Last Updated on November 26, 2025 by Bilal Hasdemir
Anal fistulas are a tough condition to treat. Liv Hospital uses a patient-focused method. They treat anal fistulas with fistulotomy surgery and seton placement.
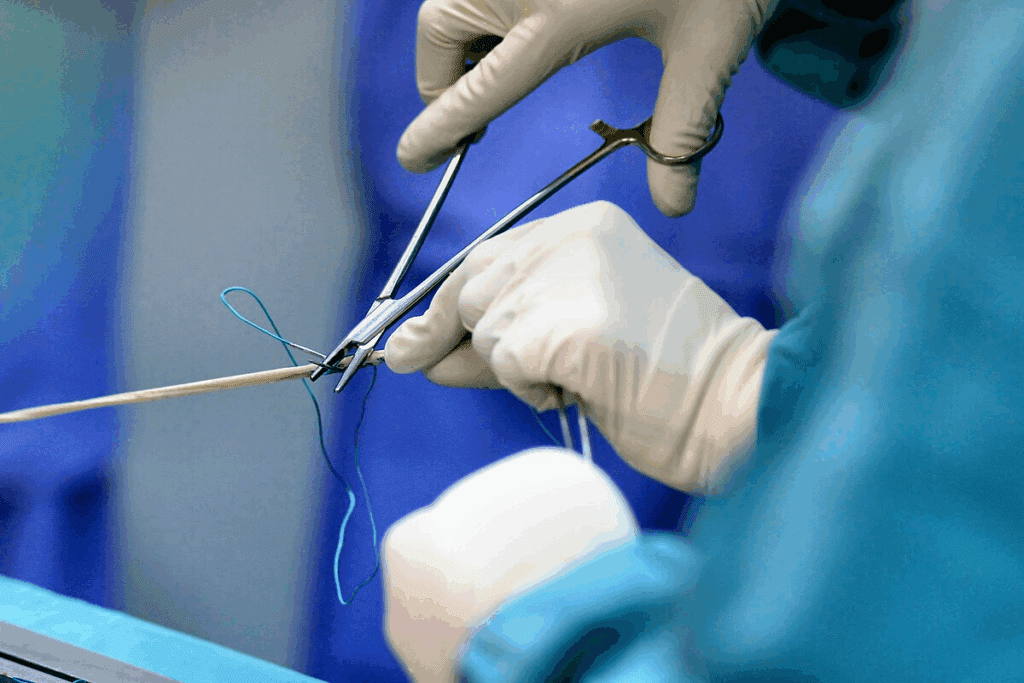
This surgery puts a seton suture in to help with drainage and healing. Knowing the steps of this procedure helps patients understand its complexity. It also shows the need for a skilled team.
Using the latest surgical methods and evidence-based protocols is key. This ensures patients get top-notch care. As we look into this guide, it’s clear how seton placement is vital for treatment success.

To treat anal and perianal fistulas well, knowing their anatomy and types is key. Anal fistulas are abnormal tunnels from the anal canal to the skin. They often start from an infection or inflammation.
The anal canal is wrapped by two muscles: the internal and external anal sphincters. Fistulas can go through these muscles, making treatment harder. It’s important to know how the fistula tract relates to these muscles for surgery planning.
An anal fistula usually begins with an infection in the anal glands. This can turn into an abscess. If not drained right or keeps coming back, it might become a fistula.
Fistulas are sorted by where they are in relation to the anal sphincters. The Parks classification is widely used. It groups fistulas into:
| Type of Fistula | Description | Treatment Complexity |
| Intersphincteric | Between internal and external sphincters | Low |
| Transsphincteric | Crosses both sphincters | Moderate to High |
| Suprasphincteric | Above the sphincters | High |
| Extrasphincteric | Outside the sphincters | Very High |
Surgery is often needed for fistulas that don’t get better with simple treatments. This includes symptoms that won’t go away, abscesses that keep coming back, and complex fistula paths. Surgery aims to close the fistula without harming sphincter function or causing incontinence.
Choosing surgery depends on the fistula’s complexity, the patient’s health, and the risks and benefits of the surgery.

Before surgery, a detailed assessment is key to a patient’s success. It helps spot risks and plan for them. This ensures the best results for the patient.
Knowing a patient’s health history is vital. It shows their overall health and past surgeries. A physical exam checks the anal area for the fistula’s details.
Imaging tests are important for planning. MRI or ultrasound help map the fistula and find any abscesses.
Common tests include:
Assessing risks is about checking the patient’s health and the fistula’s complexity. Choosing the right surgery depends on these factors.
Important factors are:
Getting informed consent is essential. Patients need to know about the surgery, risks, and recovery.
Education should include:
The success of fistulotomy surgery with seton placement depends on the right tools and materials. Choosing the right ones is key for a good outcome and recovery.
Fistulotomy surgery needs specific tools for precision and safety. These include:
Table: Essential Surgical Instruments for Fistulotomy
| Instrument | Purpose |
| Probes | Identifying and exploring the fistula tract |
| Surgical Scissors | Incision and dissection |
| Forceps | Handling tissue and seton materials |
| Retractors | Maintaining clear visibility of the surgical site |
Seton devices come in threads, bands, and tubes. Each has its own use and benefits. The right one depends on the fistula’s type and complexity.
