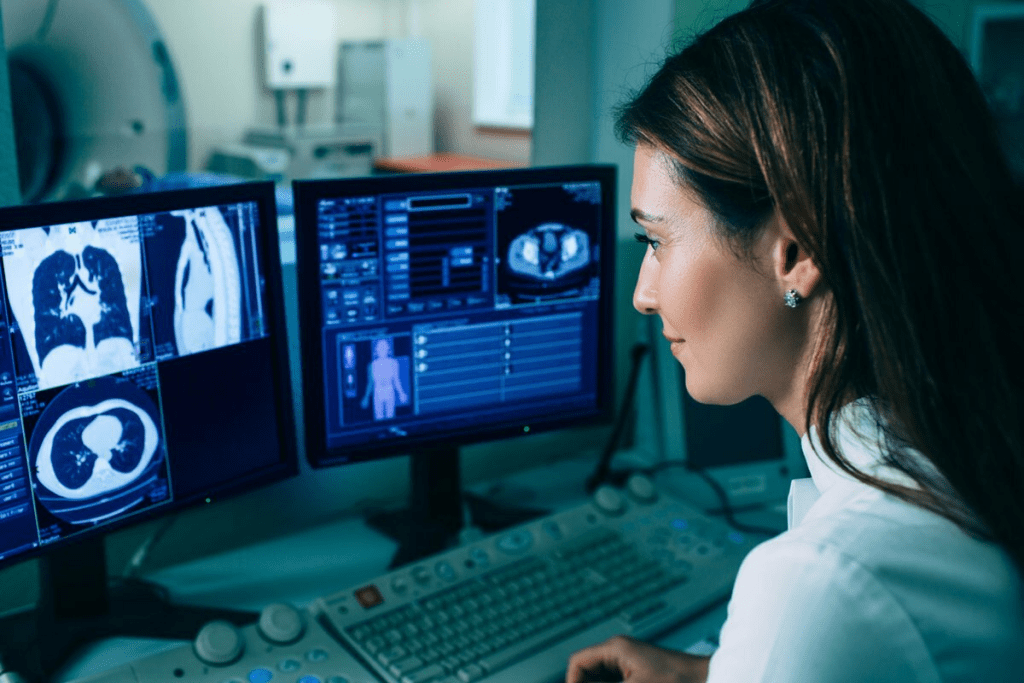
Diagnosing anemia involves several steps. These include clinical checks, lab tests, and sometimes more tests. Important steps include:
Knowing why someone has anemia is key to treating it right. By figuring out the type and cause, doctors can create a treatment plan that really helps. This improves how well patients do.
The first line of treatment for anemia patients usually receives is oral iron replacement. For those with iron deficiency anemia, oral iron therapy is often the first choice. This method uses iron salts to treat the condition. We’ll look at the benefits and possible side effects of oral iron therapy.
Oral iron therapy is suggested for mild to moderate cases of iron deficiency anemia. It’s for those who can take oral supplements easily. The National Institutes of Health says it works by adding iron and boosting hemoglobin levels.
There are different oral iron supplements, like ferrous sulfate, ferrous gluconate, and ferrous fumarate. Ferrous sulfate is often chosen because it’s effective and affordable. Ferrous gluconate and ferrous fumarate are used for those who can’t handle ferrous sulfate well.

The amount of iron supplement needed varies based on the severity of the deficiency. A typical dose is 30-120 mg of elemental iron daily. Taking it on an empty stomach helps absorption, but food can lessen stomach side effects.
People on oral iron therapy usually see better hemoglobin levels in 2-3 weeks. The count of new red blood cells, or reticulocytes, goes up in 7-10 days. It’s key to keep taking the treatment for months to fully refill iron stores.
Managing anemia is more than just treating it. It’s also about dealing with the side effects of oral iron therapy. As healthcare providers, we guide patients through this process. We make sure they know how important it is to stick with the treatment and how to handle any bad effects.
Oral iron therapy works well but can cause stomach problems like nausea, constipation, and diarrhea. To lessen these issues, we suggest taking iron with food. This might slightly lower how much iron is absorbed. Sometimes, changing to a different iron type or adjusting the dose can help.
What you eat affects how well your body absorbs iron. We tell patients to eat foods high in vitamin C with iron-rich foods to boost absorption. But, foods with polyphenols (like tea and coffee), calcium, and certain phytates can block iron absorption. It’s best to eat these foods apart from iron supplements.
It’s important to regularly check how well oral iron therapy is working. We look at hemoglobin levels, reticulocyte count, and iron stores through serum ferritin levels. Symptoms and hemoglobin levels usually start to get better within a few weeks of treatment.
By managing side effects, making smart food choices, and keeping an eye on how treatment is going, we can make oral iron therapy better for patients with anemia. This improves their quality of life and treatment results.
For those who don’t respond to or can’t take oral iron, new hope is found in alternative treatments. When oral iron doesn’t work, doctors look for other ways to treat anemia.
Intravenous iron therapy is a good option for those who can’t take oral iron or haven’t seen results. It puts iron straight into the blood, skipping the stomach. Intravenous iron anemia therapy helps those with chronic diseases or need iron quickly.
This method works better and has fewer side effects than oral iron for some. It can raise hemoglobin levels and cut down on blood transfusions.
For severe anemia, blood transfusion might be needed. Blood transfusion anemia indications include severe anemia with heart problems or when quick anemia correction is needed.
Blood transfusions quickly increase red blood cells. This helps symptoms lessen and improves oxygen to tissues.
Patients with megaloblastic anemia due to vitamin B12 or folate deficiency need supplements. Vitamin B12 and folate supplementation treat the cause, boosting red blood cell production.
“Vitamin B12 deficiency is a common cause of megaloblastic anemia, and supplementation can lead to significant improvements in patient outcomes.”
Pregnant women, children, and those with chronic diseases need special anemia treatments. For example, pregnant women might need more iron because of their increased needs.
It’s important to tailor treatments for these groups. We must ensure the chosen therapy is safe and works well for each patient.
Managing anemia well means tackling its root cause. Knowing the different types and their causes helps us pick the best treatment. Oral iron is often the first choice, but other options are needed if it doesn’t work.
It’s key to treat the cause of anemia to get the best results. We need to follow guidelines and tailor treatment for each patient. This way, we can ease symptoms and improve health outcomes.
By sticking to a clear treatment plan and handling side effects, we can make anemia treatment better. Our aim is to give top-notch care and support to those with anemia.
The first step in treating iron deficiency anemia is oral iron replacement therapy. It works well if the patient takes it as directed and doesn’t have issues with absorbing it.
To find the cause of anemia, doctors use lab tests, physical exams, and look at the patient’s medical history. This helps them choose the right treatment.
Oral iron therapy can cause stomach problems. But, there are ways to make these side effects less bothersome. This helps patients stick with their treatment.
Doctors suggest intravenous iron therapy when oral iron doesn’t work or causes problems. It’s also good for those with severe anemia or who can’t absorb iron well.
Vitamin B12 and folate are key in treating anemia caused by their lack. They are often used with other treatments to get the best results.
Doctors check how well treatment is working by looking at lab results. They check hemoglobin levels and iron stores. This helps them adjust the treatment if needed.
Blood transfusions are needed for severe anemia, when symptoms are bad or there’s a risk of serious problems. They quickly raise the red blood cell count.
Eating foods high in vitamin C and avoiding tea and coffee can help with iron absorption. This makes oral iron therapy more effective.
For special groups like pregnant women or those with chronic diseases, treatment plans are made just for them. They consider their unique needs and health situation.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!