The fistula’s complexity guides the choice of seton material. More complex fistulas need stronger materials. Simpler ones might use less invasive options.
“The selection of seton material should be tailored to the individual patient’s condition and the specific characteristics of the fistula.” – Surgical Guidelines
Preparing the operating field is key. It involves cleaning, disinfecting, and draping the area. This step reduces infection risk and ensures a clean environment for surgery.
By picking the right tools and materials, surgeons can greatly improve fistulotomy surgery results.
Before fistulotomy surgery, it’s key to prepare well and choose the right anesthesia. Good preparation can lower risks and improve results.
Getting the bowel ready is a big part of fistula surgery prep. It helps avoid infections. Patients often eat only clear liquids the day before and might take bowel prep meds.
Bowel prep methods can differ based on the doctor and patient. Doctors might use laxatives or enemas to empty the bowel.
How the patient is positioned is important for reaching the fistula. They might lie on their stomach or sit with their legs up, depending on where the fistula is.
Draping is done to keep things clean and clear. The area around the anus is cleaned and covered to prevent infection.
The type of anesthesia depends on the fistula’s complexity and the patient’s health. Choices include local anesthesia with sedation, regional anesthesia, or general anesthesia.
| Anesthesia Type | Description | Usage Scenario |
| Local Anesthesia with Sedation | Numbing the specific area with sedation for relaxation | Simple fistulas, minor procedures |
| Regional Anesthesia | Numbing a larger area, such as below the waist | More complex fistulas, patient comfort |
| General Anesthesia | Complete unconsciousness | Complex cases, patient anxiety |
Using antibiotics before surgery is a big decision. It’s based on the risk of infection. For fistulotomy, antibiotics might be given to certain patients.
Deciding on antibiotics is important. It depends on the patient’s health and the fistula’s complexity.
Fistulotomy surgery starts with a detailed initial assessment. This step is key to figuring out the best way to fix the fistula. It involves several important parts that help the surgeon plan the surgery.
Examination under anesthesia is a vital part of fistulotomy surgery. It lets the surgeon check the fistula without the patient feeling pain. With the patient relaxed, the surgeon can get a clear view of the fistula’s details and its position.
Finding both the external and internal openings of the fistula is essential. The external opening is easy to see, but the internal one might need special tools or scans to find. Knowing where these openings are helps the surgeon plan the surgery.
The surgeon gently probes the fistula to see its path and any connections to nearby tissues. This step is important for choosing the right surgery method and avoiding problems.
Checking if the fistula touches the anal sphincter is a key part of the initial check. The surgeon needs to know how much of the sphincter is involved to plan the surgery. This helps decide if a seton is needed and how much of the fistula to cut.
The first steps of fistulotomy surgery are all about careful planning. By examining the fistula under anesthesia, finding the openings, probing, and checking the sphincter, surgeons can create a treatment plan that fits the patient’s needs.
Fistulotomy surgery can greatly improve patient outcomes when done right. It needs a deep understanding of the surgical techniques involved.
The first step is making a precise incision to reach the fistula tract. Incision and drainage techniques are key to opening and draining the fistula. This helps prevent abscesses.
The surgeon must find the fistula’s external and internal openings for the incision. Probing the fistula tract helps understand its path and complexity.
After accessing the fistula tract, the next step is fistula tract excision. This can be done in different ways, like laying open the tract or removing it entirely. The choice depends on the tract’s complexity and the surgeon’s preference.
Managing simple and complex fistulas is different. Simple fistulas are easier to treat with a direct fistulotomy. But, complex fistulas need a more detailed approach, often with setons.
After removing the fistula tract, curettage and debridement are done. This removes any infected tissue left behind. It helps in healing and lowers the chance of the fistula coming back.
By following this step-by-step method, surgeons can make sure fistulotomy surgery is done well. This reduces complications and improves patient results.
The seton placement technique is key in fistulotomy surgery. It ensures effective drainage and lowers the risk of incontinence. This method is used for complex fistulas, helping them heal gradually and reducing complications.
Choosing between a loose seton and a cutting seton depends on the fistula’s complexity and the patient’s health. Loose setons are for complex or high fistulas, aiding in drainage and healing. Cutting setons are for simpler fistulas, aiming to cut through tissue for healing.
The seton threading procedure has several steps:
Securing the seton is vital for it to work right. It’s usually done with a knot or a locking mechanism. The seton’s tension is adjusted, with loose setons needing less tension than cutting setons.
The seton’s tension is adjusted based on its type. For loose setons, the tension is low for drainage and healing. For cutting setons, the tension is set to help cut through tissue gradually.
| Seton Type | Tension Adjustment | Treatment Goal |
| Loose Seton | Minimal Tension | Drainage and Healing |
| Cutting Seton | Adjusted Tension | Gradual Cutting through Tissue |
Effective wound management is key to avoiding problems after fistulotomy surgery. The right care right after surgery can greatly help the healing process. It also affects how well the patient does overall.
Stopping bleeding is a major step in caring for patients after fistulotomy surgery. Hemostatic agents like oxidized cellulose or absorbable gelatin sponge can be used to stop bleeding. Sometimes, suturing or ligating the bleeding vessels is needed.
Wound packing is a big part of postoperative care. It helps manage drainage and aids in healing. Materials like gauze, calcium alginate, or foam dressings can be used. The right material depends on how much drainage there is and the wound’s needs.
Choosing between partial closure and open healing depends on several things. Partial closure means closing part of the wound but leaving the rest open. Open healing lets the wound heal from the bottom up without closure.
Managing pain well is important for patient comfort and recovery. Multimodal analgesia, which uses different pain medicines, is effective. This can include opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetics.
By using these strategies for wound management and postoperative care, healthcare providers can improve patient outcomes. They can also lower the chance of complications after fistulotomy surgery.
Managing setons long-term is key to healing after fistulotomy. Regular check-ups are needed to adjust the seton and track healing.
Adjusting the seton is a big part of long-term care. How often it needs adjusting depends on the seton type and the patient’s healing. Usually, adjustments happen every few weeks.
| Type of Seton | Adjustment Frequency | Average Replacement Time |
| Loose Seton | Every 2-3 weeks | 6-8 weeks |
| Cutting Seton | Every 1-2 weeks | 3-6 weeks |
Good wound care is vital for healing and avoiding infections. Patients need to know how to keep the wound clean and dry.
“Gentle wound care with saline irrigation and dressing changes is key to avoiding problems and helping the wound heal.”
— Expert Opinion
Patients with setons should not do heavy lifting, bending, or hard activities. This helps avoid discomfort and complications. When to go back to normal activities depends on how well the patient heals.
Regular check-ups are important to watch healing and adjust treatment if needed. The schedule for follow-ups can change based on the case’s complexity.
By sticking to a detailed follow-up and management plan, patients can get the best results from their fistulotomy surgery.
Fistulotomy surgery with seton placement is often effective. Yet, it can lead to various complications. It’s vital to manage these issues well to ensure the best results for patients.
After fistulotomy surgery, patients might face infections, incontinence, or fistula recurrence. To tackle these problems, several strategies are available:
Table: Complications and Management Strategies
| Complication | Management Strategy |
| Infection | Antibiotic treatment |
| Incontinence | Biofeedback therapy |
| Recurrence | Revision surgery |
Preventing fistula recurrence is key. To do this, several steps are taken:
At times, other treatments are explored. These include:
Reoperation might be needed if the first surgery fails. This is true for:
Managing complications and exploring alternative treatments are essential. They help improve outcomes for patients undergoing fistulotomy surgery with seton placement.
Fistulotomy surgery with seton placement is a top choice for treating anal fistulas. It offers a good chance of healing and lowers the risk of complications. This is true when the surgery is done right.
The procedure for fistula surgery is carefully planned. It starts with checking the patient before surgery and goes to caring for them after. This ensures the best results for patients.
A seton placement summary shows how key it is to use the right method. It’s important to place the seton correctly and adjust its tightness as needed.
When perianal fistula surgery works well, it can heal the fistulotomy scar. This helps the patient live a better life.
Understanding fistulotomy surgery well and following the best practices helps surgeons get great results. It also lowers the chance of the problem coming back.
A seton suture helps with drainage and healing in fistulotomy surgery. It keeps the fistula open, helping it close over time. This reduces the chance of problems.
To place a seton drain, a suture or material is threaded through the fistula. It’s then secured and the tension is adjusted. This is based on what the treatment aims to achieve.
There are thread, band, and tube setons used in fistulotomy surgery. Each type has its own benefits. They are chosen based on the fistula’s complexity and the treatment goals.
The seton tension is adjusted to meet treatment goals. This might be to help with drainage or to close the fistula slowly. Adjustments are made during follow-up visits to ensure healing and avoid complications.
Complications can include the fistula coming back, infection, incontinence, and anal stenosis. These can be managed with proper care, follow-up, and other treatment options.
Wound care involves keeping the area clean and using sitz baths. Following specific instructions from the healthcare provider is also important. This helps with healing and prevents complications.
After surgery, you might need to avoid heavy lifting, bending, or strenuous activities. Following a bowel management regimen can also help. This reduces discomfort and aids in healing.
Follow-up assessments are usually scheduled every few weeks. They help monitor healing, adjust the seton tension, and address any issues or concerns.
Reoperation might be needed if the fistula doesn’t close or if complications like abscesses or infections occur. It’s also considered if the treatment doesn’t meet the desired outcomes. In these cases, other treatments might be tried.
A seton can be removed when the fistula has healed or as decided by the healthcare provider. This is usually after a certain period or when the treatment goals are met.
Khalil, H. M., et al. (2021). Biliary leakage following cholecystectomy: A prospective population study. Journal of Research in Medical and Dental Science, 9(5), 289-296. Retrieved from https://www.jrmds.in/articles/biliary-leakage-following-cholecystectomy-a-prospective-population-study-84919.html
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!